Quick Answer: The UNAIDS 2025 report warns that HIV prevention and treatment services are collapsing in key areas due to global funding cuts, rising criminalization, and reduced access to PrEP and testing.
Why This Report Hits Harder Than Usual
Every year, World AIDS Day comes with a report. But this one doesn’t pull punches. Titled “Overcoming Disruption, Transforming the AIDS Response,” the 2025 UNAIDS report details how years of underfunding, political backlash, and quiet policy shifts are pushing the global HIV response to the brink. For the first time in over a decade, progress has stalled. In some countries, it's reversed.
What’s changed? For one, international funding has dipped below pre-pandemic levels. The Global Fund has seen reduced pledges. National budgets, especially in the Global South, are tightening. HIV isn’t trendy anymore in some donor eyes, even as infections persist, especially among men who have sex with men, sex workers, transgender individuals, and young women in sub-Saharan Africa.
But this isn’t just a financial crisis. It’s also a rights crisis. The report details how increased criminalization of LGBTQ+ people, sex work, and drug use is blocking access to prevention and care. In dozens of countries, anti-LGBTQ+ laws have tightened, putting clinics and outreach programs at risk. And when community-led services are forced to shut down, it’s the most vulnerable who lose.
The Cuts That Hurt Most: PrEP, Testing, and Peer Support
Ana, 27, had been on PrEP through a subsidized clinic in São Paulo. She stopped when the program ended in March. No one called to explain. No referrals were made. Her last refill simply wasn’t honored. She’s not sure if she’s still protected, and she doesn’t want to ask her new partner to get tested yet. “I don’t want to scare him away,” she says.
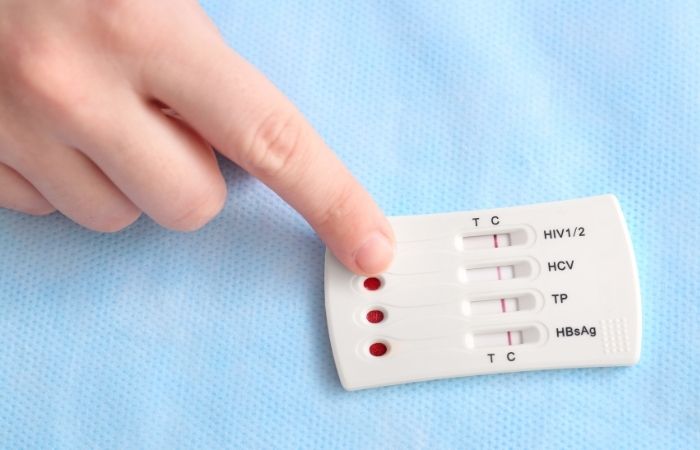
The UNAIDS report confirms that Ana’s story is far too common. Prevention tools, especially PrEP, are being defunded or deprioritized. That includes oral PrEP, injectable options, and partner services like HIV testing for sexual contacts. Where funding hasn't been cut entirely, supplies have stalled. Clinics in West Africa reported waiting months for PrEP stock resupply. Trans-led outreach in parts of Southeast Asia has paused due to lack of travel stipends and protective supplies for volunteers.
Community testing, especially peer-based or mobile, has been gutted in some areas. These programs aren’t just about diagnostics; they’re often the only entry point for people living outside traditional health systems. In rural areas, remote LGBTQ+ communities, and places with heavy stigma, peer testers often provided education, condoms, and referrals alongside rapid HIV testing. Their absence leaves a silent gap.
| Service Type | Status in 2025 | Primary Populations Affected |
|---|---|---|
| Oral PrEP Access | Decreased in 38+ countries | Young women, MSM, transgender individuals |
| Mobile/Peer HIV Testing | Suspended or reduced in 24 regions | Remote/rural populations, sex workers |
| Community Drop-In Centers | Closed or operating part-time | LGBTQ+ youth, people who use drugs |
Table 1. UNAIDS-reported service disruptions and their impact by population.
People are also reading: Does Your STD Test Really Include Everything? Check for Hep B
How Criminalization and Stigma Block Care
If your identity is illegal, it’s hard to access health care. The UNAIDS report underscores this reality. From Uganda to the United States, anti-trans laws, anti-sex work crackdowns, and increased surveillance have made many people too scared to seek testing, even when they have symptoms.
In one documented case from Eastern Europe, a health worker refused to offer an HIV test to a transgender woman, citing “moral conflict.” In Malaysia, outreach teams halted work in certain districts after police harassment escalated. In Florida, a trans-affirming health center lost its public grant, forcing patients to pay out of pocket or drop care.
