Quick Answer: Herpes isn’t the only STD that can live in your mouth. Oral gonorrhea, chlamydia, syphilis, HPV, and even HIV can be transmitted through oral sex or close contact. Symptoms range from sore throat and swollen tonsils to ulcers, white patches, or no symptoms at all. The only way to know? Get tested, and yes, you can screen for oral STDs at home with the right kit.
Why We Underestimate Oral STDs
Oral sex is often framed as “low risk” or even “not real sex,” especially in sex education (if you got any at all). That framing is flat-out wrong, and dangerous. Every mucous membrane in your body can absorb STDs. That includes your throat, your gums, your tongue, your lips. So yes, you can get (and give) STDs through oral sex, even if it’s just “a little” or “just the tip.”
Most people aren’t taught this. That’s why symptoms like a sore throat, ulcers, or tonsil swelling go ignored. Worse? Many oral STDs have no symptoms at all. You could be carrying and transmitting infections for months before realizing something’s wrong.

People are also reading: Why Black Communities Face the Highest STD Rates, And What No One’s Fixing
Chlamydia and Gonorrhea Can Live in Your Throat
Let’s start with the two most commonly diagnosed STDs: chlamydia and gonorrhea. While most people associate them with genital infections, both can live in the throat, especially in people who give unprotected oral sex.
Oral gonorrhea can cause persistent sore throat, white spots on the tonsils, or a mild burning sensation. But often, there are no symptoms at all. It’s also harder to treat due to growing antibiotic resistance.
Oral chlamydia is rarer, but still possible. It may present with throat irritation, hoarseness, or swollen lymph nodes. Both infections can be passed back and forth between partners if left untreated.
The fix? At-home throat swab kits are now available for both. Don’t assume your negative genital test means you’re clear, ask for oral-specific screening.
Syphilis and Its Sneaky Mouth Sores
Syphilis in the mouth usually shows up in Stage 1 as a single, firm, painless sore, often mistaken for a canker sore or irritated bite. It can appear on the lips, tongue, or inside of the cheek. And because it doesn’t hurt, most people ignore it until it disappears.
Bad idea. That painless ulcer (called a chancre) means the infection is in your blood and spreading. Weeks or months later, syphilis can cause rashes, fever, hair loss, and even damage to your brain or heart if untreated.
And yes, oral syphilis is highly contagious. A quick kiss, shared drink, or single session of oral sex can transmit it. Early testing and treatment (usually one penicillin shot) can stop it fast.
HPV: The Virus You Can’t See, Until It’s Cancer
Human papillomavirus (HPV) is one of the most common STDs in the world, and it doesn’t just affect genitals. Some strains can infect the mouth and throat, increasing the risk of oropharyngeal cancer, especially in people assigned male at birth.
There’s no standard oral test for HPV, which makes it even harder to detect. Most people never show symptoms. But over time, persistent HPV infections in the mouth can lead to abnormal cell changes and, eventually, tumors.
The best protection? The HPV vaccine (Gardasil) for anyone under 45, and barrier protection like condoms or dental dams during oral sex.
Check Your STD Status in Minutes
Test at Home with RemediumPapillomavirus (HPV) Test

 For Women
For Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $33.99 $49.00
Can You Get HIV from Oral Sex?
Short answer: yes, but the risk is low. Oral transmission of HIV is far less common than vaginal or anal routes, but it's still possible, especially if the giving partner has cuts, gum disease, or open sores in the mouth.
The receiving partner is also at risk if semen or vaginal fluids enter the mouth and absorb through mucous membranes. Add bleeding gums, recent dental work, or STDs that break skin barriers (like herpes or syphilis), and the odds go up.
Most HIV oral transmission cases happen during unprotected oral sex with ejaculation, and the risk increases if the infected person has a high viral load. The good news? People on HIV treatment with undetectable viral loads cannot transmit the virus, period. That’s what “U=U” (undetectable = untransmittable) is all about.
Mouth-to-Genital vs. Genital-to-Mouth: Which Is Riskier?
This trips people up: who’s actually at risk during oral sex, the giver or the receiver? The answer is: both, but the giving partner (mouth) is typically at higher risk for acquiring STDs.
