Quick Answer: Yes, untreated STDs can reduce male fertility by damaging sperm, inflaming the testicles or epididymis, or interfering with hormones like testosterone, even when no symptoms are present.
Why This Article Matters (and Who It's For)
This guide is for anyone with a penis who’s ever had sex and wondered, “Could an old STD mess up my chances of having kids?” Whether you’re in a long-term relationship trying to conceive, recently treated for an infection, or dealing with vague symptoms like testicle pain or low libido, you deserve straight answers.
We also wrote this for the ones who’ve never had symptoms, never gotten tested, and assume everything’s fine. Because when it comes to male fertility, silence isn’t safety, it’s often the sign that something was missed. STD Rapid Test Kits offers discreet options to check your status without judgment or waiting rooms.
In this article, we’ll explore how STDs affect male reproductive organs, sperm quality, and hormones. We’ll break down what damage is reversible, when to retest, and what testing options work best from home. And we’ll do it without shame, scare tactics, or medical jargon.
People are also reading: WHO’s New HIV Guidelines Just Dropped. Here’s What That Means If You’re Testing From Home
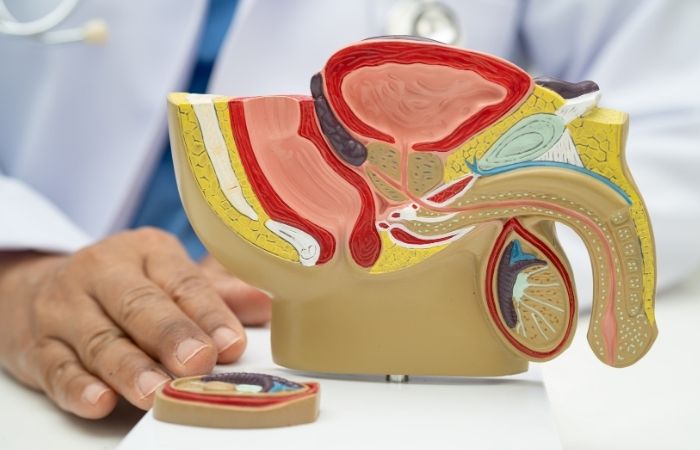
Inside the Male Reproductive System: Where STDs Do Damage
Let’s get anatomical. Sperm are made in the testicles, matured in the epididymis (a coiled tube behind each testicle), and transported through the vas deferens. To function, this system relies on clear pathways, healthy tissue, and adequate hormone levels, especially testosterone and FSH (follicle-stimulating hormone).
Here’s how different STDs can disrupt that system:
| STD | Primary Target | Potential Fertility Impact |
|---|---|---|
| Chlamydia | Epididymis, vas deferens | Scarring, reduced sperm motility |
| Gonorrhea | Urethra, testicles | Blocked sperm ducts, inflammation |
| Syphilis | Testicular tissue, CNS (late stage) | Testosterone suppression, nerve impact |
| Trichomoniasis | Prostate, urethra | Sperm DNA fragmentation, inflammation |
| HPV | Penile urethra, semen | May reduce sperm count or function |
| Herpes (HSV) | Genital skin, nerves | Rare impact, mostly psychological or indirect |
Figure 1: Where STDs impact male fertility, and how. Sourced from peer-reviewed urology and reproductive health studies.
The Invisible Threat: STD-Linked Epididymitis
One of the most overlooked fertility risks in men is epididymitis, inflammation of the epididymis, often caused by untreated chlamydia or gonorrhea. It might present as mild scrotal swelling, low-grade fever, or soreness during ejaculation. Or it might not present at all.
Over time, inflammation can cause scarring, blocking sperm from exiting the testicles. According to the National Institutes of Health, up to 40% of male infertility cases involve undiagnosed inflammation or infection, often traceable to an earlier STD.
Case in point: A 33-year-old man underwent a fertility workup after a year of trying to conceive with no success. Semen analysis showed zero motile sperm. A retroactive NAAT test detected past chlamydia. He’d never had symptoms, but the damage was done.
This is why early testing matters. Even if symptoms are subtle, getting screened and treated can prevent long-term harm.
Hormones, Sperm, and the STD Connection Most Men Never Hear About
When men think about fertility, they usually picture sperm count. But fertility is just as much about hormones, especially testosterone, as it is about numbers under a microscope. This is where long-standing or repeated STDs can quietly interfere in ways that don’t show up until much later.
