Quick Answer: Chlamydia in the eye, also called ocular chlamydia or chlamydial conjunctivitis, can mimic pink eye but usually includes thicker discharge, longer-lasting symptoms, and a connection to recent sexual exposure. It’s treatable, but requires antibiotics, not regular eye drops.
This Isn’t Just Pink Eye, And Here’s Why
Most people assume eye redness is from allergies, lack of sleep, or basic pink eye. But chlamydia can infect the eye directly, usually through accidental transfer of infected fluids to the eye. It’s one of those diagnoses people rarely expect, yet it’s more common than you’d think, especially in people under 30 and sexually active.
Chlamydial conjunctivitis can come from vaginal, anal, or oral sex, especially when semen or vaginal fluid comes into contact with the eye, or if fingers transfer bacteria after genital contact. You don’t need to have full penetrative sex to get infected. It happens during close contact, including rimming, oral sex, or touching your eye after intimate play.
Viral pink eye usually spreads to both eyes and goes away in a few days. Ocular chlamydia, on the other hand, usually starts in one eye, causes yellow-green discharge, and doesn't respond to regular pink eye treatments. If you don't treat it, it could hurt your cornea or cause vision problems that last a long time.
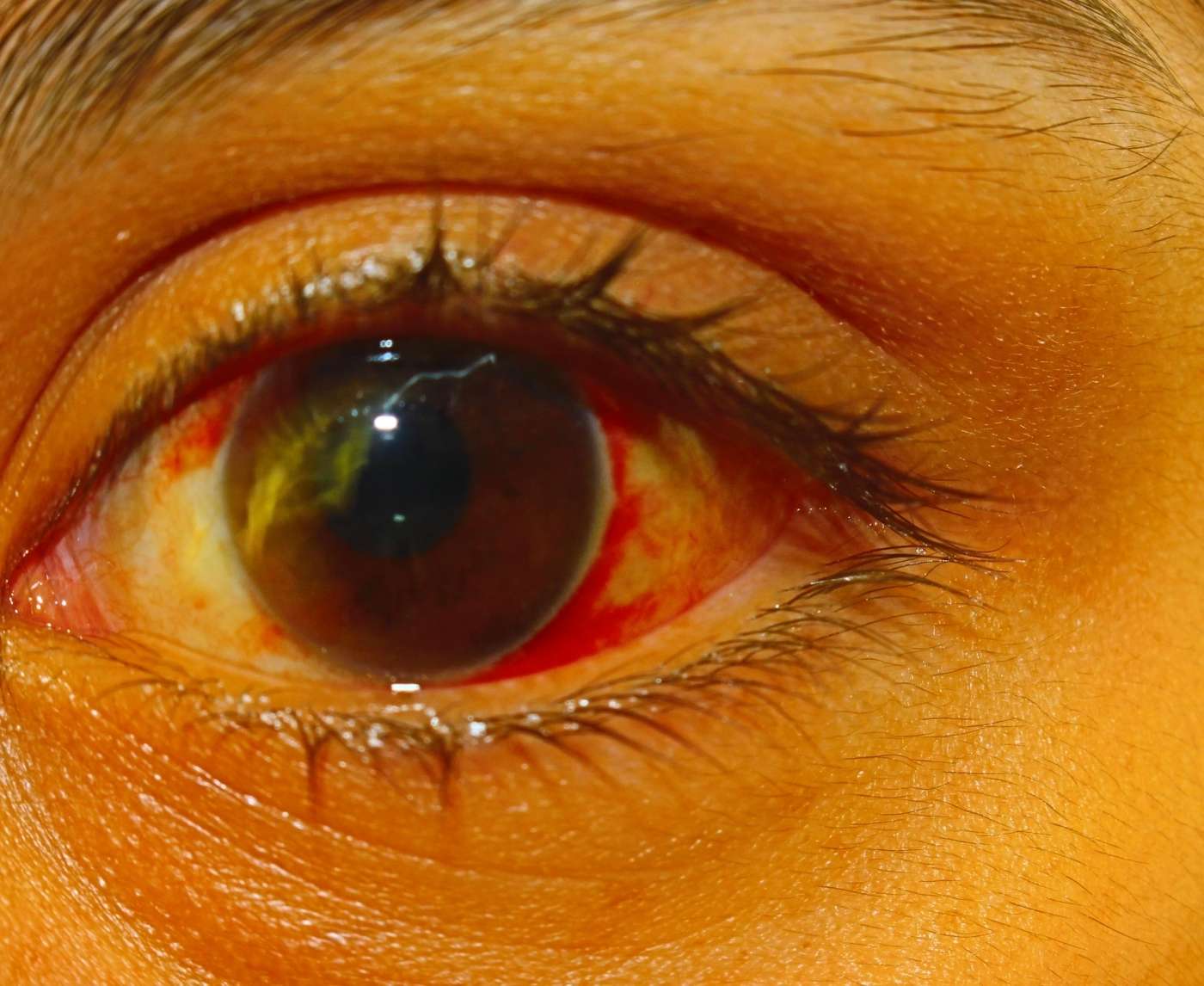
What Chlamydia in the Eye Actually Looks Like
Visual signs matter, but they can also mislead. Many cases of eye chlamydia are misdiagnosed as bacterial or viral conjunctivitis, especially in clinics unfamiliar with its presentation. Here’s what makes it stand out:
| Symptom | Typical Pink Eye | Ocular Chlamydia |
|---|---|---|
| Eye Redness | Common | Common |
| Discharge | Watery or mild mucus | Thick, yellow-green pus |
| Duration | 3–5 days | Can last over a week without treatment |
| Response to Eye Drops | Often improves quickly | No improvement, may worsen |
| Associated STD Risk | None | Recent unprotected sexual activity |
| Other Symptoms | Possible cold-like symptoms | Possible genital, throat, or rectal symptoms too |
Table 1. Key differences between regular pink eye and chlamydia-related conjunctivitis.
