Quick Answer: Hepatitis C can live silently in the body for years without causing symptoms, often leading to liver damage or failure before it’s detected. Early testing, even if you feel fine, is the only way to know.
When You Feel Fine But You’re Not
Most people think they’d know if they had an STD. Maybe a rash, a burning sensation, something obvious. But Hepatitis C doesn’t play by those rules. In its early and even middle stages, it often causes no symptoms at all. You might feel a little tired, maybe chalk it up to stress. But under the surface, your liver could be under siege.
The CDC estimates that nearly 40% of people infected with Hepatitis C don’t know they have it. For some, it’s a virus acquired decades ago, through sex, shared equipment, or even a forgotten medical procedure. For others, the infection is recent but just as invisible. Hepatitis C isn't always passed through intercourse, but it is considered an STD due to its blood-to-blood transmission risks during sex, especially when there's mucosal damage or co-infections involved.
People like Jared don’t just exist in case studies. They're your Lyft driver, your coworker, your old roommate. One study found that among those newly diagnosed with Hep C, more than half had no symptoms at all when they tested positive. That’s why testing is less about how you feel, and more about what you don’t yet know.
People are also reading: I Used a Condom, So Why Did I Still Get an STD?
How Hep C Damages the Liver in Silence
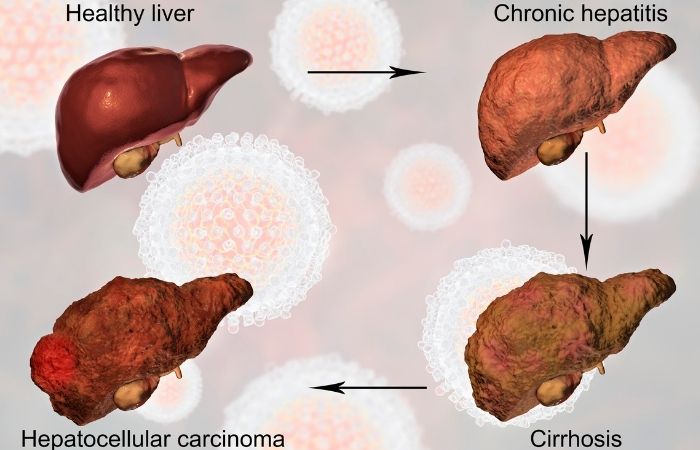
So what’s actually happening inside your body while you feel “fine”? Once Hepatitis C enters your bloodstream, it heads straight to your liver. There, it begins a slow, persistent attack, one that can last for years. Your immune system fights back, creating inflammation. Over time, this inflamed state begins to scar the liver, a process called fibrosis. If left untreated, fibrosis becomes cirrhosis. Cirrhosis can lead to liver failure, liver cancer, and death.
Here’s the brutal part: you might not feel anything until cirrhosis is already advanced. That means many people go years, even decades, before the first warning sign appears. And when it does, it’s often something vague like fatigue, joint pain, or a little yellowing in the eyes. By then, it may already be serious.
| Stage | What’s Happening | Typical Symptoms |
|---|---|---|
| Acute Infection (0–6 months) | Virus enters liver, inflammation begins | Usually none, or mild flu-like symptoms |
| Chronic Infection (6 months–30 years) | Ongoing inflammation and liver cell damage | Fatigue, joint pain, mild abdominal discomfort (if any) |
| Fibrosis | Scarring of liver begins | No symptoms or mild liver enzyme elevation |
| Cirrhosis | Severe scarring, liver begins to fail | Swelling, jaundice, confusion, dark urine, weakness |
Table 1. Progression of Hepatitis C and its symptom timeline. Most damage occurs before obvious signs appear.
Hep C isn’t rare. According to the CDC, an estimated 2.4 million people in the U.S. have chronic Hepatitis C. And the leading cause of liver transplants in the country? Hep C-related cirrhosis.
But I Don’t Inject Drugs, How Could I Have Hep C?
Here’s where the stigma gets dangerous. Most people associate Hepatitis C with IV drug use. And yes, sharing needles is a high-risk route, but it’s not the only one. You can get Hep C through sex, especially if there’s bleeding or rough contact. You can also get it from shared razors, tattoo equipment, or even medical settings where equipment wasn’t properly sterilized (more common before universal precautions were adopted).
