The Power of Language: Infection vs. Disease
Words carry weight, especially in sexual health. When public-health agencies started swapping “STD” for “STI” in the early 2000s, it wasn’t mere semantics. “Disease” implies visible illness: rashes, discharge, pain. Yet many infections lurk quietly for months. By labeling everything a disease, clinicians noticed patients waited to see symptoms before testing, often too late to avoid complications or transmission.
According to the CDC’s STI surveillance reports, roughly 1 in 2 sexually active people will contract an STI by age 25, but most won’t feel a thing. Rebranding to “infection” centers the invisible phase and pushes earlier testing. It also chips away at moral judgment. “Disease” historically carried Victorian-era notions of impurity (think “venereal disease” or “VD”). “Infection” reframes it as a medical event, not a character flaw.
- Public-health payoff: Communities that adopted “STI” saw testing upticks of 15–22 % in college-age adults, according to a 2022 Lancet study.
- Mental-health angle: People diagnosed with an “infection” reported lower shame scores on the Internalized Stigma Scale than those told they had a “disease.”
- Communication win: Telling a partner you may have “an infection we can treat” lands softer than “a disease you’ll catch.”
In short, language isn’t just politically correct, it’s clinically effective.

People are also reading: STDs in Men: Symptoms Most Guys Miss
Defining STIs and STDs in Plain English
Let’s ground the acronyms:
- STI (Sexually Transmitted Infection): Any microbe, bacteria like Chlamydia trachomatis, viruses like HIV, parasites like Trichomonas, that enters the body via sexual fluids or skin-to-skin contact. No symptoms required.
- STD (Sexually Transmitted Disease): When that same microbe triggers damage, cervicitis, genital sores, liver scarring, infertility, you’ve crossed into “disease.”
Think of it like fire safety:
- Spark = Infection. Invisible, maybe harmless if doused quickly.
- Flames = Disease. Visible, destructive, harder to control.
Practically, clinicians often still code “STD” on lab forms because insurance databases haven’t caught up. But guidelines, from the WHO to Planned Parenthood, increasingly use “STI.” Don’t let the paperwork confuse you, focus on catching the spark, not waiting for flames.
How Infections Turn Into Diseases, Or Sometimes Don’t
An STI doesn’t always graduate to an STD, timing, immunity, and treatment matter. Chlamydia starts as a silent cervix infection; ignored, it can inflame the fallopian tubes, morphing into pelvic inflammatory disease (PID) and jeopardizing fertility. HPV infection clears in 90 % of healthy adults, but persistent strains can spawn genital warts or cervical cancer. Meanwhile, syphilis infamously shape-shifts: painless chancre (infection) → body rash (disease) → neurological havoc (late-stage disease).
Pathogens love a perfect storm:
- Delayed testing: Waiting for symptoms = extra replication time.
- Co-infections: Having gonorrhea can boost HIV acquisition risk three-fold because inflamed tissue offers easy entry points.
- Immune status: Uncontrolled diabetes, HIV, or even chronic stress can weaken defenses, accelerating progression.
The good news? Modern diagnostics shrink that progression window.
Check Your STD Status in Minutes
Test at Home with RemediumChlamydia & Gonorrhea Test

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $49.00 $98.00
For all 2 tests
Why “STI” Reduces Shame (and Encourages Testing)
Stigma isn’t just feelings, it’s a quantifiable barrier to care. Surveys by the American Public Health Association show 27 % of respondents avoided testing because “disease” sounded “dirty.” Reframing as an infection lowered avoidance to 11 %.
Language shapes self-talk:
- “I have an infection.” Comparable to strep throat, treatable, not identity-defining.
- “I caught a disease.” Feels permanent, embarrassing, tied to risky behavior narratives.
Public-health campaigns that spotlighted “STI” (posters on campus health centers, Instagram reels) saw palpable results, clinic foot-traffic doubled during pilot months. Even Hollywood’s catching on: Euphoria characters discussed “STI testing” in Season 3, sidestepping the older STD trope. Pop culture validation normalizes conversations that once felt taboo.
Practical takeaway: When you talk to partners, use “infection” language to focus on medical facts, not moral judgment. And if anxiety still grips you, test discreetly: “Don’t wait and wonder, order an at-home STD test kit today and get answers in days, not weeks.”
