Quick Answer: Delaware has a high rate of chlamydia because more people are getting tested, there are still cases that don't show symptoms, and there are problems with getting tested quickly. At-home kits can help fill in the gaps in testing by giving people private and easy ways to get tested.
The Numbers Behind Delaware’s Ranking
Chlamydia is the most common bacterial STI in the US, and Delaware is no different. In 2023, the state had 5,703 new cases, a lot of which were in young adults aged 15 to 24. Experts say that silent transmission is still a big problem, even though more people are getting tested. Chlamydia can go unnoticed for months or even years because up to 70% of women and 50% of men with the disease don't have any symptoms.
The rise from 19th in 2020 to 12th in 2023 shows that reporting systems have gotten better, but prevention strategies still have holes in them. A public health nurse in Delaware says, "We're finding more cases because we're looking harder." "But we're also seeing infections come back, which means we're not breaking the cycle."

People are also reading: How Chlamydia Can Affect Babies When the Mother is Infected
Why Chlamydia Is So Common, And So Underestimated
There’s no single reason Delaware has moved up the chlamydia rankings. Instead, it’s a combination of factors: high rates in younger populations, overlapping sexual networks in small communities, and social stigma that keeps people from getting tested regularly. In rural areas, lack of nearby clinics can delay diagnosis. In urban centers, even when clinics are available, fear of judgment or privacy concerns may keep people away.
Public health experts also point out that Chlamydia often travels with other STIs, and once you’ve had it, your risk of reinfection is higher. Without consistent partner testing and treatment, infections bounce back and forth in a cycle that’s hard to break.
The Role of Delaware’s Geography and Demographics
Delaware’s small size means its communities are more interconnected, socially and sexually, than in many larger states. This can speed up the spread of any communicable disease, especially one as silent as Chlamydia. College towns, military bases, and seasonal tourism all add layers of mobility and interaction that fuel transmission.
Data shows the highest chlamydia rates in New Castle County, which includes Wilmington, and in Sussex County, a rural area with limited sexual health resources. This mix of high-density and underserved populations makes it tricky to apply a one-size-fits-all prevention strategy.
“I Didn’t Think I Needed to Get Tested”
Kara, 22, grew up in southern Delaware and had been with the same partner for over a year. “I figured we were safe,” she says. “We never talked about testing, it just didn’t come up.” When she went in for a routine physical, her doctor suggested an STI screen. The result? Positive for Chlamydia. “I was shocked. I had zero symptoms. If my doctor hadn’t pushed, I never would have known.”
“It made me realize testing should be like dental check-ups, just something you do.”
Order Now $33.99 $49.00 Check Your STD Status in Minutes
Test at Home with Remedium
Chlamydia Test Kit




Delaware’s Public Health Response: Progress and Gaps
Delaware's Division of Public Health has stepped up its screening efforts, focusing on high-risk groups like teens, young adults, and communities that don't get enough health care. Mobile clinics, health centers in schools, and partnerships with Planned Parenthood have all made it easier to get tests. The state is also part of the CDC's STD Prevention Program, which pays for outreach and education efforts.
But there are still gaps, even with these efforts. Mobile testing only goes to some rural areas a few times a year. It can be hard for shift workers to get screened because clinics aren't always open. And even though the CDC says that sexually active women under 25 should get tested for chlamydia every year, not all healthcare providers do.
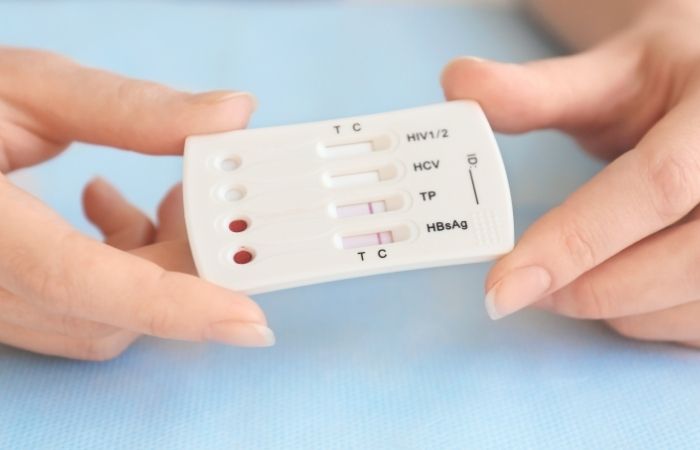
How Home Testing Kits Fit Into the Solution
At-home STD testing kits have the potential to close many of Delaware’s screening gaps. They allow people to collect samples privately, mail them to a certified lab, and get results online, often within days. This removes the need to travel, take time off work, or face possible stigma in public clinics.