Chronic infection and inflammation stress the body. Over time, that stress can suppress the hypothalamic–pituitary–gonadal axis, the hormonal communication loop that tells your testicles to produce testosterone and sperm. Studies summarized by the Centers for Disease Control and Prevention show that untreated or recurrent STDs are associated with altered testosterone levels and impaired sperm production, particularly in men with epididymal or testicular involvement.
This doesn’t mean every STD tanks your hormones overnight. It means persistent inflammation, delayed treatment, or repeat infections increase the risk, especially when symptoms were mild or ignored.
Check Your STD Status in Minutes
Test at Home with Remedium3-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $69.00 $147.00
For all 3 tests
Can Fertility Recover After an STD?
This is the question almost every man asks once the panic settles: “If I treat it, does my fertility come back?” The honest answer is, often yes, sometimes partially, and occasionally no. It depends on timing, severity, and whether structural damage occurred.
Infections caught early, before scarring or duct blockage, are far more likely to resolve without long-term fertility consequences. Antibiotic treatment can clear chlamydia, gonorrhea, and trichomoniasis, allowing inflammation to subside and sperm quality to improve over the following months.
However, if scarring has already narrowed or blocked the epididymis or vas deferens, sperm may not travel effectively, even if production resumes. This is why some men have normal testosterone levels but low or zero sperm counts after past infections.
Fertility specialists often recommend waiting three to six months after treatment before repeating a semen analysis. That window allows the body to complete a full sperm production cycle and gives clearer insight into recovery potential.
“I Had No Symptoms”: Why Men Miss the Fertility Window
One of the most dangerous myths about STDs is that you’ll “feel something” if there’s a problem. In reality, the majority of men with chlamydia or gonorrhea report no symptoms at all. No pain. No discharge. No warning.
By the time fertility becomes the concern, often years later, the infection is long gone, but the damage remains. This is especially common in men who had multiple partners, inconsistent testing, or assumed condoms eliminated all risk.
A urology review published through the NIH found that asymptomatic STDs were a leading contributor to unexplained male infertility diagnoses. In many cases, the STD was only discovered retrospectively through antibody markers or partner testing history.
This isn’t about blame. It’s about information. And it’s why proactive testing matters even when everything feels fine.
Testing Options for Men: Clinic vs At‑Home
If you’re concerned about fertility, testing is not just about the present, it’s about protecting what comes next. The good news is that men now have more discreet, accessible options than ever.
Clinic testing remains the gold standard for complex cases, especially when semen analysis or hormone panels are needed. But for STD screening itself, at‑home testing can be an effective first step, particularly for infections like chlamydia and gonorrhea that are strongly linked to fertility damage.
At‑home kits typically use urine or swab samples and NAAT-based detection, which is the same technology used in many clinics. Ordering through STD Rapid Test Kits allows men to test discreetly, without appointments, and take action sooner rather than later.
If results are positive, or if fertility issues persist despite negative results, a clinician can then guide next steps like ultrasound imaging, semen analysis, or hormone testing.

People are also reading: Queer, Unvaccinated, and At Risk: How HPV Hits Gay Men Hardest
When to Test If You’re Thinking About Kids
If pregnancy is on your radar, now or in the future, testing timing matters. Ideally, STD screening should happen before trying to conceive, not after months of frustration.
Men with any of the following risk factors should strongly consider testing:
Past STDs, even if treated. A history of testicular pain, epididymitis, or unexplained groin discomfort. Multiple partners without regular screening. A partner with a known STD history. Or fertility challenges without a clear explanation.
Testing early gives you leverage. If an infection is present, treatment can prevent further damage. If an old infection caused scarring, knowing sooner opens doors to fertility support options instead of unanswered questions.
What If You Test Positive?
First: breathe. A positive STD result doesn’t mean you’re broken, toxic, or permanently infertile. It means there’s information now, and with it, a path forward. Nearly all STDs that impact male fertility are treatable, especially when caught early. But even delayed cases have options for recovery, management, or assisted fertility care.
If your test is positive, seek treatment as soon as possible. For chlamydia, gonorrhea, and trichomoniasis, this typically involves a short course of antibiotics. For viral infections like herpes or HPV, your provider may recommend symptom management and longer-term sexual health monitoring.
It’s also important to let partners know, both current and recent. This isn’t about blame, it’s about giving them the same opportunity to test, treat, and protect their own fertility. Anonymous notification tools exist. So do compassionate scripts if you're not sure how to start the conversation.
