Quick Answer: A syphilis chancre is a painless, firm sore that appears where the bacteria entered your body, usually the genitals, mouth, or anus. It’s highly contagious even without pain or other symptoms.
The Sore That Doesn’t Scream: Why Syphilis Is So Easy to Miss
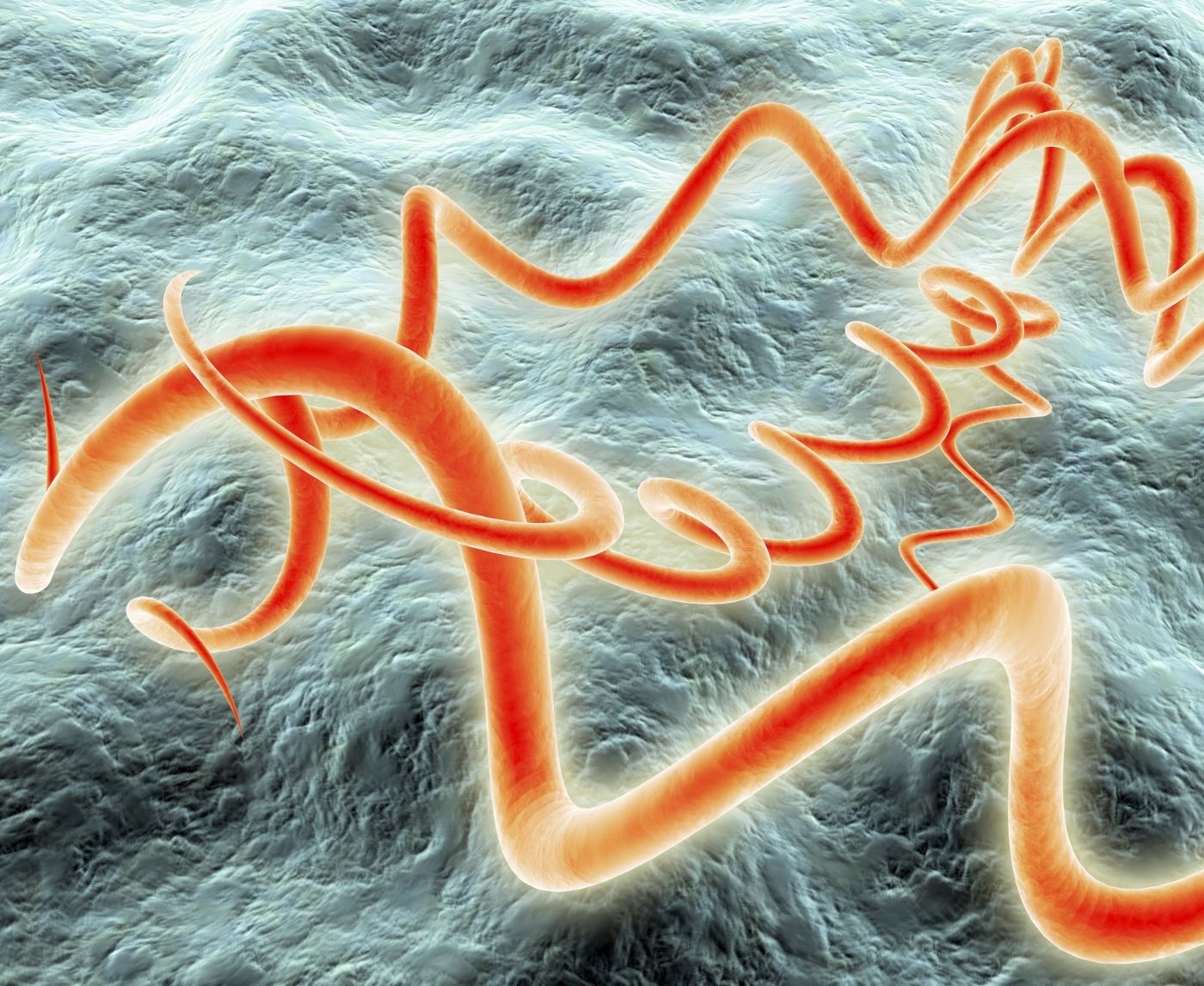
Unlike herpes, which usually burns, stings, and blisters, a syphilis chancre doesn’t beg for attention. It’s typically round or oval, may feel hard at the edges, and often pops up alone. No discharge. No pus. Just... there. Quietly. Waiting.
This is why syphilis spreads silently. Many people think STDs must hurt, ooze, or come with a fever. But in reality, the first stage of syphilis is stealth mode. It can appear as a sore on your genitals, mouth, or even hidden spots like your inner rectum or under foreskin. Some people only discover it by accident while shaving, wiping, or having a partner point it out mid-hookup.