For a condition like Chlamydia, which can cause long-term complications like infertility if left untreated, early detection is critical. Home testing can turn “I’ll get around to it” into “I’ve already sent my sample,” especially for those in rural Sussex County or busy parts of New Castle County.
Why Routine Screening Matters More Than Ever
Chlamydia’s ability to hide in the body without symptoms makes routine screening essential. In Delaware, where young adults make up a large portion of new cases, testing once a year, or more often if you have new or multiple partners, is one of the simplest ways to protect yourself and your partners.
Routine screening also helps break the cycle of reinfection. When both partners get tested and treated at the same time, the infection stops bouncing back and forth. This is where home kits can be a game changer, making partner testing more convenient and less awkward.
People are also reading: How Gonorrhea Can Cause Arthritis
Delaware vs. the Nation: What “High” Really Means
When headlines say Delaware is a “top state” for Chlamydia, context matters. Nationally, chlamydia remains the most reported bacterial STI, and younger people, especially ages 15–24, carry the heaviest burden. Delaware’s rates sit above the U.S. average, which signals two truths at once: the state is finding more infections (good surveillance), and enough people are still getting infected to keep numbers up (room for prevention). For local health teams, that means doubling down on consistent screening and fast treatment, not just awareness posters.
Another nuance: small states can swing more dramatically year to year. A few hundred additional cases, or a campus outbreak that drives more people to test, can nudge rankings quickly. That’s why the trend line, not just a single year, should guide strategy. Delaware’s multi‑year climb tells us this isn’t a blip; it’s a system asking for easier, more routine testing and better partner treatment.
Who’s Most Affected, and Why
Across Delaware, the majority of reported Chlamydia cases show up in people under 25. Many infections are asymptomatic, so people don’t seek care until a partner discloses a positive test or a routine exam catches it. Gender and access play a role too: women are screened more often during reproductive healthcare visits, which can uncover silent infections; men, who may visit clinics less frequently, can remain undiagnosed and continue transmitting without realizing it.
Social networks amplify risk. In tight‑knit communities, college dorms, service industry circles, military bases, partners may overlap within a short time frame. Add in barriers like transportation, clinic hours, or fear of being recognized at the local health center, and it’s easy to see why infections persist. This is precisely the gap that discreet home kits can fill.
From “I’ll Do It Later” to “I Already Tested”: How Home Kits Change Behavior
Behavioral friction is the silent enemy of public health. Even highly motivated people can put off clinic visits because of work schedules, childcare, or anxiety. An at‑home test reduces friction to a single, private task: collect, mail, check results. Many users complete testing within 48–72 hours of deciding they should; that speed matters for breaking chains of transmission.
- Privacy: No waiting rooms, no awkward check‑ins, no running into your neighbor.
- Speed: Clear instructions help you collect a sample correctly the first time.
- Follow‑through: App or email reminders nudge you to open, swab, and send, closing the intention–action gap.
Think of home kits as a complement to clinics, not a replacement. They’re the on‑ramp that gets more people tested more often, and that consistency is what drives community rates down over time.
Check Your STD Status in Minutes
Test at Home with Remedium7-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $129.00 $343.00
For all 7 tests
Exactly How a Chlamydia Home Kit Works (Step‑by‑Step)
Curious what the process actually looks like? Here’s a straightforward walk‑through so there are no surprises.
- Order & Delivery: Choose a discreet option that fits your needs, single‑infection or combo. Packages arrive in plain wrapping.
- Collect: Follow the illustrated guide. Most chlamydia tests use a urine sample or a gentle swab (vaginal, rectal, or throat if indicated by sexual practices).
- Seal & Send: Place the specimen in the pre‑labeled, prepaid mailer. No extra trip to the post office counter needed.
- Results: Secure online results within a few days, with clear next‑step instructions.
- Treatment & Partners: If positive, a clinician can guide antibiotic treatment and discuss partner notification so you don’t get reinfected.
Ready to make screening simple? Start with our discreet Chlamydia Home Test Kit, or go broader with the 7-in-1 STD At-Home Rapid Test Kit if you want a multi‑infection screen.
Prevention That Actually Fits Real Life
Delaware’s numbers won’t drop on posters alone. They’ll drop when prevention fits into messy, busy lives. Here’s what moves the needle without moralizing:
- Routine Testing: Make screening a calendar event every 6–12 months, or sooner with a new partner.
