Quick Answer: Untreated chlamydia in college students can silently lead to pelvic inflammatory disease, chronic pelvic pain, infertility, and complications in future pregnancies, even without symptoms.
Why College Students Are Especially at Risk
College is a strange paradox: the years when you’re finally in control of your choices, but often lacking the tools to fully understand their consequences. For many students, sexual health takes a backseat to deadlines, roommate drama, and trying to make it to 8 a.m. lectures. Testing seems like something to “get around to.” Pain gets chalked up to a rough hookup or stress. When the symptoms are invisible, it’s easy to assume there’s nothing wrong.
For people like Jordan, a 22-year-old senior, the warning signs were subtle. “I didn’t even know guys could have chlamydia and not feel anything,” he admitted during a telehealth follow-up after finally testing. “I only got tested because my ex told me she had it. I probably had it for months.”
This delay isn’t unusual. In one campus-based study, fewer than 20% of students who tested positive for chlamydia had reported any symptoms. And without symptoms to flag something wrong, the infection quietly travels upward in the body, especially in people with uteruses, potentially leading to complications like PID or scarring in the fallopian tubes. The irony? Catching chlamydia early is usually as simple as a quick urine test and a round of antibiotics.
The Quiet Fallout: What Untreated Chlamydia Can Actually Do
Chlamydia is known for its stealth. You can carry it for weeks or months without knowing. But invisibility doesn’t mean inactivity. In fact, untreated infections trigger slow, internal inflammation. Here’s what can happen when chlamydia is left to run its course in the body without treatment:
In people with uteruses, the biggest risk is the spread to the upper reproductive tract. Once it reaches the cervix and beyond, the infection can cause inflammation in the uterus, fallopian tubes, and ovaries, a condition known as pelvic inflammatory disease (PID). PID is a big reason why young women can't get pregnant. An untreated infection can permanently damage the fallopian tubes, making it more likely for an ectopic pregnancy (a life-threatening condition where a fertilized egg implants outside the uterus) to happen or making it impossible to get pregnant at all.
In people with penises, untreated chlamydia can lead to epididymitis, painful inflammation in the tube that carries sperm. Though rare, it can also cause reactive arthritis or affect sperm quality. And just like with those assigned female at birth, many cases go unnoticed until a partner gets diagnosed or until discomfort becomes severe enough to trigger testing.
It’s also worth noting the psychological toll. Delayed diagnoses often lead to a spiral of guilt, fear, and shame, especially if a relationship is involved. One missed test can turn into a breakup, a confrontation, or an unplanned journey into the complexities of fertility treatment later in life. Most of this is preventable, and yet it keeps happening in dorms and college apartments across the country.

People are also reading: You Didn’t Cheat. You Still Got HPV. Here’s Why That Happens
Chlamydia’s Invisible Timeline: How Long Is “Too Long” to Wait?
There’s no perfect answer to how long is too long. Some people go months, or longer, without realizing they’re infected. Others catch it early by chance during routine screening. The reality is, once chlamydia is in the body and multiplying, it can start damaging tissue within a matter of weeks, especially if reinfection happens or the immune system is already compromised.
The progression of the infection isn’t always linear. Some people may harbor chlamydia for 6 to 12 months without noticeable symptoms. Others develop early complications in a matter of weeks. This makes routine testing critical, especially after new partners or unprotected sex. Waiting until something feels wrong is a gamble with high stakes.
| Time Since Infection | Possible Progression Without Treatment |
|---|---|
| 1–2 Weeks | Often asymptomatic; bacteria begin colonizing cervical or urethral tissue |
| 3–6 Weeks | Inflammation may spread to uterus or epididymis; symptoms may start subtly |
| 2–3 Months | Risk of pelvic inflammatory disease increases; long-term damage begins |
| 6 Months+ | Tubal scarring, infertility risk, increased risk of ectopic pregnancy or chronic pain |
Figure 1. General progression timeline of untreated chlamydia in college-aged individuals. Individual timelines can vary.
Does It Just Go Away on Its Own?
There’s a dangerous rumor that some STDs clear up on their own. And while it’s technically true that a small percentage of people might “self-resolve” chlamydia over time, relying on this is reckless and dangerous. The majority of untreated infections persist and cause irreversible damage long before they fade. More importantly, even if symptoms subside, or never appear, you’re still contagious.