It’s not unusual for people with ocular chlamydia to also have genital or throat chlamydia without knowing. The bacteria can move between sites. So even if the eye is the only place showing symptoms, full testing is important.

People are also reading: Can Herpes Cause Cancer? What You Actually Need to Worry About
How It Happens: Eye Exposure and STD Risk
People don’t often think about their eyes when it comes to STDs. But chlamydia is an opportunistic pathogen, it only needs a soft, wet mucous membrane to enter the body. That includes your eyelids and conjunctiva.
One of the most common transmission routes? Accidental contact. Fingering a partner, handling a condom, or cleaning up post-sex, and then rubbing your eye without thinking. Semen or vaginal fluids that contain Chlamydia trachomatis can introduce the bacteria directly to the eye. It doesn’t take much.
In rare cases, ocular chlamydia is contracted from shared towels or makeup contaminated by infected secretions, though this is much less likely than direct transfer during or after sexual activity. Babies can also contract it during vaginal birth if the mother is infected. That’s why chlamydia screening is part of prenatal care.
There’s no shame in how it happens. The truth is: no one teaches us that STDs can show up in our eyes. So when it happens, most people either panic, or ignore it until things get worse.
Check Your STD Status in Minutes
Test at Home with Remedium6-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $119.00 $294.00
For all 6 tests
Real Talk: What It Feels Like to Have Eye Chlamydia
Jordan, 24, thought it was a bad allergic reaction. His eye was itchy and red, and he assumed pollen was to blame. But by the third day, it had morphed into a sticky, painful mess. “It literally crusted shut overnight,” he said. “I’d peel it open in the morning, and it would tear up again an hour later. I felt gross, but I didn’t think STD, I thought allergies.”
That’s the emotional curve many people follow: confusion, embarrassment, then surprise. Ocular chlamydia doesn’t come with a “you caught something” alert. It sneaks in under the radar, often after what felt like a low-risk encounter. Oral sex. A hot tub hookup. Using the same towel. The mind doesn’t always link those moments to the eye pain that appears days later.
Symptoms often include:
- A gritty or sandy sensation in the eye
- Discharge that thickens over time
- Swelling of the eyelids (especially the lower lid)
- Photophobia (light sensitivity)
- Itching or burning that worsens over several days
Because the symptoms worsen instead of resolving, most people eventually end up at urgent care or an eye doctor. Unfortunately, misdiagnosis is common without sexual history disclosure, and even when disclosed, many providers miss the link unless they’re STD-trained.
If your eye symptoms aren’t clearing with standard pink eye treatment, especially if they started after recent sexual contact, it’s time to test.
Testing and Treatment: How to Know for Sure
Unlike regular pink eye, ocular chlamydia requires specific testing, usually a swab from the inside of the lower eyelid or the discharge itself. But here’s the twist: many people also need a genital, oral, or rectal chlamydia test at the same time, because ocular symptoms often accompany (or follow) infection in another site.
Here’s how different tests compare:
| Test Type | Sample Location | Detects Ocular Chlamydia? | Turnaround Time |
|---|---|---|---|
| NAAT (Nucleic Acid Amplification Test) | Genital, oral, rectal, ocular | Yes (with proper sample) | 1–3 days |
| Rapid Chlamydia Test | Genital only | No (but may catch co-infection) | 15–20 minutes |
| Eye Culture or Swab | Lower eyelid/conjunctiva | Yes (specialized lab) | 2–5 days |
Table 2. How different STD tests detect (or miss) eye-based chlamydia infections.