- Site‑Specific Screening: If you have oral or anal sex, ask for throat and rectal testing. Urine‑only screens can miss infections.
- Condoms/Dental Dams: Use them more often, not perfectly always. Even partial increases lower risk in a network.
- Faster Partner Treatment: If positive, loop partners in quickly. Consider expedited partner therapy where available through a clinician.
- Post‑Treatment Retest: Recheck about three months after treatment to catch reinfection early.
“I Didn’t Want Anyone to See Me at the Clinic”
Rene, 24, lives near Dover without a car. “I work split shifts, and the clinic closed before I got off. I also didn’t want to bump into someone I knew.” After a partner texted a positive result, Rene ordered a kit that night. “I mailed it on my lunch break. When it came back positive, the nurse set up treatment and told me exactly how to tell partners. It was way less scary than I thought.”
“Home testing made it practical. I stopped guessing and actually did something.”

People are also looking for: Am I crazy to be terrified of getting tested?
FAQs
1. Why do so many people in Delaware have chlamydia?
A lot of things happen at once: many infections don't show any symptoms, so people don't get tested until a partner tells them or problems arise. Transmission happens faster in small, connected social networks, especially among people aged 15 to 24. In small towns, things like clinic hours, transportation, and stigma make it harder to get help, and the disease keeps spreading.
2. Does Delaware's high ranking mean it is more dangerous than other states?
Not always. A higher ranking can mean better screening and reporting, which is good for finding infections that are hard to see. It does mean that the disease is still spreading, though, so the best thing to do is to test more often and treat partners quickly.
3. How often should I get tested for chlamydia in Delaware?
If you have sex, you should get tested every year, especially if you're under 25. If you have sex without a condom, with a new partner, or if your partner tests positive, you should test sooner. If you've had chlamydia before, get tested again about three months after treatment to catch it early.
4. Is it possible to get chlamydia from oral sex?
Yes, you can get throat infections after having oral sex with someone who has one. They are often mild or have no symptoms, which is why they go unnoticed. If you have oral sex, ask for a site-specific screening (throat swab).
5. Are home tests for chlamydia correct?
When you use a kit that has lab-based NAAT (the clinical gold standard) and follow the directions, the results are as accurate as those from a clinic. For accurate results, it's important to collect samples correctly and mail them on time. After getting positive results, you should see a doctor and tell your partner.
6. Will my insurance pay for a home chlamydia test?
A lot of plans will pay for STD testing, but the benefits depend on the insurer and the kit. Some Delaware community programs offer free or low-cost options for people under 25 or who need help with money. You can pay out of pocket and still keep records in case you want to get your money back later if privacy is a concern.
7. How do I let my partner know I have chlamydia?
First things first, be honest and straightforward. The conversation won't be pleasant, but it'll only get worse the longer you take to have it. Chlamydia is perfectly treatable as long as you act fast. Give your partner a link or phone number to a clinic, or better yet, set up a test for them if you believe you might've exposed them. If talking to your partner directly makes you feel unsafe or stressed, ask a clinic about services that let you tell your partner without giving your name.
8. What happens if you don't treat chlamydia?
Some people with a uterus who don't get treated for infections can get pelvic inflammatory disease (PID) and have trouble getting pregnant later on. Ongoing infections can cause urethritis and raise the risk of getting or spreading other STIs in anyone. Early testing and antibiotics stop problems before they start.
9. After treatment, can I test positive again?
Yes, most "positives after treatment" are from getting sick again from a partner who hasn't been treated or is new to the area. That's why it's so important to treat your partner and test again in three months. While your partner is being tested and treated, use condoms or dental dams more often.
10. Do I need to have a urine, throat, or rectal test?
It depends on how you have sex. Urine-only tests can miss infections in the throat or rectum, so ask for swabs that are specific to your needs. This is especially important if you want a full screen and have oral or receptive anal sex.
Get Privacy and Clarity
Delaware’s high chlamydia rate is a reminder, not a verdict. You can take control of your sexual health without shame, without hassle, and without unnecessary delays. Whether you live in Wilmington, Dover, or a rural corner of Sussex County, testing is within reach.
Skip the guesswork and make screening part of your routine. The sooner you know, the sooner you can treat, and prevent passing it on.
Sources
1. CDC – 2023 STD Surveillance: State Ranking Tables
2. Testing.com – Delaware STD Statistics