In fact, being asymptomatic is one of the reasons chlamydia spreads so easily on college campuses. People assume they’re fine. They move on to new partners. They don’t use condoms every time. And the cycle continues. This is why the CDC recommends yearly screening for all sexually active women under 25 and men who have sex with men. But college culture often lags behind medical advice. Routine testing isn’t part of the rhythm of campus life, yet.
Testing doesn’t just protect you. It’s an act of care for everyone you’re connected to. And it’s far easier than most people assume. With options ranging from campus clinics to fully private home test kits, getting tested is no longer the ordeal it once was.
Check Your STD Status in Minutes
Test at Home with Remedium6-in-1 STD Rapid Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $119.00 $294.00
For all 6 tests
The Ripple Effect: Chlamydia and Fertility in Your 20s
Ask most 19-year-olds if they’re thinking about fertility, and you’ll get a shrug. But what you do now, before you’re even thinking about kids, can shape your reproductive options in the future. Chlamydia is the leading preventable cause of infertility in women. And you don’t need to have had multiple partners or dramatic symptoms for it to do damage.
Take Anjali, who found out she had blocked fallopian tubes during a routine fertility workup at age 29. “I remember crying, trying to figure out how this could’ve happened,” she recalled. “I had one chlamydia infection in college. I didn’t even know what PID was at the time. I thought the antibiotics had fixed it. But I guess the damage had already been done.”
While one round of antibiotics can clear an active infection, the body doesn’t always heal perfectly, especially if the diagnosis was delayed. Scar tissue from inflammation can linger, silently closing doors you didn’t even know were open.
In people with penises, there’s growing evidence that chlamydia may reduce sperm motility or affect semen quality over time. Though less widely discussed, it’s another piece of the reproductive puzzle. And in couples where only one partner was diagnosed, both may end up facing fertility questions they never expected.
When You Don’t Know You’re Spreading It
The hardest part about untreated chlamydia isn’t just the damage it causes to the person who has it. It’s what happens next, when someone passes it on without even realizing they’re infected. For many college students, there’s no moment of recklessness, no obvious “I messed up” night. It’s often the routine hookups, the low-stakes relationships, the “we used protection… mostly” situations that become the source.
Eric, 21, had only ever been with two partners. He used condoms but admitted there were times it didn’t happen. “She told me she got chlamydia and must’ve gotten it from me,” he said, still processing the guilt. “But I never felt sick. I got tested after, and yeah, I was positive too. I had no clue.”
Chlamydia doesn’t need symptoms to spread. It can pass through vaginal, anal, and sometimes even oral sex. It can linger between partners for months, quietly infecting others. And unless someone breaks the silence, gets tested, tells their partners, or experiences symptoms that prompt a check, it keeps moving.
This is why regular screening matters even when you’re in a monogamous relationship. Many students pick up the infection in the early days of dating, long before they’ve discussed exclusivity or history. Without testing, there’s no way to tell who had it first, and no benefit in assigning blame. What matters is stopping the cycle before it loops again.
Why “I Don’t Feel Anything” Is the Most Dangerous Symptom
Here’s the truth: feeling “fine” isn’t a green light when it comes to STDs. In fact, the most common symptom of chlamydia in college students is… no symptom at all.
The lack of pain, discharge, itching, or burning doesn’t mean the infection isn’t active. It just means your body hasn’t thrown up red flags, or you’ve normalized the symptoms. That low-grade cramp? Could be ovulation. A little testicle ache after a night out? Maybe you sat weird. Our brains are master rationalizers, especially when we’re busy, embarrassed, or emotionally invested in someone.
Medical providers see this every week. Students coming in with “weird spotting” that’s been happening for months. People who thought they had a yeast infection and self-treated with OTC creams. Guys who noticed a burning sensation and figured it was dehydration or stress. By the time a diagnosis is made, the infection has often had time to spread.
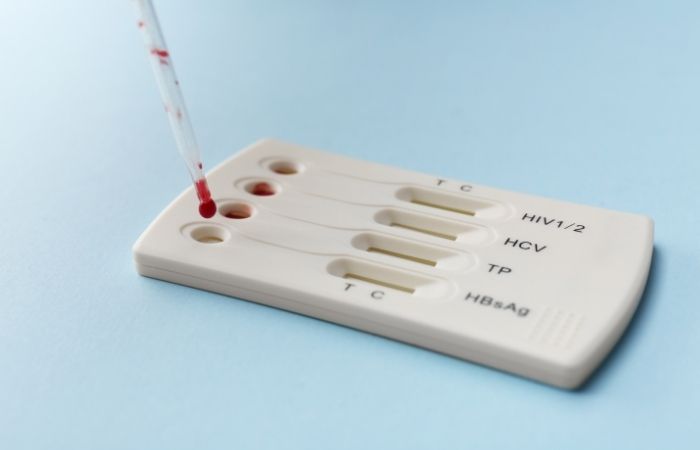
This is why many college health centers encourage routine screenings, even if you feel fine. Most offer urine-based NAAT tests (nucleic acid amplification tests), which are highly accurate and non-invasive. Some also offer self-swab options or referrals to local clinics. And for students who don’t feel comfortable going in, at-home test kits offer discreet, fast alternatives without ever stepping foot in an office.