UNAIDS calls this a “double bind”: legal barriers push people out of services, and their absence is then cited as lack of demand, justifying further funding cuts. It's a feedback loop that punishes those already pushed to the margins.
The report names over 130 countries that criminalize some aspect of HIV risk behavior, be it drug use, homosexuality, sex work, or HIV transmission itself. This isn’t abstract. It affects where clinics can operate, who they can reach, and whether people feel safe getting tested or staying on treatment.
Check Your STD Status in Minutes
Test at Home with Remedium6-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $119.00 $294.00
For all 6 tests
When the System Fails, Communities Still Respond
Despite the bleak headlines, the report also highlights resistance, and resilience. In Zimbabwe, a network of HIV-positive mothers has organized informal PrEP education circles after their local clinic shut down. In Mexico City, a queer-run bookstore now stocks self-testing kits in its bathroom. These aren’t formal programs, but they’re lifesaving.
Rafael, 21, works at one such grassroots effort. He started a Telegram channel where users anonymously request free HIV self-tests. The kits are mailed in plain envelopes with no return address. “We have to do what the government won’t,” he says. His project serves about 100 people a month. “We’ve caught seven new positives already this year,” he adds. Every one of them was linked to treatment through a friend-of-a-friend network.
The report emphasizes that when official services fall short, informal networks fill the gap, especially when led by those most affected. But UNAIDS warns that without reinvestment and decriminalization, this patchwork response will collapse under pressure. Volunteers burn out. Supplies run dry. And without data, policymakers assume nothing’s wrong.
HIV Self-Testing: Quiet Revolution or Desperation Move?
One of the report’s most hopeful threads is the rise of HIV self-testing. These rapid at-home kits have become more available in some regions, even as clinics close. In places where self-testing is supported by local policy, uptake is climbing fast. But the report cautions that without proper linkage to care, a positive result can leave someone stranded.
Fatima, 33, took an at-home test in the Philippines after noticing swollen lymph nodes. It came back positive. She cried for hours before Googling “where to get HIV care for free.” She found a Reddit post that led her to a WhatsApp group, which eventually connected her to an NGO clinic still operating under the radar. “It felt like chasing a ghost,” she said. “But I made it.”
The takeaway? HIV self-testing can empower people, but only if the system helps them after the result. UNAIDS urges governments to ensure that kits come with linkage pathways: a hotline, an app, a text service, something. Without that, self-testing can become another place where stigma wins.
| Region | HIV Self-Test Availability | Formal Linkage Support | Report Outlook |
|---|---|---|---|
| Sub-Saharan Africa | High in urban areas | Variable by country | Cautiously optimistic |
| Latin America | Moderate and growing | Mostly informal or community-led | Needs policy support |
| North America | High access (online and in-store) | Limited in low-income areas | Stalled by stigma and costs |
| Asia-Pacific | Mixed availability | Improving via NGO efforts | Promising but fragile |
Table 2. Regional trends in HIV self-testing access and support according to the 2025 UNAIDS report.
The Question Everyone’s Asking: Can We Still End AIDS by 2030?
It was the North Star goal for two decades: end AIDS as a public health threat by 2030. But in this year’s report, that vision feels shaky. UNAIDS doesn’t say it’s impossible, but it no longer calls it “on track.” That’s a subtle but important shift in tone.
The global targets, reducing new infections, expanding treatment, removing legal barriers, were already behind schedule before the pandemic. COVID-19, then political shifts, then economic instability layered new barriers. Now, with funding drying up and rights under attack, the 2030 goal feels more aspirational than operational.
Still, the report doesn’t give up. It outlines a pivot: not just to overcome disruption, but to “transform” the AIDS response entirely. That means rebuilding from the community up, funding with sustainability in mind, and placing human rights, not just lab results, at the center of the strategy.
This transformation requires more than medical supplies. It demands trust. It demands legal reforms. It demands that governments stop treating key populations as criminals and start recognizing them as partners.
“Ending AIDS isn’t just about the virus,” the report reads. “It’s about the systems we build, and the people we refuse to leave behind.”
What This Means If You’re Living With Risk (Or Just Living)
If you’re reading this and wondering whether any of it applies to you, the answer is probably yes. Even if you’re not part of a key population. Even if you’ve never tested positive. The report makes one thing clear: systems that fail the most vulnerable eventually fail everyone.
