Quick Answer: Trichomoniasis increases HIV risk by up to 50% because it causes inflammation and microtears, making it easier for HIV to enter the body. Many people don’t realize they have it because symptoms are mild or absent.
This Isn’t Just Discharge, It’s a Trojan Horse
Trichomoniasis is caused by a microscopic parasite called Trichomonas vaginalis. It's spread through sexual contact, including vaginal and, in rare cases, anal sex. While often grouped in with bacterial STIs like chlamydia or gonorrhea, trich is neither bacteria nor virus, it's protozoan. That might sound like trivia, but it matters: most STI panels don’t even test for it unless you ask.
Here’s the catch: around 70% of people with trich show no symptoms at all. And when there are symptoms, they’re so subtle that people brush them off as yeast infections, BV, or just irritation from sex. You might feel a little vaginal or penile itching. There might be a frothy discharge with a slightly fishy smell. Or it might be absolutely nothing.
That invisibility makes it dangerous, not just to your partners, but to your immune system. According to CDC guidelines, untreated trichomoniasis increases the likelihood of acquiring or transmitting HIV. That risk isn’t theoretical, it’s biological. The infection inflames the vaginal or urethral lining, causing tiny tears that give HIV a doorway into your body. It also pulls immune cells to the surface, exactly the kind HIV targets.
In one landmark study out of Kenya, researchers found that women with trich were 52% more likely to acquire HIV. Another 2020 meta-analysis confirmed it: across global populations, trich made people 1.5 to 2.0 times more susceptible to HIV. These aren't just scary stats, they're a reality most sexual health providers aren't talking enough about.
“I felt betrayed by the silence,” said Maya, 28, who learned she had trichomoniasis only after her partner tested HIV-positive. “No one told me an itch could lead to this. No one tested me. I was just… dismissed.”
She’s not alone. Trich spreads quietly through communities, especially among women, Black and Latina populations, and queer folks, often because it’s not included in standard STI testing. You have to know to ask for it. And if you don’t? You could be living with a preventable, treatable STI that increases your HIV risk every day.

People are also reading: I Gave My Partner an STD
When Silence Is a Symptom Too
Silence is part of how trichomoniasis survives. It hides in bodies that don’t get tested. It thrives in medical systems that treat Black and brown women’s pain as exaggeration, or ignore symptoms that don’t present “severely” enough. It festers in queer communities where sexual health care isn’t always affirming or accessible. And because it’s not flashy, no painful sores, no emergency room visits, doctors often wave it off, even when people describe textbook symptoms.
Trichomoniasis doesn’t look dramatic. It looks like irritation after sex. A discharge you think is from your period. A yeast infection that doesn’t go away with Monistat. A feeling that something’s “off” down there, but not enough to take time off work to get it checked.
And even when someone does show up to a clinic, the testing gap is real. Most “full-panel” STD tests don’t automatically include trich. Clinics may prioritize chlamydia, gonorrhea, HIV, and syphilis, but skip trich unless you specifically ask. This is despite the fact that trich is estimated to affect over 2 million people in the U.S. each year, and possibly much more, since underdiagnosis is rampant.
Self.com reports that women often go years without knowing they’re infected. One anonymous contributor shared, “I got a pap smear every year. Not once did anyone mention trich. I thought I was doing everything right.” She eventually learned she’d been passing it unknowingly to partners, some of whom were also never tested.
What makes this even more frustrating is that trichomoniasis is curable. A single dose of metronidazole or tinidazole (both antibiotics) typically clears the infection. But if no one’s testing, no one’s treating. And that leaves people vulnerable to a much bigger threat: HIV.
Why HIV Loves Trichomoniasis
It’s not just that trich causes inflammation, it’s how that inflammation changes your biological defenses. The parasite damages the mucosal lining of the vagina and urethra, opening up tiny lesions. These become easy entry points for HIV if exposure happens. But it also changes the microbial balance inside the vagina, disrupting the pH and allowing harmful bacteria to flourish.
