Quick Answer: Yes. Untreated STDs can cause infertility in both men and women by damaging reproductive organs, triggering chronic inflammation, and blocking the normal movement of sperm or eggs, even when symptoms are mild or absent.
Why STDs and Fertility Are So Closely Connected
Fertility depends on healthy tissue, open pathways, and precise timing. Sperm must be produced in adequate numbers, move efficiently, and reach an egg. Eggs must mature, be released, and travel through open fallopian tubes. Untreated STDs interfere with these steps by inflaming or damaging the systems involved.
When the body responds to infection, it sends immune cells to fight it. This response causes inflammation, which is helpful in the short term but harmful when it becomes chronic. Over time, inflammation can lead to scar tissue, narrowing, or complete blockage of reproductive structures.
The biggest risk factor is delay. The longer an STD goes untreated, the more opportunity it has to spread upward or deeper into the reproductive system. This is why infections that cause few or no symptoms are often the most damaging to long-term fertility.

People are also reading: Why Your Vulva Might Itch After Sex (And When to Test)
How Untreated STDs Can Affect Female Fertility
In women, fertility damage most often happens when an untreated STD spreads beyond the cervix and into the upper reproductive tract. This includes the uterus, fallopian tubes, and surrounding pelvic tissues. Once this happens, the risk of lasting complications increases significantly.
A major concern is pelvic inflammatory disease, which is commonly referred to as PID. PID is not an infection but rather a complication brought about by the progression of bacteria from the vagina or cervix. One incidence of PID is enough to increase the chances of infertility, and repeated occurrences further increase this risk.
Inflammation in the fallopian tubes can lead to scarring or adhesions. This can partly block the fallopian tubes or prevent the egg from moving properly, which makes fertilization difficult. This scarring can also lead to ectopic pregnancy, which is life-threatening and affects fertility.
STDs Most Commonly Linked to Female Infertility
Chlamydia is the most common STD linked with female infertility. Moreover, it often does not display any symptoms, which enables it to linger undetected. If it remains untreated, it can continue to cause chronic inflammation, scarring of the fallopian tubes, and future difficulties with conception.
Gonorrhea can also have the same impact on the reproductive system, especially if it is contracted along with chlamydia. When the two infections are present together, they can create more severe inflammation and hasten the development of pelvic inflammatory disease.
Trichomoniasis is not as directly related to female infertility as the other infections. However, if it remains untreated for an extended period, it can continue to cause chronic inflammation and irritation in the pelvic region.
Viral infections, including HPV, do not directly impact female fertility. However, complications with cervical disease or procedures for treating cervical disease can impact future reproductive capabilities.
How Untreated STDs Can Affect Male Fertility
Male fertility is often overlooked in discussions about STDs, but untreated infections can have serious effects on sperm production and delivery. In men, fertility problems usually arise when infection causes inflammation in the testicles, epididymis, or prostate.
The epididymis is a tightly coiled tube where sperm mature and are stored. When it becomes inflamed, a condition known as epididymitis, sperm movement can be disrupted or blocked entirely. Even after infection clears, scar tissue may remain.
Untreated inflammation can also affect sperm quality. Infections may reduce sperm count, impair motility, or damage sperm DNA, all of which lower the chances of successful fertilization.
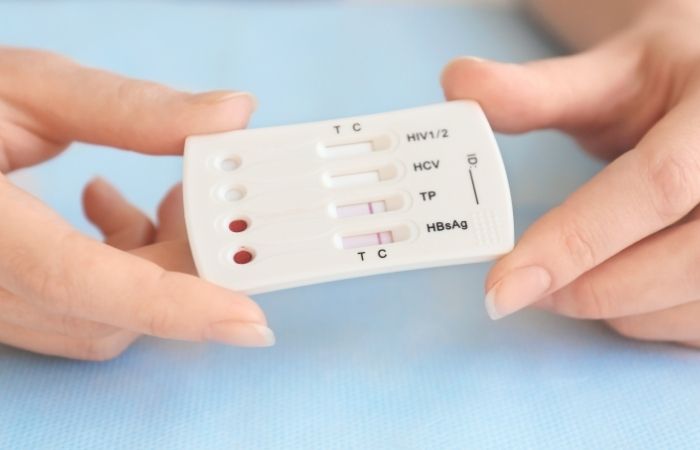
Check Your STD Status in Minutes
Test at Home with Remedium3-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $69.00 $147.00
For all 3 tests
Which STDs Are Most Likely to Cause Infertility?