There are also real stories of people getting infected during overseas dental visits, prison tattoos, or even hospital blood transfusions before 1992, when blood screening for HCV became mandatory. In other words, if you’re relying on outdated ideas about “who gets Hep C,” you might be skipping a test you actually need.
Hepatitis C doesn’t care if you’re sober, monogamous, or cautious. It only needs one exposure. That’s why universal screening is now recommended by both the USPSTF and the CDC for all adults 18–79, regardless of risk.
The Window Period: Why Timing Your Test Matters
Let's say you had sex without protection or did something else risky two weeks ago. You are worried, scared, and want answers right away. But it's not always easy to find Hep C right away. The window period is the time between when you are exposed to the virus and when a test can reliably find it.
Most antibody tests for Hepatitis C (which check how your immune system reacts) are accurate about 8 to 11 weeks after you were exposed. It is possible to find Hep C earlier with RNA tests, which look for the virus itself, usually within one to two weeks. However, these tests are more expensive and not as common in home kits.
| Test Type | What It Detects | Earliest Detection | Best Time to Test |
|---|---|---|---|
| HCV Antibody Test | Body's immune response | ~8 weeks | 12+ weeks post-exposure |
| HCV RNA (PCR) Test | Viral genetic material | 1–2 weeks | 3–6 weeks post-exposure |
| At-Home Fingerstick Combo Kit | Antibody (± antigen) | 6–12 weeks | 12 weeks or later for best accuracy |
Table 2. Timing and accuracy of Hepatitis C tests by method. RNA testing detects earlier but is not included in most over-the-counter kits.
If you’ve been recently exposed, testing now can give you a snapshot, but you may need to retest later. This doesn’t mean early testing is pointless. For many, it’s a starting point that relieves some anxiety and builds a timeline for follow-up.
Why Retesting Matters (Even If You’ve Tested Negative Before)
If you got a negative Hep C result after a risky encounter, you might breathe a sigh of relief, but don’t close the book just yet. Timing matters. If you tested before the window period closed, your body may not have produced enough antibodies to trigger a positive result. That’s why most clinicians recommend retesting 12 to 24 weeks after a known exposure if your initial test was negative but you’re still concerned.
Retesting also matters after treatment. Yes, Hep C is curable with today’s antivirals, but a follow-up test ensures the virus is truly gone. And because reinfection is possible, especially if you're still navigating risk-heavy situations (like unprotected sex or shared paraphernalia), it’s not a one-and-done deal.
Here’s a quick narrative: Kelsey got a tattoo on a backpacking trip and felt uneasy afterward. She tested negative six weeks later. But something still felt off. She retested at 14 weeks, and that’s when the antibody test flagged a positive. Today she’s fully treated, and says that second test saved her liver. “It wasn’t what I wanted to hear, but I’m so glad I knew.”
Use testing as a way to check in with your health, not judge your past. That mindset shift can save your life.
Can Hep C Really Be an STD?
This question confuses a lot of people, and honestly, for good reason. Hepatitis C is primarily transmitted through blood-to-blood contact, not traditional sexual fluids. But in the right circumstances, especially with mucosal trauma, anal sex, co-infections like HIV, or menstrual blood, Hep C can absolutely be sexually transmitted.
The CDC acknowledges sexual transmission as a documented route, particularly among men who have sex with men (MSM) and individuals with multiple partners. If you’ve been told it’s “not an STD,” understand that this language is outdated and misleading. The reality is more nuanced: it’s sometimes sexually transmitted, and that’s enough of a reason to include it in regular screening.
Don’t assume your partners are testing for it either. Hep C isn’t always included in routine STI panels unless specifically requested. So unless you or your partner asked for it, chances are it wasn’t checked.
If you’re reading this thinking, “Wait, I’ve never been tested for that,” you’re not alone. But you do have options. You can get tested quietly, at home, on your own timeline, the Hepatitis C Rapid Test Kit takes just minutes to use and is shipped discreetly.
Check Your STD Status in Minutes
Test at Home with RemediumHepatitis C Test Kit
 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $33.99 $49.00
What If You Test Positive?
Take a breath. A positive Hep C result is not a death sentence. In fact, it’s one of the few chronic viral infections that’s routinely curable with a short course of antivirals. Treatment lasts 8 to 12 weeks and has success rates upwards of 95%
The hardest part for many people isn’t the treatment, it’s the emotional weight. You might feel ashamed, confused, or angry. That’s normal. What matters now is acting with clarity. Find a provider who can confirm your diagnosis with an RNA test. Most health departments offer low-cost or free follow-ups. If you’re not ready to go to a clinic, use a telehealth service to start the conversation.