Chancres generally show up between 10 to 90 days after exposure, most commonly around three weeks. They stick around for 3 to 6 weeks, then disappear on their own. But disappearing doesn’t mean the infection is gone. It just means it's leveling up into the bloodstream, preparing for the next stage.
Not Every Bump Is a Chancre, But Here’s What to Watch For
Let’s be honest, genital skin is complicated. Ingrown hairs, friction burns, cysts, herpes, even shaving cuts can all cause bumps. So what makes a chancre different?
For one, it’s almost always painless. That alone can be a red flag, because most other genital bumps cause some level of irritation. Second, it tends to be solitary, just one sore, not a cluster. And third, it has a firmer, ulcer-like appearance: not fluid-filled, not crusty, just raw in the center with clean edges.
| Condition | Painful? | How Many Sores? | Fluid or Crust? | |
|---|---|---|---|---|
| Syphilis Chancre | No | Usually one | No fluid; raw center | Genitals, anus, mouth |
| Herpes | Yes | Multiple blisters | Clear fluid, then crust | Genitals, anus, mouth |
| Ingrown Hair | Sometimes | One | Possible pus | Anywhere shaved |
| Friction Burn | Yes | One or more | None unless infected | Labia, penis shaft, thighs |
Table 1. Symptom comparison between common genital sores and a syphilis chancre.
Still unsure? That’s normal. The human body doesn’t come with labels, and a lot of sexually transmitted infections mimic each other. The safest way to know is to test. But not just any test, a rapid syphilis test or blood screening at the right time can detect it early, even if symptoms are vague or gone.

People are also reading: Can HIV Show Up in Your Mouth? Early Signs You Shouldn’t Ignore
How Long Does a Chancre Last, And Why It Matters
Most people don’t even realize the chancre is gone until weeks later, by then, syphilis has moved on without fanfare. That’s the trap. A syphilis chancre typically lasts around 3 to 6 weeks before healing without treatment. No scar, no scab, nothing dramatic. Just a quiet exit. But while it’s there, it’s a live wire of infection.
Even if you use condoms, contact with the sore itself, during oral sex, mutual masturbation, or even close skin-to-skin rubbing, can transmit Treponema pallidum, the bacteria that causes syphilis. And since many chancres show up in spots condoms don’t cover (think scrotum, labia, inner anus), you could be doing everything “right” and still be exposed.
Here’s the tricky part: once the sore disappears, the risk of spreading syphilis goes down, but the disease is far from gone. It’s now circulating in your bloodstream, preparing for stage two. That’s when a rash may show up, or... nothing at all. It’s possible to carry syphilis silently for years, especially if you miss the window to test during the chancre stage.
| Stage | Chancre Presence | Contagious? | What Happens |
|---|---|---|---|
| Primary | Yes | Yes | Painless sore appears where bacteria entered |
| Secondary | No | Yes | Rash, flu-like symptoms, mouth or anal ulcers |
| Latent | No | No (early latent may be) | No symptoms; still in body, detectable by blood test |
| Tertiary | No | No | Damage to organs, nerves, brain (rare with treatment) |
Table 2. Stages of syphilis and when the infection is contagious.
By the time someone gets symptoms like fever, joint pain, or rash on the palms or soles, the window for early treatment is closing. That’s why identifying the chancre early, when it’s still painless, small, and visible, is one of the best opportunities to stop syphilis in its tracks.
Check Your STD Status in Minutes
Test at Home with RemediumSyphilis Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $33.99 $49.00
Testing Timing: When to Check for Syphilis (and What to Use)
If you’ve had a sore that’s come and gone, or you’re looking at a current one and wondering, testing now is better than waiting. The most reliable syphilis tests look for antibodies in the blood, not the sore itself. So even if the bump is healing or has vanished, your body will still show signs of the infection if it’s there.
Most guidelines suggest testing around 3 to 6 weeks after exposure. Earlier tests (as soon as 10–14 days) can pick up infections in some cases, but may require retesting for confirmation. Rapid at-home tests for syphilis work similarly to lab-based blood tests, they detect antibodies, not the bacteria itself.
If you’re within the exposure window and concerned, here’s what makes sense:
Get tested now. If it’s negative but the sore looked suspicious, test again in 2–4 weeks to confirm. This two-step approach helps you avoid false negatives while still taking action early. And if you’re positive? Treatment is simple, fast, and often just one antibiotic injection away.
Whether you're unsure about that bump or you’ve had a partner mention possible exposure, peace of mind is just one test away. This at-home syphilis test gives fast results in minutes, no waiting room, no awkward questions.