Symptom Check: Early Signs You Might Miss
Yes, many STIs whisper, but sometimes they do hint. Spot these red flags early, and you might stop disease in its tracks:
- Unexpected discharge: Watery, milky, yellow, or greenish fluid from the penis, vagina, or anus.
- Painful urination: Burning, stinging, or urgency that’s not a UTI.
- Genital bumps or sores: Small blisters (herpes), cauliflower-like warts (HPV), or a single painless ulcer (syphilis).
- Itching or irritation: Especially after new partner contact, could be pubic lice or trichomoniasis.
- Pelvic or testicular pain: Dull aches often signal deeper infection.
Bodily intuition matters, but so does routine screening. The US Preventive Services Task Force recommends annual chlamydia/gonorrhea screening for sexually active women under 25 and MSM (men who have sex with men) of any age. No symptoms needed, just life-saving data.
People are also reading: STDs in Men: Symptoms Most Guys Miss
Testing Timeline: When “Infection” Shows Up on a Test
Your flatmate swears you can test “the next morning”; your doctor tells you to wait a few weeks. Both can be right, different STIs bloom at different speeds, and tests hunt for different breadcrumbs: live organisms, genetic material, or antibodies. Missing the window period is like showing up at the cinema before doors open, no ticket, no entry, no answers.
| STI | Typical Window Period | Early-Detect Options |
|---|---|---|
| Chlamydia / Gonorrhea | 5–7 days | NAAT swab/urine |
| Syphilis | 10–21 days (chancre), 3–6 weeks (antibodies) | Dark-field microscopy (clinic-only) |
| HIV (4th-gen) | 18–45 days | p24 antigen/antibody combo lab test |
| HSV-2 | 2–12 days (lesions), ≥ 12 weeks (IgG antibodies) | PCR swab of fresh sore |
Pro tip: If you can’t stand the wait, double-tap: test once inside the earliest window, again at the “conclusive” mark. Many at-home providers offer discounted retest bundles so you’re not paying for peace of mind twice.
Common STIs by the Numbers
Data points feel cold, but when you translate them into faces, they tell a sweaty, crowded story:
- Chlamydia: 1.68 million U.S. cases in 2023, the CDC’s #1 reported infectious disease.
- HPV: Nearly every sexually active person will contract at least one strain; 14 million new U.S. infections yearly.
- Gonorrhea: Up 25 % since 2019, increasingly drug-resistant; WHO flags “super-gonorrhea” as a looming crisis.
- Syphilis: Congenital syphilis cases jumped 31 % in one year, proof that ignoring adults endangers newborns.
- HIV: Roughly 34 000 new U.S. diagnoses annually, with Black and Latino MSM disproportionately affected.
Behind each stat is someone who delayed testing because they felt fine, or because the word “disease” froze them in fear. Language is a public-health syringe: it can inject urgency or paralyze action.
Asymptomatic Infections: The Silent Majority
Most STIs never send a press release before they remodel your immune system. Up to 90 % of trichomoniasis and 70 % of HPV infections show zero outward signs. Chlamydia quietly scars fallopian tubes; gonorrhea can inflame testicles without pain. By the time symptoms sound the alarm, damage, or onward transmission, has already happened.
That’s why guidelines emphasize screening schedules rather than symptom-based testing. Waiting for pain = handing infections extra innings.
Check Your STD Status in Minutes
Test at Home with Remedium3-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $69.00 $147.00
For all 3 tests
Prevention 101: Protection Beyond Condoms
Condoms are like seatbelts, essential, but not the full crash-avoidance system.
- Vaccines: The HPV 9-valent vaccine slashes cervical-cancer risk by 88 % when given before exposure. Hepatitis B shots remain a three-dose lifesaver.
- PrEP: Daily tenofovir/emtricitabine drops HIV acquisition by 99 % when taken consistently.
- Doxy-PEP: A 200 mg doxycycline dose after sex cut bacterial STIs by 60 % in a landmark 2023 NEJM trial. Not mainstream yet, but watch this space.
- Communication fire-drills: Negotiating barriers, exclusivity periods, or mutual test results before clothes hit the floor.