This disruption, known as bacterial vaginosis when it becomes a full imbalance, can further lower your immune response. And the immune cells your body sends to fight trich (like CD4+ T-cells and macrophages) are the exact same cells HIV uses to replicate.
One study in The Lancet found that trich made women nearly twice as likely to acquire HIV. Another explained that even brief infections, lasting a few weeks, can significantly increase HIV risk, especially if there’s repeated exposure during that time.
This is why treating trich isn’t just about clearing an STI. It’s HIV prevention.
And yet, this connection is rarely discussed outside of research papers. It’s almost never included in sex-ed. And many healthcare providers still don’t mention it unless directly asked. Which means people at highest risk, Black women, trans folks, people living in STI-endemic communities, are being left with invisible vulnerabilities, often through no fault of their own.
“No one explained the link between trich and HIV to me,” said Desmond, 31, a gay Black man who was diagnosed with both in the same year. “They just gave me pills. No follow-up. No conversation about what it meant.”
Testing alone won’t solve this, but it’s a place to start. So is naming the silence. Talking about these infections in the open. Making sure people know what’s happening in their bodies, and what’s at stake.
Check Your STD Status in Minutes
Test at Home with RemediumTrichomoniasis Test Kit
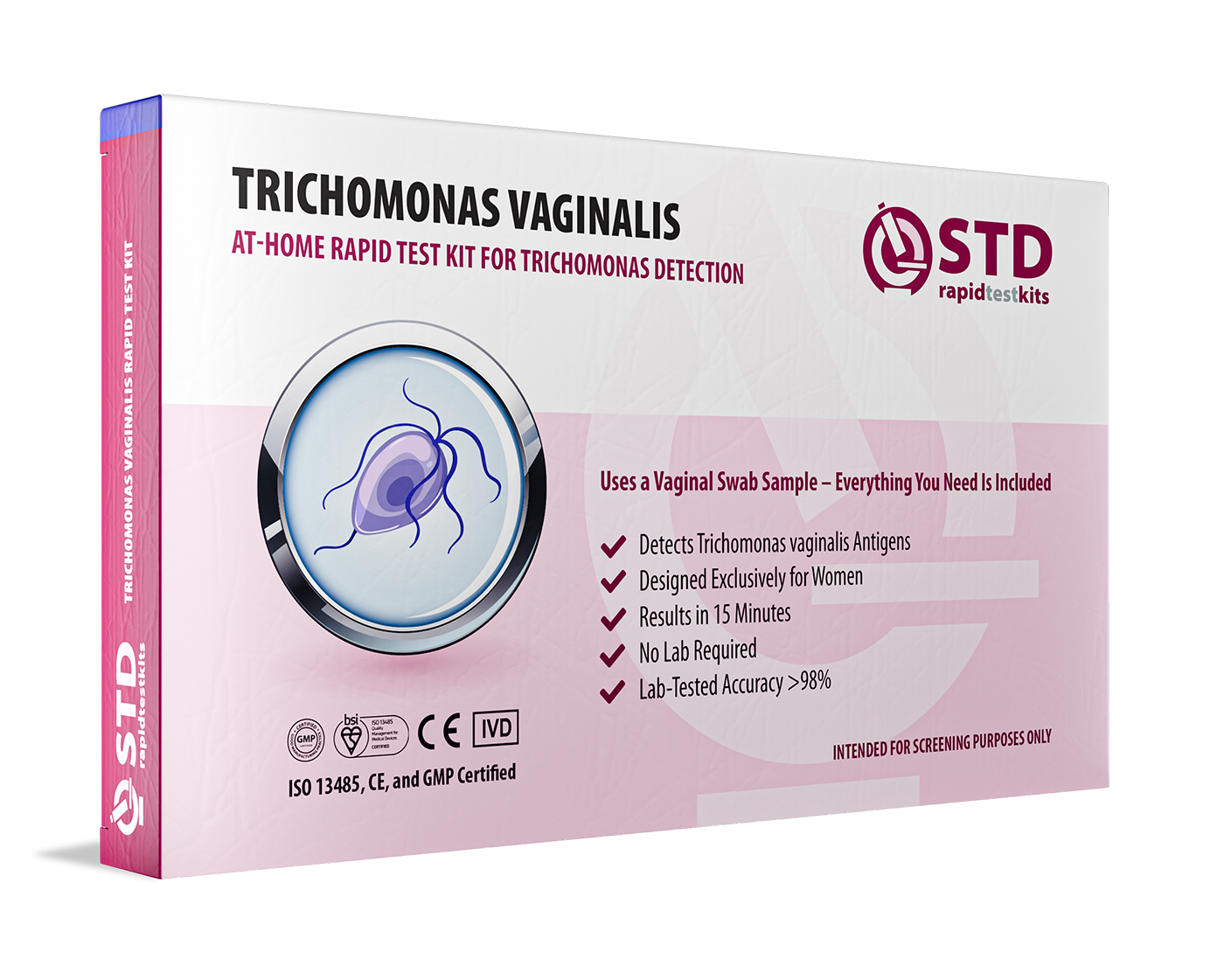
 For Women
For Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $33.99 $49.00
“Negative for Everything” Doesn’t Mean You’re Clear
There’s a myth floating around in hookup culture and even among couples trying to be safe: that a “full STD panel” means you’re good to go. But here’s the truth, most of those panels don’t include trichomoniasis. Unless you ask for it. Unless your provider knows to screen for it. Unless your symptoms are loud enough to force attention.
For cis men especially, trich is almost never tested unless you’re showing discharge or burning, which most men with trich aren’t. The parasite can live quietly in the urethra for months without causing any symptoms. During that time, it can be passed back and forth between partners like a silent tag. And every time it’s passed, it increases the chances of HIV taking hold if exposure occurs.