Many providers recommend starting with a full STD panel that includes a genital chlamydia test, especially if the patient is sexually active and the eye symptoms aren’t resolving. While ocular samples require special handling, genital NAAT testing often reveals co-infection and guides treatment.
STD Rapid Test Kits offers discreet, lab-grade home testing for chlamydia that’s shipped in unmarked packaging. The Chlamydia Test Kit provides a quick first look, but if your eyes are involved, follow up with your provider.
Why This Isn’t Just Cosmetic: Long-Term Risks of Ignoring It
Let’s be real, when it comes to eye infections, most people reach for the same tired bottle of drops and assume it’ll go away. But untreated chlamydia in the eye doesn’t just linger, it escalates. If left alone, it can lead to a form of chronic conjunctivitis that causes scarring inside the eyelid, sensitivity to light, and even vision problems over time.
One specific concern? Trachoma, a severe form of chlamydia-related eye disease that, although rare in developed countries, can result from repeated or untreated ocular chlamydia. In extreme cases, the inner eyelid scars and turns inward, making lashes scratch the cornea. That’s not a scare tactic, that’s the reason ocular chlamydia demands medical attention, not over-the-counter fixes.
Even in less severe cases, the discomfort alone can wreck your week. These are not small problems: blurry vision, pain when blinking, and worry about how you look. They make it harder for you to drive, work, and be close to your partner. That’s why ignoring eye symptoms after sex or intimate contact isn’t just risky, it’s avoidable harm.
Can You Treat Chlamydia in the Eye at Home?
Here’s the truth: you can’t fully treat ocular chlamydia without antibiotics. But you can start the process at home with testing and symptom management until you’re prescribed medication.
The standard treatment is an oral antibiotic, usually azithromycin (a single high dose) or doxycycline (taken for seven days). These antibiotics don’t just clear the eye infection; they also treat hidden chlamydia infections in other parts of the body.
What you should not do:
- Don’t rely solely on artificial tears or pink eye drops.
- Don’t use leftover antibiotics or borrow someone else’s eye drops.
- Don’t avoid telling your doctor about recent sexual contact.
You can start with a home test like the Chlamydia Rapid Test Kit to check for genital chlamydia, which often co-exists with ocular infection. While this won’t swab your eye, it gives you the first piece of the puzzle. If it’s positive, you’re already halfway to a correct diagnosis.
After testing, you’ll need to see a provider for the full treatment plan. If you're worried about stigma or can't see someone in person, many telehealth services can prescribe antibiotics after reviewing your symptoms and test results.
Can You Spread It to Others?
Yes, you can spread ocular chlamydia, through both sexual and nonsexual contact. And not just to partners, sometimes even to roommates, kids, or anyone using the same towels or pillowcases if proper hygiene isn’t followed.
That’s not to say it’s easily airborne like a cold. But chlamydia-laced eye discharge or genital fluids left on hands, towels, or washcloths can pass the bacteria. Here’s what to do while waiting for test results or treatment:
Avoid touching your eyes, don’t share pillowcases or towels, and wash your hands frequently. If you live with others, switch to paper towels temporarily and keep your linens separate. It's not about shame, it’s about keeping others safe while you heal.
And yes, chlamydia can move from your eye to someone else’s genitals, or vice versa. A partner who touches your eye and then their own body, or who receives oral sex from someone with untreated eye chlamydia, can contract the infection. It’s rare, but real. Sex while symptomatic should be off the table until antibiotics have done their job and discharge has stopped.
What About Babies? Ocular Chlamydia in Newborns
In newborns, chlamydia in the eye is a known complication of vaginal birth from an untreated parent. It’s one of the reasons pregnant people are screened for chlamydia early on, because neonatal exposure can cause serious eye infections that lead to pneumonia or blindness if left untreated.
Ocular chlamydia in infants usually appears 5 to 14 days after birth. Symptoms include eyelid swelling, discharge, and redness. Unlike most forms of pink eye in children, this one requires prompt antibiotic treatment to prevent damage. It’s not about parental failure, it’s about untreated or undiagnosed infections that often go unnoticed due to lack of symptoms during pregnancy.
For adult readers with new babies: if your child has eye discharge within two weeks of birth, and you’ve had any untreated STDs during pregnancy, even if asymptomatic, it’s worth getting checked.