Then, notify any recent partners or anyone who might have shared equipment with you. You don’t need to carry this alone. Many apps and public health departments offer anonymous partner notification tools, no awkward phone calls required.
There’s power in knowing. There’s even more in treating. Start where you are, and know that a positive test is the first step toward protecting your health, not a sign that you failed.
What Makes Hepatitis C So Easy to Miss?
It’s not just you, Hep C’s invisibility is one of its most dangerous traits. Many infected people go years without lab work, or only get routine STD panels that exclude Hepatitis C unless specifically ordered. Meanwhile, general fatigue, mild nausea, or changes in appetite may be dismissed as stress, aging, or lifestyle.
Here’s the kicker: Even basic liver panels might not flag Hep C until significant damage has occurred. Elevated liver enzymes aren’t always present in early-stage infection, and some people stay within “normal” ranges for years. That’s why it’s crucial to ask for Hep C testing outright, or use a combo test at home that includes it by default.
Symptoms aren’t a reliable screening tool. Testing is.
Privacy, Packaging, and Getting Results at Home
Worried about who might see your results? You’re not alone. Many people delay or avoid testing because of shame, stigma, or simple logistics. That’s where discreet, at-home options change the game.
Today’s rapid test kits arrive in plain packaging, contain easy-to-use instructions, and deliver results in minutes. You don’t need a lab, a nurse, or a waiting room. Just a few drops of blood, a timer, and some privacy. Even better? You stay in control of what happens next, whether that’s getting treatment, retesting, or simply breathing easier.
Whether you're managing multiple partners, reentering the dating scene, or just unsure if you’ve ever been tested, it’s worth doing now. Think of it as a liver check-in. Your future self will thank you.
Not sure where to start? Visit STD Rapid Test Kits to browse discreet options for Hepatitis C and other silent infections.

People are also reading: Herpes, HIV, HPV: What Living With an STD Actually Feels Like
Why Liver Tests Alone Aren’t Enough
Maybe your doctor ran bloodwork last year and told you, “Everything looks normal.” That’s comforting, until you realize most basic liver panels don’t actually check for Hepatitis C.
Liver function tests (like ALT, AST, and bilirubin) measure how your liver is behaving, not whether it’s under viral attack. And even then, your liver can be inflamed or scarred while those numbers still fall in the “normal” range. It’s like checking if your car runs without ever looking under the hood.
Take Marcus. He was 41, doing routine health maintenance. His labs were “fine,” but he kept feeling wiped out. His doctor chalked it up to stress. It wasn’t until Marcus asked specifically for a Hep C screening, after reading a Reddit thread, no less, that the real cause emerged. He had likely been infected for over a decade.
If you’ve had abnormal liver tests in the past but no clear diagnosis, or if you've never had a Hep C test specifically, it’s time. Normal liver panels do not rule out Hepatitis C. Only a targeted antibody or RNA test can do that.
What Makes Hep C Different From Other STDs?
Unlike chlamydia, gonorrhea, or syphilis, which tend to show symptoms faster and respond to antibiotics, Hepatitis C is the slow burn of the STD world. It rarely causes early discomfort, often lingers undetected, and requires a longer course of antiviral therapy, not a single-dose cure.
It also doesn’t follow the same transmission patterns. You can’t get it from kissing, sharing drinks, or a toilet seat (obviously), but you can get it from shared sex toys, unclean tattoo equipment, or a rough hookup where blood was involved.
To make it simple:
| STD | Time to Symptoms | Curable? | Typical Treatment | Silent Damage Risk? |
|---|---|---|---|---|
| Chlamydia | 1–3 weeks | Yes | Single-dose antibiotic | Low (unless untreated for years) |
| Gonorrhea | 2–7 days | Yes | Antibiotics | Moderate (especially for fertility) |
| Herpes (HSV) | 2–12 days | No (but manageable) | Antivirals for flare-ups | Low |
| Syphilis | 10–90 days | Yes | Penicillin injection | High if untreated (neurological damage) |
| Hepatitis C | 8–24 weeks (or years) | Yes | 8–12 week antiviral course | Very High (liver damage, cancer, failure) |
Table 3. How Hepatitis C compares to other common STDs in timeline, treatment, and hidden risks.