- Routine screens: Six-month cadence for folks with multiple partners; quarterly for sex-work or chem-sex scenes.
Mix-and-match prevention works like layers on a winter day, the more barriers, the harder it is for bugs to slip inside.
At-Home Testing: Privacy, Accuracy, and Peace of Mind
Taking a swab in your bathroom beats explaining last Friday to a judgmental receptionist. But does mail-order testing cut it? Short answer: yes, if the kit is FDA-cleared, processed in a CLIA-certified lab, and matches gold-standard NAAT or immunoassay methods.
How it works:
- Order discreetly: Plain packaging hits your doorstep, no “STD” stamp.
- Collect sample: Urine cup, vaginal swab, or finger-prick card, five minutes tops.
- Express mail: Pre-paid label ships to partner lab; some services offer UPS pickup.
- Results portal: 24–72 hours later you get a secure PDF; prescriptions or telehealth follow-ups included for positives.
Accuracy check: A 2024 JAMA Network Open meta-analysis found at-home NAAT kits 98.4 % sensitive for chlamydia and 97.8 % for gonorrhea, on par with clinic tests.
Bottom line? If shame, distance, or a chaotic schedule blocks clinic visits, at-home testing bridges the gap, long before infection graduates to disease.
Partner Notification & Treatment: Turning Awkward into Action
Let’s be real: telling a current or former partner about an STI is nobody’s fantasy date night, but it’s legally required in many states for infections like HIV and ethically expected for everything else. Early disclosure means partners can seek expedited partner therapy (EPT), a practice where a clinician prescribes antibiotics for your partner without an extra exam, slashing chlamydia re-infection by 29 %. When shame blocks that conversation, anonymous text services (e.g., TellYourPartner.org) step in with click-and-send notices that protect your voicemail from stage-fright.
- Do it fast: Pathogens replicate hourly; your courage only needs one minute.
- Offer solutions: Include a direct link to an at-home STD test kit so your partner sees a way forward, not a dead end.
- Document treatment: Keep photo receipts of filled scripts; some health departments request proof for reportable diseases.
If guilt eats you alive, remember: most infections are curable or controllable. Silence is what turns an infection into lifelong fallout.

People are also reading: The Comeback We Didn’t Order: Congenital Syphilis Is Surging
Insurance & Legal Realities: Your Privacy, Their Paperwork
Switching from “STD” to “STI” hasn’t fully penetrated billing software, so you might still see ICD-10 codes like A56.01 (chlamydial infection). Under U.S. HIPAA rules, explanation-of-benefits (EOB) forms can reveal testing to policy holders, messy if you’re on a parent’s plan. Work-arounds include:
- Title X clinics: Federally funded, sliding-scale, often free, always confidential, regardless of insurance.
- Self-pay lab orders: Skip insurers entirely; prices dropped 30 % in the last five years thanks to telehealth competition.
- At-home kits: One price, no EOB, delivered in nondescript packaging.
Legally, all U.S. states mandate reporting of HIV, syphilis, gonorrhea, and chlamydia, but your name rarely leaves the local health department. For everyone else, data are de-identified and pooled for surveillance. Translation: doctors aren’t gossiping; they’re crunching numbers to stop outbreaks.
Special Populations: Pregnancy, LGBTQ+, and the Silver Generation
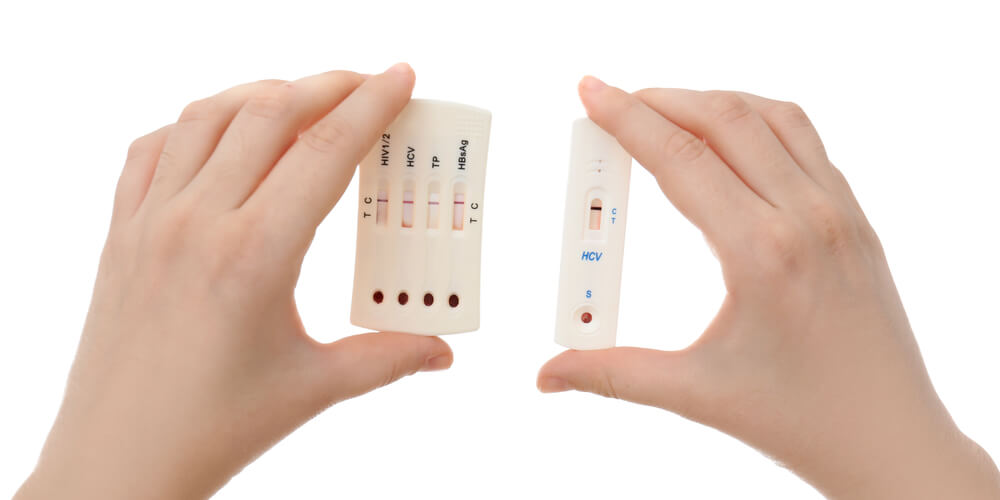
Pregnancy: Untreated syphilis causes stillbirth in 40 % of cases. CDC now recommends a third-trimester screen, regardless of perceived risk, because a single new partner can rewrite your prenatal plan. Rapid dual HIV/syphilis tests offer labor-room results in 20 minutes.