Not all sexually transmitted diseases affect fertility in the same way. Some primarily cause short-term symptoms and clear with treatment, while others can quietly damage reproductive organs if left untreated. The greatest fertility risks come from infections that cause ongoing inflammation or ascend into deeper reproductive structures.
The challenge is that the STDs most strongly linked to infertility are also among the most likely to cause mild symptoms, or no symptoms at all. Without testing, people often don’t realize anything is wrong until fertility problems appear.
Chlamydia: The Leading Cause of STD-Related Infertility
Chlamydia is the most common bacterial STD worldwide and the leading STD-related cause of infertility. In women, untreated chlamydia can spread from the cervix into the uterus and fallopian tubes, where it causes inflammation and scarring. This damage can block egg transport or prevent fertilization altogether.
In men, untreated chlamydia can infect the epididymis or prostate. This can interfere with sperm maturation, reduce motility, and in some cases create blockages that prevent sperm from being ejaculated normally.
What makes chlamydia especially dangerous is how often it goes unnoticed. Many people carry the infection for months or even years without symptoms, giving it time to cause lasting reproductive damage.
Gonorrhea: Rapid Damage When Treatment Is Delayed
Gonorrhea can damage fertility more quickly than many other STDs when left untreated. In women, it can rapidly progress to pelvic inflammatory disease, increasing the likelihood of fallopian tube scarring and infertility.
In men, gonorrhea can cause painful inflammation of the epididymis or testicles. Severe or repeated infections raise the risk of long-term sperm transport problems, particularly if treatment is delayed.
Coinfection with chlamydia is common, and when both infections are present, the inflammatory response is often stronger. This combination significantly increases fertility risks for both sexes.
Syphilis and Fertility Complications
Syphilis is less commonly associated with infertility than chlamydia or gonorrhea, but untreated infections can still cause serious reproductive complications. Chronic syphilis can affect multiple organ systems and may interfere with pregnancy outcomes.
In people who become pregnant, untreated syphilis can lead to miscarriage, stillbirth, or congenital infection. While syphilis does not typically cause mechanical infertility, its systemic effects can make carrying a pregnancy to term much more difficult.
Trichomoniasis and Chronic Inflammation
Trichomoniasis is often overlooked because symptoms can be mild or intermittent. However, long-term untreated infections can cause persistent genital inflammation. In women, this may increase susceptibility to other infections and complicate reproductive health.
While trichomoniasis alone is less likely to cause infertility, its presence can amplify inflammation when other STDs are also present. Over time, this inflammatory environment may contribute to fertility challenges.

People are also reading: The Herpes Test Most People Don’t Know They Need
Viral STDs and Indirect Fertility Effects
The viral STDs such as HPV and Herpes do not cause infertility directly. However, complications arising from these infections may influence reproductive outcomes.
Advanced changes in the cervix due to HPV may necessitate procedures that compromise the integrity of the cervix, which may influence reproductive outcomes. Herpes outbreaks do not influence fertility; however, an active Herpes infection during pregnancy may influence delivery outcomes.
Even though viral STDs do not directly influence fertility, they play an important role in reproductive outcomes and cannot be ignored.
Silent Infections: Why Symptoms Aren’t a Reliable Warning
One of the most dangerous myths about STDs is the idea that you would “feel something” if an infection were harming your fertility. In reality, the opposite is often true. The infections most strongly associated with infertility are frequently silent.
Chlamydia and gonorrhea are asymptomatic in a large percentage of people, particularly women. Without pain, discharge, or noticeable changes, many individuals assume they are healthy and delay testing.
During this silent period, inflammation continues in the background. Tissue damage accumulates slowly, and by the time symptoms appear, or fertility becomes a concern, the opportunity to prevent damage may have already passed.
How Long Does It Take for Untreated STDs to Affect Fertility?
