Quick Answer: If you test for chlamydia too soon, within 0 to 5 days of being exposed, you might get a false negative. After 14 days, the accuracy goes up a lot. If you tested early, have symptoms, or had sex without protection, you should test again.
Who This Is For (And Why Timing Can Break the Test)
If you’re reading this, chances are you’re in the waiting zone, the emotional no man’s land after a risky encounter. Maybe you don’t have symptoms. Maybe you do. Maybe you're scared, angry, or just confused. Whether you’re someone in a long-term relationship who suspects a betrayal, or you just hooked up with someone new and forgot to ask about testing, this guide is for you.
It’s also for people without easy access to clinics. People living off-grid, managing chronic illness, navigating new relationships, or carrying the weight of past trauma. We see you. And we want you to know: Testing is not a confession. It’s care. And knowing how soon is too soon can make all the difference.

People are also reading: Yes, You Can Get an STD Even If You Use Condoms
How Chlamydia Rapid Tests Actually Work
Let’s strip the science down to what really matters. Most at-home chlamydia tests use one of two technologies: rapid antigen detection (used in some cassette tests) or lab-grade nucleic acid amplification tests (NAAT), which look for genetic traces of the bacteria. The rapid tests offer answers in minutes. The NAAT tests take longer but are much more sensitive.
The rapid tests don’t look for symptoms, they look for evidence of the bacteria itself. That means if the bacteria hasn’t multiplied enough to trigger the test’s detection threshold, the result will show up as negative, even if you're infected. This is what makes early testing risky. It’s not that the test is broken. It’s that your body hasn’t given it enough data yet.
Accuracy Numbers: Sensitivity, Specificity, and the Window Game
Let’s talk numbers. Chlamydia rapid tests typically have a sensitivity of 85–92% and specificity over 98%, according to manufacturer data and validation studies from public health sources like the CDC. But those numbers assume you’re testing at the right time, usually 14+ days after exposure.
If you test too early, sensitivity plummets. That means your risk of a false negative goes up, even if the specificity stays high. Here's what that looks like when broken down by timing:
| Days Since Exposure | Estimated Sensitivity | Accuracy Risk |
|---|---|---|
| 0–3 days | ~10–30% | Very high false negative risk |
| 4–7 days | ~40–65% | Moderate risk |
| 8–13 days | ~70–85% | Reduced risk, but still possible |
| 14+ days | ~90–95% | Peak accuracy |
Table 1. Estimated chlamydia test sensitivity by days since exposure. Data reflects trends from published studies and at-home kit validations. Always read individual test specs.
Window Periods Explained (And Why Symptoms Don’t Mean You're Safe)
People often mix up the incubation period (when symptoms may show up) with the window period (when a test can show that someone is infected). If you have chlamydia, the symptoms usually show up within 1 to 3 weeks. But the test may not be able to find the bacteria at its best until after the two-week mark.
This is why you can feel fine and still have an infection, or have symptoms but test negative if it's too early. Here's how it works:
| Timeline | What’s Happening in the Body | What the Test Might Show |
|---|---|---|
| Day 0 (exposure) | Chlamydia enters the body | Too early, test likely negative |
| Day 3–5 | Bacteria may begin multiplying | Still too early for reliable detection |
| Day 7–10 | Some tests may detect infection | Result may still be false negative |
| Day 14+ | Peak detection window | Most accurate result possible |
Table 2. Chlamydia window period and test detection timeline.
So, if you tested too early and got a negative result, it doesn’t mean you're clear. It means you might need to retest.
What Can Go Wrong: The Mistakes That Ruin Accuracy
It’s easy to assume the test will do all the work. But even a highly accurate chlamydia rapid test can give you the wrong result if you don’t follow the instructions carefully. These aren’t just “oops” moments, they’re the reason so many people get false negatives when they test too early or handle the kit improperly.
In our experience, the most common errors include:
| Error Type | What It Does | Why It Matters |
|---|---|---|
| Testing too early | Gives body no time to develop detectable infection | Results in false negatives, even if infected |
| Not enough sample | Swab or urine isn’t saturated enough | Reduces test’s ability to detect chlamydia |
| Contamination | Unwashed hands or improper handling | May cause invalid or misleading results |
| Reading too soon or too late | Misreads develop outside the result window | Can lead to faint lines or false results |
| Improper storage | Test kit was exposed to heat, moisture, or freezing | Degrades sensitivity of the test device |
Table 3. Common user errors that reduce chlamydia rapid test accuracy.