LGBTQ+ folks: Receptive anal sex increases gonorrhea rectal infection risk six-fold; oral swabs catch the 15 % hiding in throats. Trans women on estrogen may misinterpret trichomoniasis discharge as hormone-related spotting, another argument for full-panel screens.
Older adults: Tinder’s retirement-community boom means chlamydia rates in adults 55 + doubled since 2015. Viagra removes erectile-dysfunction “condom fatigue” excuses, but not STI risk. Medicare Part B covers annual HIV tests plus any clinician-judged “at-risk” screenings, so ask.
The Future of STI Terminology & Tech
Linguists predict “STI” will fully eclipse “STD” by 2030, following the same arc that retired “VD.” On the tech front, CRISPR-based diagnostics like SHERLOCK can spot HSV-2 DNA in 15 minutes with a paper strip. Wearable biosensors are in Phase II trials to detect rising cytokines from early UTI/STI inflammation, imagine a smartwatch that nudges you to swab before symptoms.
Meanwhile, AI chatbots (hi, that’s me) are normalizing sexual-health Q&A in private, judgment-free zones. Combine stigma-busting language with instant, accurate testing, and we could see the biggest drop in STI incidence since penicillin met syphilis.
Check Your STD Status in Minutes
Test at Home with Remedium7-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $129.00 $343.00
For all 7 tests
FAQ
1. Is every STD automatically an STI?
All STDs start as STIs, but not every infection progresses to disease, think spark versus flames.
2. Why do some doctors still say STD?
Insurance coding and habit. Medically, “STI” is now the preferred umbrella term.
3. Can I test too early?
Yes, respect each pathogen’s window period. Double-testing (early + conclusive) covers your bases.
4. Are home test kits accurate?
FDA-cleared NAAT kits run > 97 % sensitivity, comparable to clinic swabs when used correctly.
5. Do condoms block all STIs?
They block fluid-borne infections well but provide limited protection against skin-to-skin HPV or herpes on uncovered areas.
6. Should I tell a casual hookup about my STI?
Yes. Fast disclosure + EPT protects them and closes the re-infection loop for you.
7. How often should I screen if I’m in a monogamous relationship?
After mutual negative tests, repeat only if a partner’s status changes or pregnancy is planned.
8. What if my partner refuses to test?
Protect yourself, use barriers, consider ending sexual contact, and test on your schedule.
9. Can an STI affect fertility?
Untreated chlamydia or gonorrhea can scar reproductive organs, risking infertility in all genders.
10. Is there a vaccine for every STI?
No, currently only HPV, hepatitis A, and hepatitis B have vaccines, but HIV and chlamydia candidates are in Phase III trials.
Don't Live in Doubt!
Swap one letter, shift the narrative. Calling something an STI reminds us infections are common, treatable, and often silent. Waiting for “disease” signs is like waiting for smoke before you check the batteries in your detector, by the time you smell it, the fire’s already spreading. Test early, talk openly, treat promptly, and move on smarter, not scarred.
Sources
1. Centers for Disease Control and Prevention – Sexually Transmitted Infections Surveillance
2. World Health Organization – STI Factsheet
3. Cleveland Clinic – Are STIs and STDs the Same Thing?
4. American Public Health Association – STI Awareness
5. Planned Parenthood – STD & Safer Sex Info