It’s worse in hetero contexts where women are often tested and men are not. Verywell Health notes that cis women are twice as likely to be asymptomatic, but also more likely to suffer long-term damage like pelvic inflammatory disease. And if you’re in a relationship where one partner gets tested and the other doesn’t, trich can create a loop. You think you’ve cleared it. You haven’t.
Even among LGBTQ+ folks, where there’s often more awareness around HIV prevention, trich isn’t always part of the conversation. It doesn’t show up on PrEP screening panels unless requested. It’s rarely mentioned in health apps or rapid test kits, despite how common and impactful it is.
“I thought I was doing everything right,” said Leo, 24, a queer nonbinary person who regularly tested while on PrEP. “But I kept getting this weird discharge. My doctor didn’t test for trich until I insisted. It had been months.”
That “I thought I was doing everything right” refrain comes up again and again. Because people are trying. They are getting tested. They are using protection. But they’re still vulnerable because the system isn’t designed to catch something that doesn’t scream for attention. And when symptoms do show up, they often mimic more benign issues like yeast infections or irritation from lube or toys.
There’s No Shame in Testing, Only Power
Let’s be clear: trichomoniasis isn’t a moral failure. It’s not a marker of recklessness or dirtiness. It’s a parasite that takes advantage of gaps, in protection, in testing, in awareness. And those gaps aren’t just individual. They’re systemic.
If this is the first time you’ve heard that trich can increase HIV risk, you’re not alone. But now you know. And knowing changes things.
You can ask for a test. Trichomoniasis is detectable with a swab or urine sample, and many at-home kits now include it. STD Rapid Test Kits offers combo tests that screen for trich alongside chlamydia, gonorrhea, syphilis, and HIV, giving you the full picture, not just the popular headlines.
You can treat it. A one-time antibiotic dose, taken correctly, clears the infection in most cases. But both you and your partner(s) need to be treated, or reinfection is likely. It’s not about blame. It’s about breaking the cycle.
You can protect yourself. Using condoms and dental dams during vaginal and anal sex helps reduce the risk of trich, and HIV. So does regular testing and open conversations about symptoms, even if those symptoms feel “small” or embarrassing. There’s nothing embarrassing about protecting your health.