| Symptom Presence | What It Actually Means |
|---|---|
| No Symptoms | Infection may still be active and causing internal damage; most common scenario in college students |
| Mild Symptoms | Often mistaken for UTIs, yeast infections, or period issues; easily ignored |
| Clear Symptoms | May prompt earlier testing but often delayed due to shame or misinterpretation |
Figure 2. Symptom presence doesn’t reflect severity or damage. Chlamydia is often silent but still harmful.
College Health Myths That Delay Diagnosis
Let’s be honest: campus culture isn’t exactly set up for proactive sexual health. Despite wellness initiatives, many students still rely on secondhand info, late-night Reddit threads, or whatever their roommate remembers from high school sex ed. Misinformation is rampant, and it fuels delays in testing and treatment.
Some of the most common myths include:
“If I don’t have discharge or pain, I’m fine.” “I used a condom once or twice, so I’m probably okay.” “You can’t get STDs from oral or quick sex.” “If they didn’t say anything, they must be clean.” “Testing is only for people who sleep around.”
All of these are false, and all of them allow chlamydia to thrive on college campuses. It’s not about being reckless. It’s about not knowing what you don’t know. And unfortunately, the body doesn’t wait for your class schedule or your comfort level to start reacting. Damage happens whether you’re ready to acknowledge it or not.
This is why education matters. But more than that, access matters. At-home test kits can help close the gap for students who feel too anxious, too busy, or too ashamed to go in person. These kits are discreet and often come in plain boxes. You can take them to your dorm room, apartment, or anywhere else where you can be alone.
If your head keeps spinning, peace of mind is one test away. Order a discreet chlamydia test kit and stop wondering.
Testing Options: Clinics vs. At-Home Kits
One of the reasons students delay testing is the logistics. “I don’t have a car.” “It takes forever to get an appointment.” “What if someone sees me walk in?” The good news is: testing has evolved. You don’t need to brave a waiting room or explain your sex life to a stranger if you’re not ready. There are multiple options that fit different comfort levels and schedules.
Campus health centers are often the fastest route. Many offer free or low-cost STI screening, especially during designated awareness months or wellness weeks. They may use urine-based NAAT testing, which doesn’t require a pelvic exam and has high sensitivity for chlamydia detection.
Walk-in options are often available at urgent care clinics or Planned Parenthood locations, and the results are usually quick. But not everyone feels comfortable navigating these spaces, especially in smaller towns or among friend circles where privacy feels limited.
That’s where at-home tests come in. You collect your sample yourself, usually urine or a vaginal swab, and either read the results on a rapid test strip or mail it to a lab for analysis. These tests are highly accurate when used correctly and can be a lifeline for those managing stigma, anxiety, or logistical barriers.
What matters isn’t where you test. It’s that you test. And if you test positive, getting treated quickly is crucial, not just for your health, but for anyone you’ve been intimate with. Chlamydia doesn’t mean you’re dirty. It doesn’t mean you’re irresponsible. It means you’re human. And like everyone else, you deserve to be cared for, not judged.
Retesting After Treatment: Why One Negative Isn’t Always Enough
You got treated. You took the antibiotics. You feel fine. So that’s it, right? Not exactly. With chlamydia, retesting is a key part of staying healthy, and many students don’t realize that a one-and-done approach isn’t always enough.
Here’s the problem: reinfection is extremely common, especially in the college age group. Studies show that as many as 20% of people treated for chlamydia will get it again within a few months. This usually happens because a partner wasn’t treated at the same time, or because someone resumed sex before the antibiotics had fully cleared the bacteria.
The CDC recommends retesting three months after treatment, even if you’re in a monogamous relationship. If you’re not sure when you were infected, or if your partner wasn’t treated, you may need to test again sooner. And if symptoms return or worsen, don’t wait. Pain, discharge, or spotting after treatment may signal persistent or repeat infection.
