Quick Answer: The best time to test for HSV-1 or HSV-2 is between 4 and 12 weeks after exposure. Swab tests can detect active outbreaks earlier, while blood tests (IgG) are most accurate after 12 weeks.
What If You Don’t Have Symptoms Yet?
Here’s the cruel twist of herpes: you can have it and never know. Not just for a few days, but for life. Over 80% of people with HSV-2 don’t realize they’re infected. No burning. No sores. Just silence.
Micah, 27, had what he thought was a perfect hookup. “We used protection,” he said. “It was quick, but not careless.” A week later, no symptoms, but he’d read enough Reddit threads to know herpes could be sneaky. He tested with a mail-in panel on day 9. Negative. Relief…until a blister popped up two weeks later.
Herpes isn’t like strep throat or the flu. It doesn’t always announce itself. That means testing timelines aren’t just about symptoms; they’re about the body's immune response. If you’re symptom-free, testing too soon might miss an infection that’s still hiding from your immune system, or one that’s settled into latency before it ever flared.
Incubation, Window Periods, and Why They’re Not the Same
Let’s clear this up, because Google doesn’t always get it right. The incubation period is how long it takes after exposure for symptoms (if any) to appear. The window period is how long it takes before a test can reliably detect the infection. These timelines aren’t identical, and with herpes, they often don’t overlap at all.
Your body needs time to produce antibodies that blood tests like IgG detect. If you test before those antibodies are present, your result might be negative, even if you’re infected. Swab tests, on the other hand, only work if you have an active sore that can be sampled. No blister = no swab.
| Test Type | When It Works | What It Detects | Best For |
|---|---|---|---|
| Swab Test (PCR or culture) | 1–7 days after outbreak begins | Viral DNA | Visible sores, early infection |
| Blood Test (IgG antibody) | 4–12 weeks post exposure | Antibodies to HSV-1 or HSV-2 | No symptoms, long-term diagnosis |
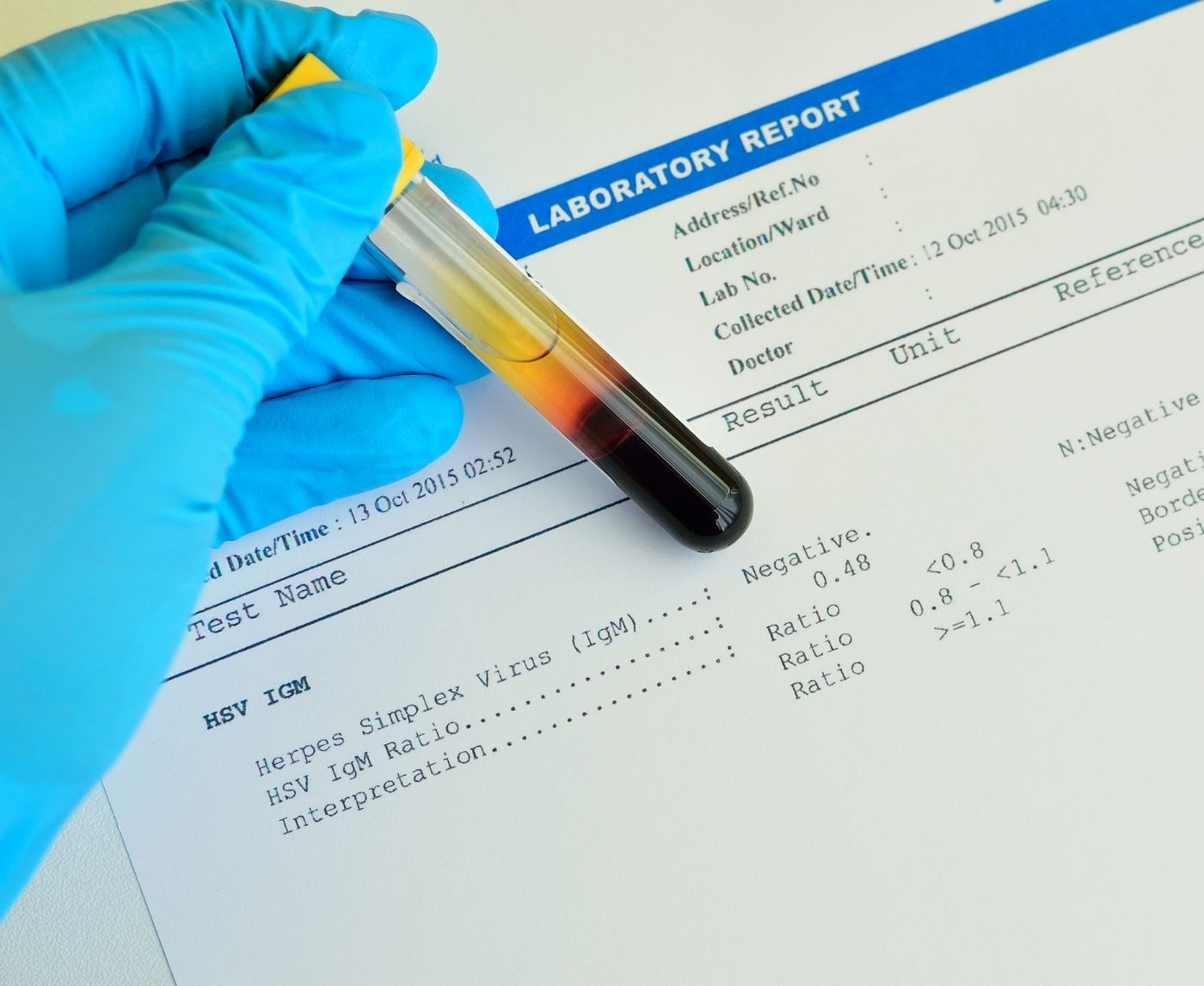
| Blood Test (IgM antibody) | Not recommended | Early antibody, but unreliable | Not advised due to false positives |
Table 1. Herpes test types by detection window and use case. Swab tests require an active outbreak; IgG blood tests are more reliable for asymptomatic cases after 12+ weeks.

People are also reading: No Symptoms, Still Infected: The Silent STD Problem
What If You Tested Too Early?
Let’s say you panicked and took a blood test one week after exposure. The negative result feels good, but how much can you trust it?
Dani, 32, had oral sex with someone who later disclosed they’d had cold sores. “I freaked out. I didn’t see anything on them at the time,” she said. She ordered an at-home test and mailed it in five days later. Negative. “I felt better...until I read that those tests don’t really work that soon.”