If fertility is your concern, ask your provider about follow-up testing in 3–6 months. Semen analysis, hormone panels, and physical evaluation of the reproductive tract can clarify whether there’s been lasting damage, or if your system just needs time to reset after infection clears.
FAQs
1. Can chlamydia really make a guy infertile?
It can. Not always, but if it hangs around untreated, it can mess with the tubes that carry sperm out of the testicles. Think of it like a silent traffic jam that no one clears until it's too late. And the kicker? Most guys with chlamydia never feel a thing. No pain, no weird discharge, nada.
2. My test was positive, does that mean I can’t have kids?
Not necessarily. A positive result is a red flag, not a death sentence for your fertility. If you treat the infection early and follow up with a semen analysis, there's a good chance your system bounces back. We've seen guys go from zero sperm to full motility six months post-treatment. Biology is wild, and resilient.
3. Does herpes affect fertility in men?
Technically, no. Herpes doesn’t damage sperm or block anything. But flare-ups can make sex painful or unpredictable, which can throw off conception timing. And stress around outbreaks can mess with your libido or performance. So, not sperm damage, but the emotional toll? Very real.
4. I had an STD years ago. Could it still be affecting my fertility now?
Unfortunately, yeah. If the infection caused scarring or inflammation in your reproductive tract, the effects might linger even if the infection itself is long gone. That’s why fertility specialists often ask about your full STD history, not to judge, but to troubleshoot.
5. How do I know if I had an STD with no symptoms?
You probably don’t, until you test. That’s the problem. Some STDs are sneaky like that. The only way to know for sure is to screen regularly, especially if you’ve had multiple partners or went through a “didn’t ask, didn’t tell” phase. No shade. Just facts.
6. Is there a sperm test I can do at home?
Yep, there are at-home sperm tests that check count and movement. They're not super detailed, but they give a good snapshot. For the full picture, volume, shape, motility, DNA fragmentation, you'll need a lab test or fertility clinic. And if you're serious about baby-making, combining that with STD screening is smart.
7. Can HPV mess with my sperm?
Possibly. Some studies suggest HPV can stick to sperm and affect how well they swim or fertilize an egg. The science isn’t totally settled, but if you or your partner are trying to conceive, it’s worth discussing with a doctor. And yes, guys can get HPV too, even if we don’t always get warts or symptoms.
8. Does an STD mess with testosterone?
It can, especially if the infection spreads to your testicles or lingers long enough to spark systemic inflammation. You might notice low energy, trouble focusing, or a disappearing sex drive. If any of that’s happening, get tested. It's not “just stress” if your hormones are crashing.
9. Can I still get someone pregnant after having an STD?
Totally possible. Lots of people do. If your infection was treated quickly, odds are good your sperm are still doing their thing. But if it's been a while, or if you’ve had repeat infections, get a semen analysis. Better to know than wonder.
10. What’s the best STD test for fertility peace of mind?
A combo test that checks for the big culprits: chlamydia, gonorrhea, syphilis, and trichomoniasis. Those are the most likely to impact fertility. Bonus points if it’s at-home, private, and uses NAAT tech, the gold standard for accuracy.
Check Your STD Status in Minutes
Test at Home with Remedium10-in-1 STD Test Kit

 For Women
For Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $189.00 $490.00
For all 10 tests
You Deserve Answers, Not Assumptions
Infertility can feel like a betrayal, of your body, your past choices, or the silence you mistook for safety. But it doesn’t have to stay a mystery. Testing is clarity. Treatment is power. And even when damage has occurred, there are paths forward for healing, conception, and peace of mind.
Whether you're dealing with past regrets, current symptoms, or future plans, your fertility story is still being written. And it starts with knowledge.
Don't leave your future to guesswork, get the clarity you deserve. This at-home combo STD test kit screens for the most common male fertility-impacting infections, privately and fast.
People are also reading: Rash After Sex: Common Causes and When to Test
People are also reading: Tested Positive for Chlamydia: What to Do Next
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted six of the most relevant and reader-friendly sources.
Sources
CDC – Sexually Transmitted Infections
NIH: Male Infertility and Infection-Related Causes
Planned Parenthood – STDs and Safer Sex
Urology Care Foundation – Male Infertility
Healthline – Epididymitis Overview
Medical News Today – Chlamydia in Men
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: Jenna A. Voss, RN, MPH | Last medically reviewed: February 2026
This article is for informational purposes and does not replace medical advice.