There is no specific time frame in which an untreated STD will result in fertility problems. It depends on the type of infection, the body's immune response, and whether or not a person is re-infected with an STD.
Fertility damage can start in as little as months, especially when the infection has reached the upper reproductive organs. Damage can also accumulate over time, especially with repeated infections or untreated infections.
This uncertainty is what makes routine testing so important. Fertility damage does not wait for life plans to align. It happens on the infection’s timeline, not yours.
Is Infertility From Untreated STDs Permanent?
This is the question that most people are afraid to ask, and the answer to it depends on the timing. Some of the fertility problems that result from untreated STDs are reversible, while others are not, especially when infections are left to persist over time or recur several times.
The main difference is that antibiotics can cure bacterial infections, but once scarring, blockages, or damage to sperm pathways occur, antibiotics do not reverse them. It is also important to note that the severity of symptoms is not as important as the timing of testing.
Many people assume that once an STD is treated, fertility automatically returns to normal. In reality, treatment stops further damage, but it does not always repair what has already been lost.
Check Your STD Status in Minutes
Test at Home with Remedium3-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $69.00 $147.00
For all 3 tests
When Fertility Can Recover
If an STD is diagnosed before it has spread and caused significant inflammation, fertility levels tend to return to normal. This is especially true for primary infections that are diagnosed and treated quickly and followed by proper retesting.
In males, sperm count and quality may be improved once the STD has been cleared, especially when inflammation is mild and brief. In females, early treatment may prevent pelvic inflammatory disease and preserve fallopian tube function.
This is why regular testing is emphasized, even when there are no symptoms. Early diagnosis of an STD may be the difference between temporary and lifelong fertility difficulties.
When Damage Is More Likely to Be Permanent
Permanent fertility damage is more likely when infections go untreated for months or years, or when someone experiences repeated infections. Each episode of inflammation increases the likelihood of scarring and blockage.
In women, scarring of the fallopian tubes may permanently prevent eggs from reaching the uterus. In men, blockages in the epididymis or vas deferens can obstruct sperm transport even if sperm production itself remains normal.
Because this damage is often painless, many people do not realize anything is wrong until they attempt to conceive. At that point, the infection may be long gone, but its effects remain.
Fertility After STD Treatment: What to Expect
Treatment is still essential, even if fertility damage is suspected. Clearing an infection prevents further harm, protects partners, and reduces the risk of additional complications.
For people planning pregnancy, follow-up testing is often recommended to confirm that the infection is fully cleared. In some cases, fertility evaluations may be suggested, particularly if conception does not occur after several months of trying.
It’s important to understand that fertility struggles after an STD are not a personal failure or a sign of neglect. Many infections are silent, and many people do everything “right” and still experience complications.
Why Many People Delay Testing
Despite all these risks, there are people who do not want to be tested for STDs because of fear and stigma associated with having an STD. Some people also believe that if there is something wrong, symptoms would definitely manifest.
Some people also believe that if they have been treated for an STD or have not manifested any symptoms for quite some time, then their fertility is not at risk.
Some people may not want to be tested for STDs if they are feeling well, if they are in a monogamous relationship, or if they are no longer sexually active. But it is also possible for fertility problems to manifest before all these factors are properly aligned.
It is not really careless or irresponsible behavior for people to shy away from STD testing because they are simply not aware or are confused about what is really at stake.
Testing Before Trying to Conceive
One of the most effective means of preserving fertility is preconception testing. STDs, if present, should be treated before conceiving. This minimizes any complications that might arise or any future harm to the reproductive system.
This is not gender-specific. Both men and women should be aware that STDs, if present, can affect one or both partners. Both partners share a common fertility, not separate ones.
This is especially important for individuals with new partners, a history of STDs, or a lack of regular testing. Knowing your STD status eliminates any form of uncertainty.
People are also reading: Cold Sore Kisses and Herpes Transmission: What This Story Reveals About Silent Spread
FAQs
1. Can I really be infertile and not even know it?
Yes, and it’s more common than you think. Many people carry chlamydia or gonorrhea without symptoms, especially women. The infection creeps upward into the reproductive tract, and by the time you're trying to conceive, scar tissue may already be in place. No warning. No fever. Just a blocked tube discovered years later.