That’s where retesting comes in. If you test within the first 3 weeks, plan on testing again at the 12-week mark. Early tests might catch an infection if symptoms push your body into overdrive, but most accurate blood test results for herpes come after three months.
If you’re in the early window but have symptoms, pain, tingling, blisters, go for a swab. If you’re asymptomatic, wait at least four weeks (preferably twelve) before trusting an IgG result.
Check Your STD Status in Minutes
Test at Home with RemediumOral Herpes Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $33.99 $49.00
What Testing Looks Like in Real Life
Let’s strip the clinical tone and look at how this actually plays out for people. You wake up, notice a weird tingling sensation near your genitals, or maybe around your lip. You Google. Then spiral. You schedule a test, or maybe you don’t, because you’re terrified of what you’ll find.
Casey, 24, had oral sex at a party. “I didn’t even think it was risky,” she said. “But then I remembered he had a healing sore on his lip.” She took a rapid STD test at a clinic two days later, but it didn’t include herpes. “I didn’t even realize herpes needed a separate test. The nurse said unless I had a blister, it wouldn’t tell me anything.”
This happens all the time. Many standard STD panels don’t include herpes, and providers often won’t test unless you ask or show symptoms. Why? Because of the test’s limitations, and the fact that false positives can cause panic in people who may never show symptoms or transmit the virus.
Testing decisions aren’t just about risk, they’re about mindset, symptoms, and timing. If you’re anxious, testing early can offer peace of mind, but only if you understand its limitations. If you need definitive results, waiting for the optimal window is your best shot at clarity.
Herpes Type Matters: HSV-1 vs HSV-2
When people say “herpes,” they often mean genital HSV-2, but HSV-1, traditionally “oral herpes,” can cause genital infections too. In fact, genital HSV-1 now accounts for up to half of all new genital herpes cases, especially in people under 30. So yes, a cold sore can lead to genital transmission. And yes, the test can (and should) tell the difference.
The blood test most commonly used, IgG, detects antibodies specific to HSV-1 or HSV-2. Swab tests can also type the virus if the lab runs PCR with typing capability. Knowing the type matters because it affects recurrence patterns, transmission risk, and emotional stress.
HSV-1 genitally often recurs less frequently, while HSV-2 tends to have more outbreaks and higher transmission potential via genital contact. That said, either virus can live silently in your body and still be passed to others, even if you feel totally fine.
| Virus Type | Typical Location | Recurrence Rate | Detected by |
|---|---|---|---|
| HSV-1 | Mouth or genitals | Low (genitally) | IgG blood test, swab with typing |
| HSV-2 | Genitals | Higher | IgG blood test, swab with typing |
Table 2. HSV-1 vs HSV-2: Differences in location, recurrence, and detection.