That means you can’t assume services will be there when you need them. Testing options might shrink. PrEP might become harder to find or afford. And if you do test positive, your care might depend on who you know, not what you need.
That’s a hard truth. But it also makes your decisions more important than ever. If you’ve had exposure, test. If your partner hasn’t tested in a while, talk. If you’re eligible for PrEP and can still access it, don’t wait. These aren’t scare tactics, they’re strategies. Because the gaps in care are widening, and waiting won’t close them.
If your head keeps spinning, peace of mind is one test away. Order an at-home HIV rapid test kit, private, fast, and doctor-trusted.
When Should You Test, and Retest?
It’s tempting to test right away after a risky encounter. That itch to know is powerful. But the UNAIDS report reminds us: testing too early can give a false sense of relief. The virus might not be detectable yet, especially with some rapid tests.
Picture this: Marcus hooked up with someone new. The condom broke. He panicked. He took a rapid HIV test the next morning, it was negative. But no one told him about the window period. Two weeks later, flu-like symptoms hit. That’s when a friend urged him to test again. The second test came back positive. He got care, but that false negative nearly delayed his treatment for good.
UNAIDS urges testing at strategic intervals. For most rapid tests, the sweet spot is about 21 to 45 days after exposure. Earlier testing is still useful, but it should be followed up. Especially if symptoms show up or if you’ve had multiple exposures. Self-testing works, but follow-up matters. And if you’re on PrEP, routine testing every three months is still the gold standard.
Retesting isn’t about paranoia, it’s about precision. The virus doesn’t play by calendar rules. Your immune response may vary. Medication can mask early signs. A retest is your insurance policy, especially when services are harder to access.
If it’s been more than three weeks and you’re still unsure, retesting could give you clarity. Don’t sit with doubt. This at-home combo STD test kit checks for HIV and other common infections with discretion and speed.

People are also reading: Babies at Risk for Hepatitis C? What Most Hospitals Still Don’t Do
What If You Test Positive, And There’s No One to Call?
This is the quiet terror that the UNAIDS report makes real. In the past, a positive result came with a roadmap: confirmatory testing, linkage to care, support groups, treatment plans. Today, in many regions, that infrastructure is eroding, or has already vanished.
Dina got her result in the middle of the night. A faint line. She wasn’t sure what it meant. No hotline answered. The clinic nearest her had been converted into a general medical office. It took her a week to find a telehealth nurse willing to see her, and that was after she lied about her gender on the intake form.
The report outlines the critical need for post-test support, especially for self-test users. But if that doesn’t exist near you, here’s what to remember:
You are not alone. HIV is treatable. Undetectable = untransmittable (U=U). If you test positive, confirm the result with a follow-up test. Then search local HIV clinics, NGOs, or telehealth services that explicitly offer support for new diagnoses. Reddit, WhatsApp groups, Discord servers, even nontraditional forums have become support networks in this fragmented landscape.
Take a breath. Take your time. But don’t give up. Treatment works. And you deserve care, no matter your background or location.
Check Your STD Status in Minutes
Test at Home with Remedium8-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $149.00 $392.00
For all 8 tests
Stigma Hasn’t Disappeared, It’s Just Evolved
The UNAIDS report doesn’t flinch from naming stigma as a core barrier. But it also explains how stigma has shape-shifted. It’s not just name-calling or rejection. It’s being ignored by the system. Being priced out of protection. Being told, implicitly, that your life is less worth saving because of who you sleep with or how you identify.
Ali, a gay man in Indonesia, hasn’t told anyone he’s positive, not even his boyfriend. He takes his meds in secret, calls them “vitamins,” and prays the clinic doesn’t stop giving them out. “I know I should be open,” he says, “but the last guy who was out… they fired him from work.”
This kind of invisibility is what UNAIDS calls the “quiet stigma”, the one that lets services disappear without protest. The one that lets deaths rise because the people affected were never visible in the first place.
Combating stigma now means more than public health posters. It means protecting rights. Funding outreach. Speaking up when your local program disappears. Buying a test for a friend who’s too scared. Posting the hotline number in a community WhatsApp group. Tiny actions can ripple when systems fail.
And if you need to act quietly? That’s valid, too. Your safety matters. Your privacy is yours. And your next step doesn’t have to be loud to be powerful.
Whether it’s a bump, a scare, or a question mark, you deserve to know. This discreet HIV test ships fast, no questions asked.