These mistakes aren’t always obvious. Someone might assume they followed the instructions, but testing on day four with a barely moist swab is not the same as testing on day fourteen with proper collection and timing.
“My Test Was Negative. Two Weeks Later, It Wasn’t.”
Jayden, 22, had just started sleeping with a new partner. They were careful, mostly. “There was one night where we didn’t use anything. I freaked out and tested three days later with a home kit I found online,” he recalls. “It was negative. I felt okay. Until two weeks later, I started peeing razor blades.”
Jayden’s story is common. He tested during the “dead zone”, after exposure but before the infection was reliably detectable. When he developed symptoms and went to a clinic, the NAAT swab lit up with chlamydia.
“I wish someone had told me not to trust the first test. It made me think I was fine, and I wasn’t.”
Jayden isn’t alone. The early test didn’t lie. It just didn’t have enough to detect. This is why retesting is critical if you test within the first 10 days and have symptoms, or if you’re anxious after a high-risk encounter.
Check Your STD Status in Minutes
Test at Home with RemediumChlamydia Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $33.99 $49.00
Faint Line? Here’s What It Can Mean
Few things trigger more panic than a chlamydia test with a faint, ghost-like line. Is it positive? Negative? Invalid? The short answer: A faint line in the test zone can indicate a low but detectable amount of chlamydia antigens. It often means positive, even if the line is barely there.
But it’s not always that simple. Faint lines can also result from:
- Evaporation lines: Lines that appear after the result window has closed
- Partial sample contact: Swab wasn’t inserted deeply or swirled correctly
- Kit degradation: The kit expired or wasn’t stored properly
That’s why it’s essential to read the test within the correct time window, usually 5 to 15 minutes depending on the brand, and under proper lighting. If you see a faint line, treat it as potentially positive and consider a confirmatory test.
Better to assume infection and act, than to dismiss something your body, and your test, is trying to show you.
Why Confirmatory Testing Can Be a Lifeline (Not a Punishment)
Confirmatory testing isn’t about shame, it’s about safety. If you tested too early, had a faint line, or are still experiencing symptoms after a negative rapid result, a follow-up test can give you clarity. The gold standard for chlamydia is the NAAT test, usually done at a clinic or via mail-in lab kits.
These tests have >99% sensitivity and are capable of detecting even low levels of Chlamydia trachomatis. If your at-home result was negative but you’re not convinced, don’t wait for things to get worse. You can either order a second rapid test at the right time, or go the lab route for confirmation.
Whether it’s peace of mind or a definitive diagnosis you need, both are valid.

People are also reading: Why Trich Gets Missed, And What Your Discharge Might Be Telling You
Do You Need to Retest? Here’s When and Why
If you’ve already taken a chlamydia test too early, there’s no shame in retesting, it’s often the smartest thing you can do. Here’s the general rule: If your exposure was less than 14 days ago, or you have ongoing symptoms, a follow-up test is necessary. The body needs time to build up enough bacteria for the test to detect.
Retesting is also crucial if you’ve recently finished treatment. Why? Because you don’t want to confuse a lingering infection with post-treatment bacterial remnants. Here’s a quick summary of when to retest:
| Situation | Recommended Retest Timing | Why |
|---|---|---|
| Tested less than 7 days after exposure | Retest at day 14+ | Initial test may miss early infection |
| Faint or unclear result | Repeat in 3–5 days or confirm at clinic | Ambiguous results need clarity |
| Completed antibiotics for chlamydia | Retest 3–4 weeks post-treatment | Ensure infection cleared |
| Ongoing risk or new exposure | Every 3 months or after each partner change | Prevent unnoticed reinfection |
Table 4. When to retest for chlamydia based on exposure, treatment, or risk.
Testing isn’t just a one-and-done checkbox. It’s a part of a healthy, empowered sex life. And retesting when you’re unsure is part of taking care of yourself and your partners.
“I Took Antibiotics, But I Didn’t Retest”
Sharanya, 31, got a positive chlamydia result during a routine panel. She followed her doctor’s orders: took the prescribed antibiotics and avoided sex for a week.
“I assumed I was good to go,” she says. “But I never retested.”