2. What if I had an STD ages ago but never got tested?
That question keeps a lot of people up at night. If you were exposed and never treated, there’s a chance some damage occurred, especially if it’s been years. But that doesn’t mean game over. Many people still conceive naturally after past infections. Testing now can help you understand where things stand and what comes next.
3. Does it matter if I’ve never had symptoms?
That’s actually why this issue is so dangerous. Most people *don’t* have symptoms. You could feel totally fine and still have had an infection causing damage behind the scenes. In fact, over 70% of chlamydia cases in women have no symptoms at all. Silence doesn’t equal safety.
4. I tested negative today, so I’m in the clear, right?
Mostly, yes. A negative test means there’s no current infection. But it can’t tell you if you had something months or years ago that already did its damage. If you’re concerned about fertility, you may need further testing like a hysterosalpingogram or semen analysis to look at the bigger picture.
5. Can men lose fertility from STDs too?
Definitely. It’s not just a female problem. STDs can mess with sperm production, block the tubes that carry sperm, and even shrink the testicles over time if inflammation goes untreated. And like in women, most guys don’t notice a thing until they get a sperm test, and realize something’s off.
6. Will antibiotics fix everything?
They’ll kill the infection, yes, but they can’t reverse any scarring that’s already happened. That’s why timing matters so much. Catching it early = stopping the damage. Catching it late = managing what’s already broken. Either way, treatment still helps stop future problems.
7. What if my partner had an STD and never told me?
Oof, this happens more than people admit. They may not have known. They may have assumed it went away. But if you’ve had unprotected sex, even once, it’s smart to test. And if you’re trying to get pregnant, both partners should get screened. It’s not about blame. It’s about moving forward with facts.
8. Is trichomoniasis a fertility risk too?
not as infamous as chlamydia or gonorrhea, but yep, it can raise the risk of PID in some cases, especially if untreated. And it's sneaky. Most men don’t get symptoms. Some women think it’s just a yeast infection. But it’s worth checking for, especially if you’re TTC (trying to conceive).
9. Can I use a test at home or do I need to visit a clinic?
You can absolutely start with an at-home test, especially if going to a clinic feels like a whole ordeal. Kits like the Combo STD Home Test Kit check for the big ones (chlamydia, gonorrhea, trich) and are super discreet. If anything comes up positive, or if you want to confirm past damage, you can always loop in a provider later.
10. How do I protect my fertility moving forward?
Test early. Test often. Use protection with new partners. Treat infections fast. And don't assume feeling fine means everything’s fine. If you’re planning for a family (now or someday), staying ahead of STDs is one of the best things you can do for your future self.
You Can’t Change the Past, But You Can Protect What’s Next
Untreated STDs are one of the few preventable causes of infertility, yet they remain a common reason people struggle to conceive later in life. The damage doesn’t happen because someone was careless, it happens because infections are often silent, misunderstood, or delayed in diagnosis.
Testing is not about blame or fear. It’s about preserving options. Whether or not children are part of your future plans, protecting reproductive health now gives you more control later.
If you’re unsure of your status or want reassurance, discreet testing can provide answers without waiting or stigma. You can explore confidential options directly through STD Test Kits or consider a comprehensive screening like the 6-in-1 STD At-Home Rapid Test Kit for broader peace of mind.
How We Sourced This: This article was developed using current clinical guidance, peer-reviewed research, and public health data related to sexually transmitted infections and reproductive health. Around fifteen reputable medical and academic sources informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources. The goal was to explain fertility risks clearly, accurately, and without stigma.
Sources
1. World Health Organization – Sexually Transmitted Infections
2. Mayo Clinic – Pelvic Inflammatory Disease
3. NHS – Sexually Transmitted Infections Overview
5. About Pelvic Inflammatory Disease (PID) (CDC)
About the Author
Dr. F. David, MD is a board-certified physician specializing in infectious diseases and sexual health. His work focuses on STD prevention, early detection, and reducing long-term complications through accessible education.
Reviewed by: Sarah Collins, RN, BSN | Last medically reviewed: February 2026
This article is for informational purposes only and does not replace professional medical advice, diagnosis, or treatment.