Why? Because your mouth is full of delicate tissue, blood vessels, and soft surfaces that make it easier for viruses and bacteria to enter your body. Plus, your mouth often comes in contact with secretions from the genitals, which may carry infections even when someone looks “clean.”
However, reverse transmission (mouth to genitals) can still happen, especially with infections like HSV-1 (oral herpes), which can cause genital outbreaks through oral contact. It’s not a one-way street.
Can You Get an STD from Kissing?
Surprise, yes. While most STDs don’t spread easily through kissing, some absolutely can, especially if there are open sores or bleeding gums involved. These include:
- Herpes simplex virus (HSV-1) , spreads through direct contact with cold sores or asymptomatic shedding
- Syphilis , if a chancre is present in the mouth or lips
- CMV (Cytomegalovirus) , often overlooked but can be sexually transmitted through saliva
- Mono (Epstein-Barr virus) , not an STD technically, but spreads through kissing and weakens your immune system
Deep kissing or "French kissing" increases the risk if either partner has active infections or bleeding gums. The risk isn’t sky-high, but it’s real. Don’t downplay symptoms just because kissing “feels safe.”
People are also reading: STD Rash vs Allergic Reaction: Why It’s So Easy to Get It Wrong
How to Test for Oral STDs
Here's the most overlooked part of oral STD care: testing often skips the mouth entirely. Most clinics default to urine or genital swabs. Unless you ask specifically for throat or oral swabs, you might leave thinking you're "clean" when you’ve only been half-tested.
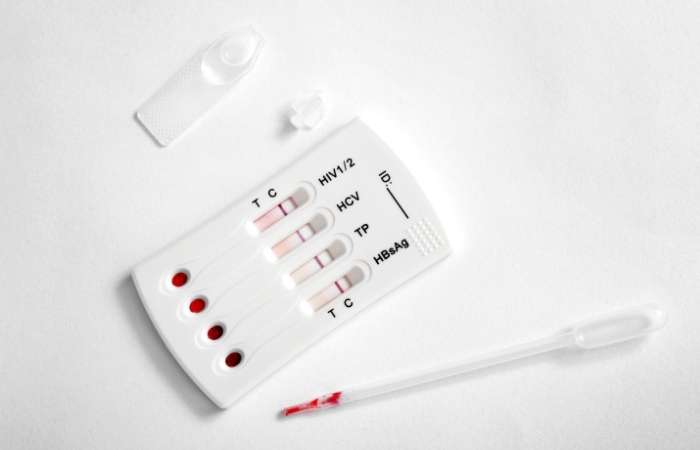
That’s why at-home kits with oral and throat swab options are essential. Look for kits that include oral chlamydia, gonorrhea, and syphilis screening. Some HIV tests also use oral fluid instead of blood, helpful if you hate needles.
Want a discreet option that covers the mouth and genitals? Check out STD Rapid Test Kits here, they offer multi-site testing that actually reflects how people have sex.
What Happens If You Don’t Treat an Oral STD?
Out of sight, out of mind? Not quite. Untreated oral STDs don’t just stay put, they spread. Gonorrhea and chlamydia in the throat can pass back to your genitals (or a partner’s) during sex. Untreated syphilis can progress to damage your heart, brain, and nervous system.
Even if you have no symptoms, the infection is still active, and still transmissible. Oral HPV may not hurt, but it’s been linked to rising rates of oropharyngeal cancer, especially in cis men. Herpes, if undiagnosed, can lead to frequent outbreaks or get passed to new partners unknowingly.
Bottom line: If it’s in your mouth, it’s in your system. Don’t wait for symptoms to scream at you. Catch it early, treat it fast, and avoid complications for yourself and others.
Oral STD Treatment: What to Expect
Treatment for oral STDs is generally the same as for genital infections, just tailored to the site. If you test positive for oral gonorrhea or chlamydia, your provider may prescribe oral antibiotics or a single-dose injection.
Syphilis is treated with penicillin, usually a single shot if caught early. Herpes (HSV-1 or HSV-2) is managed with antivirals like acyclovir or valacyclovir to reduce outbreaks and transmission risk.