When people ask, “Why is Hep C so scary?” this is why. It’s the one that often doesn’t hurt, until it really, really does. And by that time, it’s not just a course of pills. It might be a transplant list.
If you’ve never had a Hep C test, or don’t remember, this is your sign. Your liver’s been working overtime. Give it a chance to be heard.
FAQs
1. Can you really have Hepatitis C and feel totally fine?
Yes, and that’s exactly what makes it so dangerous. A lot of people live with Hep C for years, sometimes decades, without a single obvious symptom. No fever, no rash, no pain. Maybe a little fatigue or brain fog, but nothing you'd chase down. By the time signs like jaundice or swelling appear, liver damage may already be in play.
2. So... is Hepatitis C actually an STD?
It’s a bit of a gray area, but yes, Hep C can be sexually transmitted. It’s not as easily spread through sex as, say, gonorrhea or chlamydia, but it’s still on the radar, especially with anal sex, menstrual blood, or co-infections like HIV. The CDC includes it in STD screening for a reason.
3. When’s the best time to test for Hep C after a possible exposure?
You’ll get the most accurate result around 12 weeks after the exposure. That gives your body enough time to produce detectable antibodies. If you're testing earlier, around 3–6 weeks, you’ll want a more sensitive RNA test, but those aren’t always in home kits. When in doubt, test now and schedule a follow-up if it’s early days.
4. Do all STD test kits include Hep C?
Surprisingly, no. Many basic STD panels skip Hep C entirely unless you specifically ask for it or choose a combo kit that lists it. So if you’ve ever gotten a “full panel” and assumed you were cleared, double-check what was actually tested.
5. Can I get Hep C from oral sex or kissing?
Oral sex? It's rare, but possible, especially if there’s bleeding gums, open sores, or rough contact. Kissing? Basically no, unless someone’s bleeding directly into your mouth. Not a cute visual, but worth being honest about.
6. If I test positive, does that mean I’m doomed?
Not even close. Hepatitis C is one of the few chronic viruses that’s actually curable. Most people clear it with 8–12 weeks of antivirals. The key is catching it before serious liver damage sets in. A positive result just means: now you know, now you treat.
7. Can Hep C come back after I’ve been cured?
Technically no, the same infection doesn’t reactivate. But you can get reinfected if you're exposed again. So if you’ve been treated successfully, celebrate that, but stay mindful. Testing again after new exposure is smart, not paranoid.
8. What if I feel embarrassed to get tested?
You’re not alone. Shame keeps a lot of people stuck in silence. But testing doesn’t mean you’re dirty, reckless, or broken, it means you care about your health. That’s something to be proud of. And if privacy matters to you, at-home kits keep things quiet and in your control.
9. Do men and women experience Hep C differently?
Sometimes, yes. Women are more likely to spontaneously clear the virus without treatment, while men have higher rates of chronic infection. But neither gender is immune to the silent damage it causes, so no matter your body, testing is still critical.
10. How accurate are these home test kits anyway?
Pretty accurate, especially if you follow instructions and test at the right time. They use the same basic tech as clinical screenings. Just be sure to read results within the right time window and don’t test too early. And remember: false negatives are more likely if you rush the process.
Check Your STD Status in Minutes
Test at Home with RemediumHepatitis B & Hepatitis C Test Kit
 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $49.00 $98.00
For all 2 tests
You Deserve Answers, Not Assumptions
If you’ve made it this far, you’re probably not just reading for curiosity. Maybe you’ve had a risk event. Maybe something feels off. Maybe you’re just finally ready to know for sure. Whatever brought you here, good. You’re paying attention. You’re listening to your body, even if it’s been quiet.
This at-home Hepatitis C test delivers answers in minutes, with total privacy. No stigma. No judgment. Just truth, and a path forward.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and real-world stories to give you a practical, honest look at Hepatitis C. This article draws on over fifteen verified sources. Below, we’ve highlighted some of the most relevant.
Sources
4. Chronic hepatitis B may have no symptoms for years, while liver damage occurs silently – Mayo Clinic
5. Hepatitis C is a “silent infection” in many people, damaging liver over decades – Harvard Health
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: Dr. Alyssa Moreno, MPH | Last medically reviewed: September 2025
This article is for informational purposes and does not replace medical advice.