Retesting isn’t just about clearing your own system. It’s about protecting future partners, preventing long-term damage, and keeping yourself informed. There’s no shame in being proactive. You don’t get extra points for pretending it never happened.
If you're unsure whether it's time to retest, or you're in a new relationship after treatment, now’s a good time. This combo test kit checks for multiple infections at once, because chlamydia rarely travels alone.
People are also reading: HPV Throat Cancer Rates Are Exploding in the South. Here's Why.
The Risk of Reinfection: It’s Not About Promiscuity, It’s About Awareness
Reinfection isn’t a moral failing. It’s a medical reality. And yet, college students who test positive a second time often carry unnecessary shame. What they don’t realize is how easily it can happen, even when you think you’ve been careful.
One common scenario? You and a partner both test positive and get treated, but only one of you waits the full 7 days before having sex again. Another? You assume a new partner is “clean” because they said they were tested last year. Or maybe you just didn’t bring it up because the vibe was casual, and it felt awkward to ask.
None of these make you reckless. They make you human. College is often the first time people are navigating sexual autonomy, and that means figuring out communication, boundaries, and safer sex in real-time. But chlamydia doesn’t care how serious the relationship was. It doesn’t care how nice someone was to you. It only needs one opportunity.
This is why test timing matters. It’s also why talking matters, more than most of us were ever taught. Asking about testing history isn’t accusatory. It’s responsible. And it’s becoming more normalized, especially as at-home testing makes it easier to check before things get complicated.
Telling a Partner: Scripts for the Worst Conversation You’ll Ever Have (That Isn’t Actually That Bad)
For many students, the worst part of testing positive isn’t the infection, it’s telling someone else. The idea of calling or texting an ex, a hookup, or a current partner feels mortifying. But it doesn’t have to be.
If you’ve ever said “Hey, just wanted to let you know I tested positive for chlamydia. I’m getting treated and you should probably get tested too,” then congratulations, you’ve just done more for public health than a dozen posters in your dorm hallway.
Partner notification is hard. But it’s also respectful. And most of the time, it goes better than you think. Many students report that their partners were understanding, even grateful, once the initial awkwardness passed. In some cases, both people tested positive and started treatment together. In others, it led to conversations about safer sex, honesty, and getting on the same page moving forward.
You don’t have to do it alone. Many campuses offer anonymous partner notification services through student health centers or local clinics. Some at-home test providers even include discreet notification tools. What matters is making sure the person knows, so they can get tested, treated, and avoid passing it on to someone else.
This isn’t about calling people out. It’s about calling them in. And doing that takes courage.
Check Your STD Status in Minutes
Test at Home with Remedium8-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $149.00 $392.00
For all 8 tests
After Treatment: What Recovery Actually Looks Like
Most of the time, treatment for chlamydia is straightforward. A single dose of antibiotics (often azithromycin or doxycycline), followed by 7 days of no sex to let the meds work. But that’s only part of the story.
Physically, you may not feel much change, especially if you didn’t have symptoms to begin with. Emotionally, though, it can feel like a rollercoaster. Relief, shame, guilt, anger, fear, sometimes all in one afternoon. And for people dealing with complications like PID or fertility concerns, that recovery extends far beyond a week of pills.
Some students report lingering pelvic pain, irregular bleeding, or emotional triggers long after treatment ends. These may require follow-up with a gynecologist, urologist, or even a therapist. Others find the experience reshapes how they think about their bodies, their boundaries, and what they want from sexual relationships moving forward.
There’s no one “right” way to feel after a diagnosis. But what you should never feel is ashamed for taking care of yourself. Testing and treating isn’t something to whisper about. It’s something to normalize, and even celebrate. Because every time you get tested, you protect not just your future, but someone else’s too.
FAQs
1. Can chlamydia really just go away without treatment?
Kind of like that toxic situationship? It might fade... but not without consequences. While a very small number of cases might self-resolve, most don’t, and the infection doesn’t need symptoms to do damage. Even if your body fights it off, it could leave behind scarring, inflammation, or future fertility problems you won’t see coming. Bottom line? Don’t risk it. It’s way easier to test and treat than to wonder what’s happening silently inside you.
2. How long can you have chlamydia without knowing?
Longer than you’d think, and definitely longer than most people realize. You could carry chlamydia for weeks, months, even a year or more and feel totally fine. A lot of college students find out by accident, like during a routine checkup or when a partner tests positive. If you’ve ever thought “I feel fine, so I must be fine,” this is your sign to rethink that logic. Silence doesn’t mean safety.