Real Talk: Stories of Missed Chancres and What Happened Next
Sofia, 27, thought it was an ingrown hair. She had just returned from a weekend camping trip with her partner when she noticed a tiny, round sore near her bikini line. “It didn’t hurt. I just figured it was from chafing or something,” she said. By the time her partner tested positive for syphilis six weeks later, Sofia’s sore had healed and she had no symptoms. But the bacteria was in her blood, and she had unknowingly exposed a new partner during that time.
Malik, 33, tested on day five after a hookup when he noticed a lesion. His rapid syphilis test came back negative. “I was relieved, but also unsure. It still looked weird,” he admitted. Two weeks later, the sore vanished, but then came the rash, pink spots on his chest, then palms. A second test confirmed what the first one missed. He began treatment immediately, and his partner tested too.
Stories like these highlight the emotional fog around syphilis testing. Doubt. Delay. Disbelief. It’s okay to not know right away, but it’s not okay to ignore your instincts. If something looks off, if your partner tested positive, or if your gut says something’s not right, test and retest as needed.
Where Chancres Show Up, and Why You Might Never See Them
Syphilis doesn’t always leave a visible calling card. If the bacteria enters through oral sex, the chancre might be tucked behind your tonsils or on the inner cheek. If exposure happens during anal sex, it could show up just inside the rectum, where you’d never spot it unless symptoms like bleeding or discomfort push you to look closer.
That means many people, especially those with receptive anal or oral sex, may never notice a chancre at all. Add to that shaved pubic areas, dark skin tones, or locations where people simply aren’t used to inspecting, and it’s easy to see how this symptom slips by unnoticed.
Partners often don’t notice either. A sore under the foreskin, hidden in the labia, or tucked near the anus can go entirely unremarked during even the most enthusiastic encounters. Furthermore, because syphilis can spread only through skin-to-skin contact with the sore, not through ejaculation or penetration, many people think they are immune to it.
This is one reason why syphilis disproportionately affects men who have sex with men (MSM), people with multiple partners, and those in underserved communities where routine testing access is limited or stigmatized. It’s not about “dirty sex” or “bad decisions.” It’s about how invisibly this disease moves through touch and time.
What About Pregnancy, HIV, and Reinfection?
The serious part is that syphilis during pregnancy can result in stillbirth, miscarriage, or a potentially fatal congenital infection for the unborn child. Untreated syphilis can still pass through the placenta even if you don't have any symptoms and your chancre has long since disappeared. For this reason, syphilis testing is part of prenatal screening, and retesting may be required later in pregnancy if there is continued risk.
The symptoms of syphilis may be different if you have HIV or a weak immune system. You could have worse ulcers, a faster progression, or symptoms that are similar, which makes it harder to figure out what's wrong. The pain and swelling from syphilis can also make you more likely to get or spread HIV.
Reinfection is possible too. Treating syphilis once doesn’t give you immunity. You can get it again from a partner who’s untreated, or newly exposed. Some people test positive more than once in their lives. It’s not failure. It’s just life. That’s why testing after new partners, unprotected sex, or unexplained symptoms is smart, not shameful.

People are also reading: From Gums to Tonsils: The STD Symptoms Dentists Are Catching First
Breaking the Silence Around "Silent" STDs
There’s something especially insidious about a disease that doesn’t announce itself loudly. When people think of STDs, they picture burning, itching, obvious signs. But syphilis often shows up without a single red flag that feels urgent. That’s the danger, and the reason rates are rising worldwide.
In many communities, especially among queer men, sex workers, and rural populations, syphilis carries an outsized stigma. People avoid getting tested not because they don’t care, but because they’re scared. Of being judged. Of being seen at a clinic. Of confirming something they don’t want to know.
But knowing is power. A chancre may be silent, but testing speaks volumes. It says: I care about my partners. I take my health seriously. I’d rather face facts than infect someone unknowingly. And if you’re not ready to talk about it yet, that’s okay. That’s what discreet testing exists for.
Every sore tells a story. Sometimes that story is simple, an irritation, a blocked follicle, a harmless zit. But sometimes, it’s syphilis. And if it is, you deserve to know while it’s still easy to treat. One painless sore could change everything. Or it could just be a bump in the road, if you catch it early enough.
If your gut is telling you something’s off, even if the bump’s gone and things seem normal, don’t wait. This at-home STD combo test screens for multiple infections with one discreet kit. Because sometimes, the most dangerous STDs are the ones you can’t feel.
Check Your STD Status in Minutes
Test at Home with Remedium7-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $129.00 $343.00
For all 7 tests
“I Thought It Was Nothing.” (But It Wasn’t.)
Alex, 24, had just moved cities. New job, new dates, new everything. So when he found a smooth little bump near the base of his penis, he didn’t stress. “No pain. No weird color. Just... there.” It vanished in two weeks. End of story, right?