Testing Methods: At Home, Clinic, or Mail-In?
There’s no “one right test” for everyone, but the best test is the one you’ll actually do. For some, that’s a fingerstick kit ordered online. For others, it’s a clinic visit in secret between classes or shifts. What matters most is that you understand how each method fits your timeline and symptoms.
At-home kits often use blood drops (IgG antibody testing). They’re discreet, fast, and easy, but don’t work well within the first month of exposure. If you’re testing for herpes specifically, make sure the kit includes HSV-1 and HSV-2. Some only test for HSV-2, which misses oral herpes entirely.
Clinic swab tests are best for people who have symptoms. They catch active infections within days of an outbreak. But walk-in clinics don’t always run PCR, which is more sensitive than a viral culture. Ask what kind of swab test they use. Also, timing matters: get swabbed within 48 hours of sores appearing for the highest chance of detection.
Mail-in labs work well for follow-up testing after early panic subsides. You collect at home, send it out, and get results in a few days. Ideal for those between 4 and 12 weeks post-exposure.
If you want clarity sooner rather than later, STD Rapid Test Kits offers discreet, private options, including combination kits that cover herpes alongside other infections.

People are also reading: Super Gonorrhea Is Spreading. Are You at Risk?
Reducing False Negatives (and False Hope)
Herpes testing isn’t perfect. False negatives happen, especially when the test is taken too early. A blood test before your immune system has produced antibodies won’t catch an infection, even if you’re already contagious. And swab tests can miss the virus if sores have started healing or if the swab doesn’t collect enough DNA.
Jay, 38, tested after an unexpected hookup on vacation. “I waited exactly 14 days, took the test, felt okay,” he said. “But I still had this weird tingling. No sores, but something felt off. I tested again six weeks later, this time, it was positive.”
To reduce your risk of missing a real infection:
, Wait at least 12 weeks for IgG testing unless you have symptoms , Use swab testing only during an active outbreak , Avoid IgM testing, which is outdated and unreliable , Consider retesting if your first test was early or negative but exposure was high-risk
Bottom line: a negative result is only as good as the timing behind it. And while early testing can ease anxiety, it shouldn’t replace a well-timed follow-up.
Check Your STD Status in Minutes
Test at Home with RemediumGenital & Oral Herpes Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $75.00 $98.00
For all 2 tests
Retesting After Exposure, Symptoms, or Treatment
So you tested. Maybe it was negative, maybe it was too early to tell. Now what?
Retesting isn’t just for peace of mind, it’s often necessary. If you tested within three weeks of exposure and had no symptoms, you’ll want to test again between weeks 8 and 12. This second test catches delayed antibody development, which is common in both HSV-1 and HSV-2.
Jordan, 41, retested after a negative test at week 4. “I was sure I was clear, but my doctor pushed for a follow-up. I almost skipped it, I felt fine. But week 11? Positive. It was a gut punch, but at least I knew.”
Retesting is especially important if:
, You had a high-risk exposure (e.g., unprotected sex, visible cold sore, recent partner with herpes) , You were tested before week 6 , You start showing symptoms after your test , You’re entering a new relationship and want definitive results , You’re immunocompromised or have a condition that delays immune response
Testing again doesn’t mean you did something wrong. It means you care enough to be sure, for yourself and your partners.
Shipping, Privacy, and That Long Wait for Results
When you’re scared, time stretches. Two days waiting for results can feel like two weeks. That’s why many people choose rapid tests or mail-in kits with fast turnarounds. But fast doesn’t mean careless, especially when the packaging is discreet, the billing is private, and the delivery feels like a secret just for you.
Leila, 22, had her test kit shipped to a friend’s address. “I couldn’t let my roommate see it,” she said. “But everything was unmarked. I opened it in the car and did the fingerstick right there.”
Every product from STD Rapid Test Kits is designed to protect your privacy. Whether you’re testing at home in the middle of nowhere, stashing your kit in a carry-on during a business trip, or hiding it in a desk drawer until you’re ready, confidentiality is built into every layer of the process.
And when you finally open your result? You’re the only one who sees it. That’s control. That’s power. That’s care.
If the Result Is Positive: What Comes Next?
Let’s say the thing you feared happens. You test positive. You see it in black and white: HSV-1 Positive or HSV-2 Positive. Your chest tightens. Maybe you cry. Maybe you stare. Maybe you feel nothing at all, for a minute.
Emilio, 29, got his result on a Monday morning. “I thought it was the end of my dating life,” he said. “But then I called my best friend, and she said, ‘Half the world has herpes. You just know now.’”