HPV-related changes in the mouth may require specialist follow-up, biopsy, or monitoring depending on severity. There’s no cure for HPV, but the immune system clears most strains naturally within two years.
Check Your STD Status in Minutes
Test at Home with Remedium10-in-1 STD Test Kit

 For Women
For Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $189.00 $490.00
For all 10 tests
Dental Dams, Condoms, and Real Prevention
You’ve probably never seen a dental dam outside a sex-ed slideshow. But they’re one of the best ways to prevent oral STD transmission. A dental dam is a thin sheet of latex placed over the genitals or anus during oral sex. It blocks fluid exchange without killing the vibe.
If you don’t have one, cut open a condom or use non-microwavable plastic wrap (seriously). You’ll still feel contact, but keep your mouth safe from infections.
Condoms during fellatio, regular testing, and avoiding oral sex during active outbreaks (like herpes sores or strep throat) also go a long way. Use mouthwash with hydrogen peroxide or alcohol after oral sex if you’re worried about exposure, it’s not foolproof, but it can help reduce bacteria.
How to Talk About Oral STDs With Your Partner
It’s awkward. But it’s necessary. If you’re sexually active, you should be able to say: “Have you been tested for oral STDs?” or “Do you usually use protection during oral?”
These conversations don’t have to kill the mood. Try starting the convo outside the bedroom, stay nonjudgmental, and share your own testing routine to make it mutual. If you’ve tested positive for an oral STD, let your partner(s) know so they can get tested too, it’s not just ethical, it’s health-preserving.
Trust, transparency, and testing go hand in hand. The more you normalize these talks, the easier they get. You’re not being dramatic. You’re being responsible.

People are also reading: Private, Fast, and 92% Accurate? At-Home STD Tests Explained
FAQs
1. Can you get chlamydia in your mouth?
Yes, although it’s less common than genital chlamydia. It can cause sore throat or go unnoticed. Throat swabs are required to detect it.
2. Is oral gonorrhea curable?
Yes. It’s treated with antibiotics, but growing resistance makes timely treatment essential. Always follow up if symptoms persist.
3. Do I need a separate test for oral STDs?
Usually, yes. Most standard STD panels only test urine or genital swabs. Ask for oral swabs or buy a kit that includes them.
4. What does an oral STD sore look like?
They can appear as ulcers, red patches, white spots on the tonsils, or painless lesions. Syphilis sores are usually firm and not painful.
5. Can HPV cause mouth cancer?
Yes, especially in people with long-term infections of high-risk HPV strains. It’s more common in cisgender men and people over 40.
6. Can I pass oral herpes during oral sex?
Yes. HSV-1 from the mouth can cause genital outbreaks if passed during oral sex, even without visible sores.
7. How accurate are at-home oral STD tests?
Highly accurate if used properly. Some throat swab tests reach 95–99% accuracy. Read instructions carefully and avoid eating/drinking before testing.
8. Can kissing give you an STD?
Yes, especially herpes, syphilis, and CMV. It’s rare, but possible, especially with open sores or oral bleeding.
9. Should I stop oral sex if I have a sore throat?
Yes. It could be a sign of an STD or other infection. Avoid oral sex until you’ve been tested and cleared by a provider.
10. Can I use mouthwash after oral sex to reduce STD risk?
Some studies suggest mouthwash with alcohol or hydrogen peroxide may reduce gonorrhea risk, but it’s not a substitute for protection or testing.
Conclusion
Your mouth isn’t immune. Oral STDs are real, common, and often missed. Whether it’s herpes, gonorrhea, syphilis, or even HIV, these infections don’t care if you’re using your hands, your mouth, or your whole body. If there's contact, there’s risk.
The good news? You can prevent, detect, and treat all of them. All it takes is honest info, consistent testing, and sex that prioritizes health, not just heat. Protect your mouth the way you protect everything else. It deserves that much.
For private, accurate, multi-site testing kits that don’t skip your throat, shop STD Rapid Test Kits now. Because sexual health should include every part of your body, especially your mouth.
Sources
3. CDC – HPV and Oropharyngeal Cancer: Facts about oral HPV and cancer risk
4. CDC – Cancers Linked With HPV Each Year: Oral cancer incidence in the U.S.