This isn’t about fear. It’s about freedom, freedom from guessing. Freedom from silently carrying something you didn’t know you had. Freedom to have sex the way you want, with confidence, clarity, and care.

People are also looking for: Trichomoniasis: The STD No One Talks About
FAQs
1. Can trichomoniasis actually lead to HIV?
Not directly, but it definitely rolls out the red carpet. Trich causes inflammation and microtears in the genitals, making it way easier for HIV to get in if you're exposed. Think of it like leaving a window cracked during a storm, suddenly everything gets in faster.
2. How would I even know if I have trich?
Honestly? You might not. Most people don’t feel anything. If you do get symptoms, they might be vague, itching, a weird discharge, or a smell that just feels “off.” It’s one of those STIs that whispers instead of screams. But that doesn’t mean it’s harmless.
3. Wait, my last STD test was negative. Doesn’t that mean I’m fine?
Not necessarily. Most “standard” STD panels don’t include trichomoniasis unless you, or your provider, specifically ask. So yeah, you could have gotten tested, been told you’re negative, and still be carrying trich. That’s why it spreads so easily.
4. Does trichomoniasis really smell bad?
For some people, yeah. A common description is a frothy, yellow-green discharge with a fishy smell (especially after sex). But that’s not universal. Others don’t notice a thing. Just because it’s not dramatic doesn’t mean it’s not there.
5. I’ve had itching after sex, is that trich?
Could be. Could also be BV, a yeast infection, irritation from lube, latex, or just friction. But if it happens more than once or doesn’t go away fast, it’s worth testing. STI symptoms don’t always follow the rules.
6. Can guys get trich too?
100% yes. Cis men usually don’t have symptoms, maybe a little burning when they pee, maybe nothing at all. But they can still pass it on. A lot of men think they’re “clean” because they feel fine, and that’s how trich keeps making the rounds.
7. Is this just a queer or femme issue?
Not even close. Trich doesn’t care about gender or orientation. That said, it tends to hit women and queer folks harder because of healthcare bias and lack of inclusive testing. But straight dudes? You’re not immune. Don’t sleep on this.
8. If I’m on PrEP, do I still need to worry about trich?
Yes. PrEP protects you from HIV, but not from other STIs. And if you pick up trich while on PrEP, it could still cause inflammation that makes you more vulnerable to other stuff. STI testing should always be part of your sexual health routine, PrEP or not.
9. Is it embarrassing to get tested for trich?
Nope. What’s actually embarrassing is pretending your health doesn’t matter. Testing is adulting. Testing is sexy. Testing is how you show up for yourself and your partners. It’s not shameful, it’s care.
10. So what do I do if I think I have it?
Don’t panic. Ask for a trich test, or better yet, order one yourself. If it’s positive, treatment is easy: a single dose of antibiotics in most cases. Just make sure your partner gets treated too, or you’ll pass it back and forth like a bad text thread.
You Deserve Answers, Not Assumptions
If you’ve been feeling “off,” if you’ve been dismissed, if something isn’t adding up in your test results, listen to your gut. Trichomoniasis might not scream, but it matters. It’s easy to treat, easy to miss, and powerful enough to shift your HIV risk without your knowledge.
Let this be your permission to ask for better care, better testing, and better conversations about sexual health. Not because you should be scared, but because you deserve clarity. You deserve to know what’s happening in your body. And you deserve to be protected.
Don’t wait and wonder, get the clarity you deserve. This at-home combo test kit checks for the most common STDs discreetly and quickly.
Sources
1. CDC Treatment Guidelines – Trichomoniasis
2. Trichomoniasis and HIV Acquisition in Women – McClelland et al.
3. Meta-Analysis on Trichomoniasis and HIV Risk – Masha et al.
4. WHO Fact Sheet – Trichomoniasis
5. Self Magazine – STDs You Can Have Without Knowing
6. Verywell Health – HIV and Trichomoniasis in Women