A month later, she developed pain and a milky discharge, classic signs of persistent infection. Her doctor confirmed she still had chlamydia, likely due to reinfection from an untreated partner or incomplete antibiotic clearance.
“I wish someone had told me to double-check. I thought the pills were enough.”
Stories like Sharanya’s remind us that chlamydia doesn’t always disappear quietly. Retesting is how you make sure your body, and your relationships, are truly clear.
Special Circumstances: What If You’re Pregnant, Immunocompromised, or Asymptomatic?
In some cases, the rules are a little different. If you're pregnant or have a weakened immune system, your doctor may suggest that you get tested sooner or more often, especially if your partner has symptoms or a known STD. In these cases, quick tests are useful, but they can't take the place of personalized care.
And if you’re asymptomatic? You’re not off the hook. Most people with chlamydia show no signs. In fact, the CDC estimates that up to 70% of women and 50% of men have zero noticeable symptoms, until the infection causes complications like pelvic inflammatory disease or infertility.
So even if you feel fine, even if you “always use condoms,” testing regularly, at the right time, is still the best move.
Check Your STD Status in Minutes
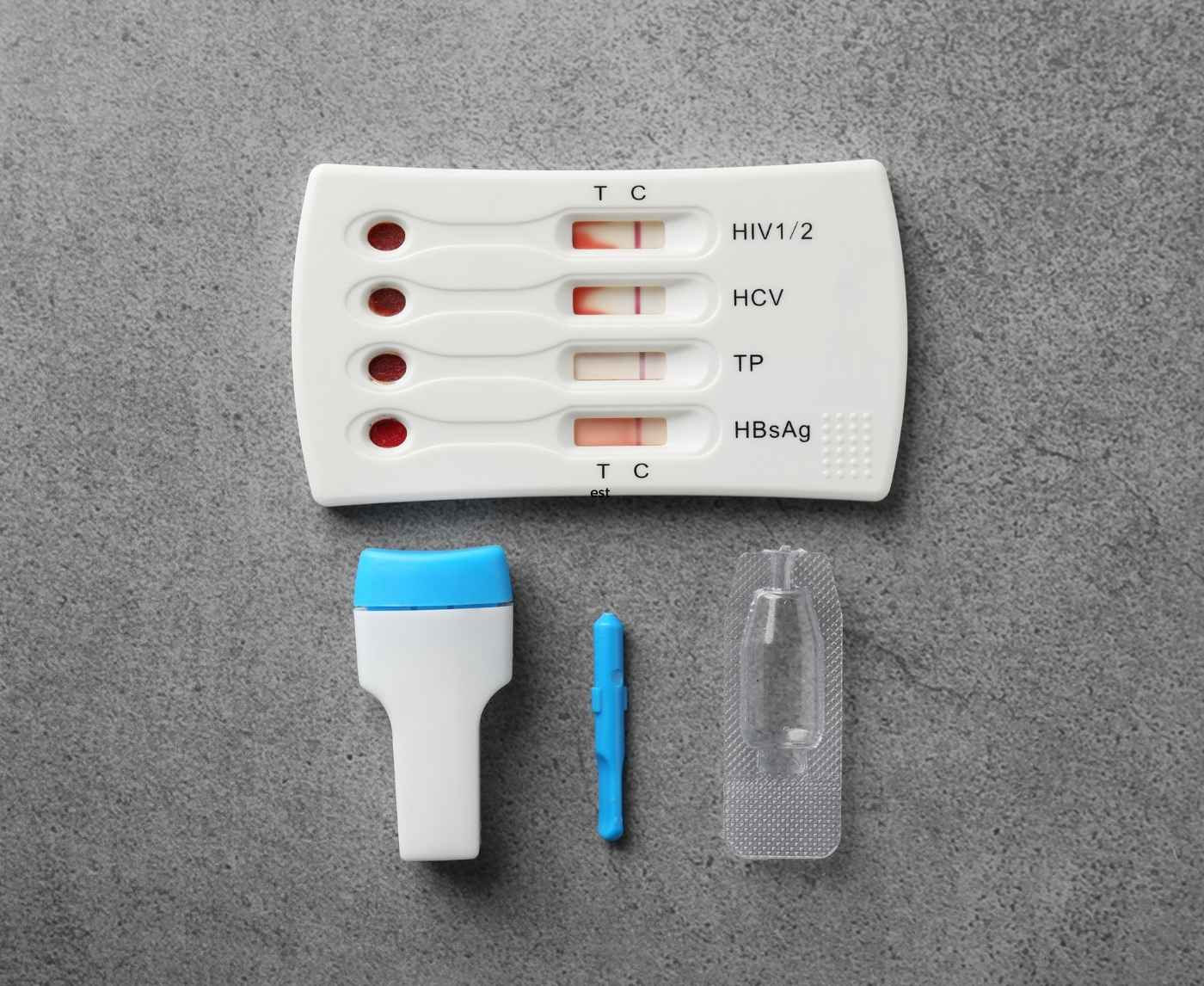
Test at Home with Remedium7-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $129.00 $343.00