FAQs
1. Is HIV prevention really getting worse?
Unfortunately, yeah, it’s not just you noticing fewer clinics or less outreach. According to the 2025 UNAIDS report, a lot of programs that made HIV prevention easier are shrinking or vanishing, especially for people who aren’t rich, straight, or living in cities. Think: no more free PrEP at your local LGBTQ+ center, no more mobile vans doing testing outside bars. It’s not alarmist, it’s already happening.
2. What if I used to get PrEP from a clinic that’s now closed?
First, deep breath. You’re not out of options, even if it feels that way. Some places now offer telehealth PrEP or at-home delivery. It might take some digging (or asking in a queer Discord or Reddit thread), but many folks are finding creative ways to keep access alive. The system is falling apart in spots, but the community hasn’t.
3. Can I really test for HIV at home?
100%. At-home HIV tests are real, accurate, and used by millions. You swab or prick, wait a bit, and get a result privately. They’re especially helpful if you don’t feel safe going to a clinic or don’t want to explain yourself to a judgmental provider. If your test comes back positive, you’ll want to confirm with a clinic or telehealth doc, but that first test? It’s yours and yours alone.
4. What if I tested too soon after a risky hookup?
That’s super common. Your body needs a little time to build up enough viral markers for the test to catch. Most rapid HIV tests are most accurate 3 to 6 weeks after exposure. If it’s only been a few days, test if it eases your anxiety, but plan to test again later. You’re not being paranoid, you’re being smart.
5. What does the UNAIDS report actually mean for me?
Big picture? It means don't assume HIV services will be there when you need them. If you’ve been putting off testing or haven’t talked to your partner about it yet, now’s a good time. Waiting won’t make services more available, but acting now might give you peace of mind before things get harder to access.
6. Why does the report keep mentioning laws and rights?
Because in a lot of places, people are being criminalized just for existing, whether that’s being gay, trans, a sex worker, or using drugs. And when your identity is illegal, getting tested or treated becomes risky. That’s not an accident. UNAIDS is calling this out because if we don’t change those laws, we’re locking people out of care on purpose.
7. Is HIV still that big of a deal in 2026?
Yep. Treatments have come a long way, and yes, U=U is real. But new infections are still happening, especially among younger folks, queer communities, and places where testing is down. The virus hasn’t gone anywhere, and stigma still blocks people from knowing their status. We’re not done yet. Not even close.
8. I tested positive. Now what?
First off, you’re going to be okay. Really. HIV is treatable, and with meds, you can live a full life and stay undetectable (which also means untransmittable). But yeah, it’s a lot emotionally. Try to confirm your result with a clinic or telehealth provider. Then breathe. Find support. You don’t have to figure it all out in one day.
9. What if I can't find help where I live?
That’s becoming more common, sadly. But people are getting care through backchannels, queer-run mutual aid, online forums, WhatsApp hotlines, even pop-up telehealth sites. Start with a self-test. Then search smart: add words like “LGBTQ-friendly” or “free HIV care” with your city. You’re not the only one looking, and you’re not alone.
10.. Can I help someone else who might be at risk?
Absolutely. Offer to order a test for a friend. Share legit info in your group chat. Donate to a grassroots HIV org. Even just starting a “have you tested lately?” convo with a partner can be huge. Change doesn’t always look like protests, it starts in small, personal, brave ways.
You Deserve Answers, Not Assumptions
The UNAIDS 2025 report doesn’t sugarcoat the situation, and neither should we. Services are vanishing. Laws are turning hostile. People are falling through cracks they didn’t create. But in every community, there are still hands reaching out. Still people mailing test kits. Still networks linking one person to the next.
This moment demands clarity, not fear. HIV is still here, but so are tools that work. Test when you need to. Retest if you’re unsure. Use PrEP if you can. Take care of your own mental health as well as your partners.
Don’t wait and wonder, get the clarity you deserve. This at-home combo test kit checks for the most common STDs discreetly and quickly.
How We Sourced This Article: To make this guide accurate, useful, and kind, we used peer-reviewed research, reports from people who have lived through it, and the most up-to-date advice from leading medical groups.
Sources
1. UNAIDS: 2025 World AIDS Day Report – Overcoming Disruption
2. When, why, and how to get an HIV test from the CDC
3. CDC: How PrEP Helps Prevent HIV
4. Clinical Guidance for PrEP – CDC
5. HIV Testing Before PrEP – CDC
6. HIV Data and Statistics – WHO
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: M. Harris, MPH | Last medically reviewed: January 2026
This article is meant to give you information, not to give you medical advice.