If your result is positive, start with these steps:
, Take a breath. You’re not dirty. You’re not broken. , Schedule a confirmatory test if needed (especially for early blood results). , Talk to a provider about suppressive therapy, which reduces outbreaks and transmission. , Tell partners, if you can, there are ways to do this with dignity and clarity. , Don’t rush to date or hook up again right away, give yourself space. But know that love, sex, and intimacy are all still possible.
Positive doesn’t mean forever contagious. Positive means you know. And now, you can care for yourself better than before.
If you’re ready to help a partner get tested, this combo kit includes herpes along with other common STDs. Peace of mind starts here.
FAQs
1. Can I get tested for herpes right after sex?
You can, but it probably won’t tell you much. Herpes tests don’t work like pregnancy tests. If it’s only been a few days since exposure, swab tests only work if you already have a visible sore, and blood tests won’t pick anything up yet. Your body needs time to create antibodies. Think of it like a detective showing up too early to a crime scene, there’s nothing to find yet.
2. I don’t have symptoms. Should I still test for herpes?
Yes, especially if there’s a reason to worry, like a new partner, a cold sore kiss, or unprotected sex. Most people with herpes never get classic symptoms, and that’s what makes it so easy to pass on without knowing. Testing gives you answers, not assumptions.
3. What’s the difference between HSV-1 and HSV-2 in testing?
A type-specific IgG blood test can find both types, but you should make sure your test looks for both. HSV-1 is most often found in the mouth, but it can also be found in the genitals. Genital HSV-2 is almost always present. If you know which one you have (if any), it can help you get ready emotionally and plan safer sex. It's not just about biology; it's also about peace of mind.
4. My herpes test came back negative, but I’m still feeling weird “down there.” What gives?
It might be too soon for antibodies to show up, or it might not be herpes at all. Genital tingling, irritation, and bumps can come from shaving, friction, yeast, even stress. If the feeling sticks around or gets worse, get rechecked and consider a swab test during symptoms.
5. Is it true that most people with herpes don’t know they have it?
Yes. Wildly true. Up to 90% of people with HSV-2 don’t know they’re infected. No sores, no drama, no clue. That’s why regular testing matters, especially in new relationships or if you’ve had a scare.
6. Can I give someone herpes if I don’t have an outbreak?
Yes, sadly. People who have herpes often pass it on without knowing it. This is called asymptomatic shedding. Condoms and suppressive drugs can help lower the risk, but nothing can get rid of it completely. More open communication and informed partners lead to better sex and fewer surprises.
7. What does herpes feel like the first time?
It’s different for everyone. For some, it’s intense: burning, rawness, flu-like aches, and painful sores. For others, it’s mild, just a little itch or red bump that gets mistaken for a pimple or ingrown hair. Some people never feel anything at all. That’s the herpes trick.
8. Do I need to test again if I already tested once?
Depends when you tested. If it was within three weeks of exposure and you had no symptoms, a follow-up test around 12 weeks is smart. Antibodies take time to build, and early tests can miss the signal. Think of it as closing the loop instead of guessing.
9. Can I get herpes from oral sex even if there’s no cold sore?
Yes. HSV-1 can still shed from the mouth even without a visible sore. It’s lower risk, but not zero. That’s why herpes can show up genitally even if no one had “regular” sex. This is also why “but we only did oral” doesn’t always protect you.
10. Is herpes included in standard STD testing?
Not usually. Most clinics don’t test for herpes unless you ask, and many at-home kits don’t include it by default either. Always check the panel details, or go with a test that specifically includes HSV-1 and HSV-2 if you want to be sure.
You Deserve Answers, Not Assumptions
Herpes isn’t a punishment. It’s a virus, common, misunderstood, and more emotionally charged than it deserves to be. Whether you’re still in the dark about your status, retesting after a scare, or supporting someone else through theirs, you deserve answers that are clear, private, and shame-free.
No one can make that anxious wait disappear. But the right timing, and the right test, can give you something better: truth. Not speculation. Not guessing games. Just clarity.
Don’t wait and wonder, get the clarity you deserve. This at-home herpes test kit checks for both HSV-1 and HSV-2, quickly and discreetly.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
1. CDC – Screening for Genital Herpes
2. CDC – Genital Herpes Treatment Guidelines
3. Diagnosis of Herpes Simplex Virus: Lab and Point-of-Care Testing (PMC)
4. Genital Herpes: Diagnosis, Treatment, and Prevention (PMC)
5. NHS – Genital Herpes Overview
6. Planned Parenthood – Herpes
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: Tessa Ng, FNP-C | Last medically reviewed: October 2025
This article is for information only and should not be used as medical advice.