3. Can chlamydia actually make you infertile?
Unfortunately, yes. It’s not scare tactics, it’s science. When chlamydia goes untreated, especially in people with uteruses, it can move up into the reproductive system and cause pelvic inflammatory disease (PID). That’s where scarring starts, and even one untreated infection can block fallopian tubes or lead to ectopic pregnancies. Fertility issues down the line? They often start here, in the silence. And you won’t know it’s happening until much later.
4. If I don’t have symptoms, how could I be contagious?
Because chlamydia doesn’t need an announcement to spread. Think of it like a quiet hitchhiker, no fireworks, no big signs, just an invisible guest passing from partner to partner. You can absolutely pass it on through vaginal, anal, or oral sex even if you feel totally normal. That’s why testing is a form of respect, for yourself and the people you’re intimate with.
5. What does treatment actually look like?
Honestly? Chill. Most chlamydia cases are cleared with a simple antibiotic, either one-time azithromycin or a week of doxycycline. That’s it. No scary procedures, no hospital visits. Just make sure you follow the instructions and wait at least seven days before having sex again, even if you feel fine. Trust the timeline, it’s not worth rushing.
6. Do guys get symptoms too, or is this just a “girl” thing?
Guys get it too, and plenty never know. Some will feel burning when they pee, notice discharge, or have testicle pain. Others feel nothing at all. One student described it as “just a weird pressure I ignored until my partner tested positive.” So no, it’s not just a “girl problem”, chlamydia doesn’t discriminate. It just hides well in everyone.
7. Can I get it from oral sex? What about just messing around?
Yep. Chlamydia can spread through oral sex, though it’s less common than other types of transmission. You don’t need deep penetration or a full-blown hookup for transmission to happen. Skin contact, shared toys, even fingers can play a role if bacteria are present. If it’s sexual contact of any kind, testing still applies.
8. How soon after sex should I get tested?
Hold off just a bit, testing immediately after exposure isn’t super reliable. Your body needs time to build up enough of the bacteria to show up on a test. Aim for 7 to 14 days after the hookup. If you test early and it’s negative, retest later to be sure. Especially if you feel off, or your partner tests positive after the fact.
9. Do I really have to tell my ex or past hookup?
Yeah... and we know that’s the hardest part. But it’s also the most important. You don’t have to give a full TED Talk. A simple “Hey, just wanted to let you know I tested positive for chlamydia. You should probably get tested too” goes a long way. Some services even let you notify anonymously. You’re not starting drama, you’re helping someone avoid long-term damage. That’s not messy. That’s mature.
10. Are at-home STD tests reliable?
When you get them from a trusted provider? Absolutely. At-home chlamydia test kits are highly accurate, especially NAAT-based ones, and they give you privacy, control, and speed. If going to the clinic feels too intense (or too public), this is a safe, doctor-trusted way to get answers on your own terms. Just make sure you're ordering from a legitimate provider, like STD Rapid Test Kits, and follow the instructions carefully.
You Deserve Answers, Not Assumptions
Here’s the truth they don’t always tell you during freshman orientation: STDs like chlamydia aren’t rare, shameful, or proof you did something wrong. They’re infections, treatable ones, and they spread most easily in silence. Untreated chlamydia doesn’t just fade away. It lingers, complicates, and sometimes scars futures you haven’t even imagined yet.
If you’re reading this because something feels off, or because someone you care about tested positive, don’t wait and wonder. Testing is quick, private, and in your control. This at-home combo test kit checks for the most common STDs discreetly and quickly. You owe yourself that clarity.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate.
Sources
1. CDC – Chlamydia: Basic Fact Sheet
2. Planned Parenthood – Chlamydia Information
3. Chlamydia trachomatis - Symptoms and Causes (Mayo Clinic)
4. Chlamydia Fact Sheet (World Health Organization)
5. Chlamydial Infections - STI Treatment Guidelines (CDC)
6. Pelvic Inflammatory Disease (PID) - STI Treatment Guidelines (CDC)
7. Chlamydia Overview - NCBI Bookshelf (NIH)
8. Reproductive Tract Complication Risks After Chlamydia - NIH PMC
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: Kelsey Vaughn, RN, MPH | Last medically reviewed: January 2026
This article is meant to give you information, not to give you medical advice.