Wrong. Two months later, a routine test lit up positive for syphilis. “I didn’t feel sick. No rash. No nothing. But the blood work didn’t lie.” That’s the part that haunted him most, not the diagnosis, but how easily it slipped under his radar. “If I hadn’t tested early, I might’ve spread it without knowing. That sucked to think about.”
There’s no shame in missing a symptom that hides so well. That’s why the smartest move isn’t waiting for answers, it’s creating them. With rapid tests, you don’t need to guess. You don’t need to explain yourself to a stranger behind a desk. And you definitely don’t need to stay in the dark.
STD Rapid Test Kits offers discreet, affordable ways to get clarity on your own terms. So if you're wondering, worrying, or waiting, stop. One painless bump is reason enough to act. You’re worth the peace of mind.
FAQs
1. Does a syphilis sore hurt?
Nope, and that’s the messed-up part. Most chancres don’t hurt at all. They just sit there silently, looking harmless. One guy described his as “like a paper cut I didn’t remember getting.” No burn, no itch. And because it’s painless, people don’t treat it like a red flag. But it absolutely is.
2. Where do chancres usually show up?
Wherever the bacteria got in. That means mouth, penis, vagina, anus, anywhere skin made contact. A lot of people expect to see it right on the tip or outside, but some sores hide in folds or just inside the rectum or throat. You could miss it completely if you’re not looking closely or if it’s in a spot you can’t easily see.
3. Can you have syphilis and not know it?
Definitely. That’s not just possible, it’s common. Some people don’t see the chancre at all. Others chalk it up to a shaving nick or a zit. And if the sore disappears (which it will), people assume they’re fine. Meanwhile, the infection is moving deeper into your system.
4. How long does it take for a syphilis sore to show up after sex?
It’s usually about 3 weeks after exposure, but it could be as quick as 10 days or take as long as 90. So if something shows up a few weeks after a new hookup, don’t ignore it. That timeline matches up with how syphilis works. And even if you’re not sure, testing is your best move.
5. How do I know if it’s a chancre or something else?
Honestly, chancres can look like a lot of things: razor burn, bug bites, ingrown hairs. The big difference? They usually don’t hurt and don’t leak fluid. If you’ve got a painless sore with a firm edge and no obvious cause, that’s your cue to get tested. A sore that’s too quiet is often a warning whisper, not a green light.
6. Does syphilis go away if the sore heals?
Sadly, no. The sore healing just means the infection is done with round one. It’s still in your bloodstream, gearing up for round two. Left untreated, syphilis moves into your brain, heart, nerves. Early treatment stops that. Letting it ride doesn’t.
7. What happens if you kiss someone with a chancre?
If that chancre’s in the mouth (and yes, oral chancres are a thing), kissing could absolutely spread it. Even sharing a toothbrush or lip balm might be risky in that short window. The bacteria needs skin or mucous membrane contact, kissing can do the job just fine.
8. Can I catch syphilis even if we used a condom?
Yes. Condoms lower the risk, but they don’t cover everything. If the sore is somewhere uncovered, like the scrotum, labia, or even pubic area, transmission is still possible. That’s why skin-to-skin STDs like syphilis and herpes sneak past the latex barrier.
9. If I’ve had syphilis before, can I get it again?
For sure. There’s no immunity after treatment. You could treat it perfectly and still get re-exposed later. That’s not failure, it’s just how this bacteria works. If you’re in a higher-risk group or have a new partner, regular testing keeps you ahead of it.
10. Do I really need to tell my partner if I think I have it?
Look, it’s not easy, but yes. If there’s any chance they were exposed, they deserve the info. You don’t need to give a speech. Just say, “I’m getting tested for something, you might want to too.” It’s awkward for a minute, but respectful forever.
You Deserve Answers, Not Assumptions
If you’ve read this far, it’s probably because something doesn’t feel quite right. Maybe it’s a sore you can’t explain. Maybe it’s the silence after a hookup. Maybe it’s a question that’s been eating at you quietly: “What if it’s something more?”
You’re not alone. The most common reason people delay testing isn’t laziness, it’s fear. But the truth is, syphilis is highly treatable when caught early. One painless sore doesn’t define you. It’s not a label. It’s just a signal. And the best response is clarity.
Don’t wait and wonder, get the clarity you deserve. This at-home combo test kit checks for the most common STDs discreetly and quickly. It could be the first step toward peace of mind, or the start of treatment that changes everything.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate.
Sources
5. CDC – Laboratory Recommendations for Syphilis Testing, United States
6. DERMNet NZ – Syphilis Overview with Dermatological Presentation
7. Public Health Agency of Canada – Syphilis Symptoms and Treatment
8. Wellcome Sanger Institute – Syphilis Surprises with a Worldwide Comeback
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: Janelle Wong, MPH | Last medically reviewed: October 2025
This article is just for information, not medical advice.