For all 7 tests
FAQs
1. Can you really test too early for chlamydia?
Yes, and it's more common than you think. A lot of people test the morning after a risky hookup, out of panic, not logic. But your body needs time to incubate the infection before it shows up on a test. Think of it like a crime scene: the test can’t find clues if the suspect just got there.
2. I got a negative test 4 days after sex, am I in the clear?
Not quite. That early result is like checking your bank account before payday, it doesn’t mean the money (or in this case, the bacteria) isn’t coming. The safest bet is to retest after 14 days, even if you feel fine.
3. How long after exposure is a chlamydia test accurate?
Most rapid tests reach peak accuracy around 2 weeks after exposure. Some might catch it earlier, especially if symptoms show up fast, but 14 days is the gold standard. Earlier than that, and you’re rolling the dice.
4. What does a faint line mean on a chlamydia test?
It usually means positive, even if it’s barely visible. We get it, faint lines are confusing. But if you see any kind of test line, treat it seriously. If you’re unsure, take a photo and retest in a few days or get a lab confirmation.
5. I have symptoms but the test said negative. Now what?
First, trust your body. If you're feeling pain, weird discharge, or that "something's not right" vibe, don’t ignore it. You might have tested too soon, made a handling error, or have a different STD. Retest and consider a full panel.
6. Can I test for chlamydia during my period?
Totally. A urine-based test is fine during your cycle. Swab tests can still work, but it’s easier to get a clean sample when bleeding has stopped. If it’s day one of a heavy flow, maybe give it a couple days unless you're urgent.
7. Do I need to retest after I take antibiotics?
Yes. Even if your symptoms go away, bacteria can sometimes stick around or come back if your partner wasn’t treated. Plan to retest 3 to 4 weeks after finishing treatment just to be sure. Peace of mind > assumptions.
8. Why did my partner test negative and I tested positive?
One of you may have tested too early, used a different test, or, let’s be real, someone wasn’t fully honest. It happens. What matters is getting retested at the right time and making sure both of you are treated if needed.
9. Can chlamydia go away on its own?
Rarely, but don’t bank on it. Some studies suggest the immune system can fight it off eventually, but waiting it out isn’t safe. Untreated chlamydia can cause infertility, chronic pain, and partner transmission. Just treat it.
10. Where can I get another test quickly?
Right here. You can order a chlamydia rapid test kit that arrives discreetly, fast, and doesn’t require awkward clinic visits. Retest when the time is right, or now, if you’re ready.
Still Anxious? Take Back Control With a Simple Test
We understand. It's hard to deal with all the emotions that come with waiting, wondering, googling, and second-guessing. You can get clarity, though, and you don't need to go to a clinic to get it. At-home kits like the chlamydia rapid test kit give you privacy, speed, and peace of mind, especially when you use them at the right time.
Still unsure? You can always retest. You deserve answers, not assumptions. Whether you're confirming a faint line, checking post-treatment status, or trying to move on from a scary encounter, there’s no harm in being certain.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted six of the most relevant and reader-friendly sources.
Sources
1. Mayo Clinic – Chlamydia Overview
2. Planned Parenthood – Chlamydia Testing & Treatment
3. When do I need to test? | GetCheckedOnline (Chlamydia timing & window period)
4. Chlamydia Testing: Types, Accuracy, Timing & Necessity | STD Center NY
5. Chlamydia Investigative Guidelines (Oregon Public Health PDF)
6. STI Screening Timetable | University of Oregon (window periods & incubation)
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: L. Tran, RN, MPH | Last medically reviewed: September 2025
This article is for informational purposes and does not replace medical advice.