People are also reading: Yes, You Used Protection. No, That Doesn’t Mean You’re Clear
Case Study: "I Thought It Was Just a Style Thing"
Sasha, 28, worked in beauty retail and thought her red, swollen eye was a reaction to a new eye shadow palette. She switched brands, bought allergy drops, and even iced her eyelid between shifts. But the symptoms kept cycling. “It would clear for a day or two, then flare up again,” she said. “I never even thought to connect it to sex.”
It wasn’t until she got a routine STI panel, unrelated to the eye stuff, that the clinic called and told her she was positive for chlamydia. A week later, still dealing with eye pain, she brought it up to a nurse during her treatment appointment. That’s when the pieces came together. The nurse explained that chlamydia can infect mucous membranes anywhere, mouth, rectum, urethra, and yes, eyes.
After finishing her doxycycline, the symptoms finally cleared for good. “I felt like a walking PSA,” Sasha joked. But she’s not wrong, her story highlights what so many people don’t know: your eye might be the first place chlamydia shows up.
Prevention: What Actually Works
The best way to prevent eye chlamydia is surprisingly simple: hand hygiene. Wash your hands after any intimate contact, especially before touching your face or handling contact lenses. If you’ve had sex, protected or not, clean your hands before rubbing your eyes or removing makeup.
Condoms and dental dams help, but because chlamydia can be present in fluids around the genitals, full prevention also involves awareness. Don’t share towels. Don’t reuse pillowcases. Don’t let someone’s fluids come into contact with your eyes, even if things are consensual and hot in the moment. Enthusiasm should never outweigh hygiene.
Also, test regularly. Even if you don’t have eye symptoms, you could be carrying chlamydia elsewhere. Catching it early, through a product like the Combo STD Test Kit, helps you avoid surprise flare-ups in sensitive areas like the eyes.
Check Your STD Status in Minutes
Test at Home with Remedium8-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $149.00 $392.00
For all 8 tests
The Emotional Side: Shame, Surprise, and Relief
There’s a particular kind of shame that hits when you find out your eye infection is actually an STD. It doesn’t help that “ocular chlamydia” sounds almost made-up, or like a punchline. But here’s the truth: bodies are messy. STDs don’t follow our logic or rules. They follow biology, and mucous membranes.
If you’re dealing with this, you’re not dirty, irresponsible, or alone. You’re one of thousands each year who unknowingly contract a treatable infection in an unexpected place. The relief most people feel after diagnosis isn’t just about starting treatment, it’s about finally knowing.
You don’t have to stay stuck in worry, guessing, or eye-drop roulette. You can take one test and begin a clear, evidence-based path to healing. Confidential, fast, and shame-free.
Still wondering if your symptoms line up? Start here with an at-home test, and take your power back.
FAQs
1. Wait, chlamydia can show up in your eye?
Yep, and it catches people off guard all the time. Most of us are taught to look out for burning when we pee, not burning when we blink. But if infected fluids like semen or vaginal discharge get into the eye (through fingers, towels, or just chaotic sex logistics), the bacteria can set up shop right there. It’s called ocular chlamydia, and it’s very real.
2. How would I even know if it’s that and not just pink eye?
Great question, because they look almost identical at first. But here’s the deal: pink eye usually clears up in a few days with drugstore drops. Ocular chlamydia just… doesn’t. It hangs around, gets gunky, and often affects only one eye. Think thick yellowish discharge, swollen eyelids, and zero improvement after a few days. If your eye’s throwing a tantrum and you had recent sexual contact, this should be on your radar.
3. Do I have to have sex to get it in my eye?
Not necessarily. It’s not about the act, it’s about fluid contact. You could finger someone, then rub your eye. Or receive oral and wipe your face without washing your hands. Some folks have even caught it from shared towels. Sex may be the context, but touch is the vehicle. That’s why this one’s sneaky.
4. What does it feel like, besides gross?
Honestly? Gritty, sticky, and frustrating. People say it feels like sand in the eye, or like the lashes are glued together. It can hurt to blink, and light might start feeling aggressive. One person described it as “having a wet Q-tip stuck behind my eyelid.” Not fun, but treatable.
5. Can I use regular eye drops to treat it?
Unfortunately, no. Over-the-counter drops might soothe the sting for an hour, but they won’t kill the bacteria. This isn’t allergies or basic conjunctivitis. You’ll need oral antibiotics, usually azithromycin or doxycycline, to fully clear it. Think of eye drops like a cool washcloth when you have the flu: comforting, but not a cure.
6. If I test positive genitally, does that mean my eye is infected too?
Not always, but it’s a strong hint. If you’ve got genital chlamydia and your eye is acting up, they could be connected. The bacteria can migrate via fluids or fingers, so dual-site infection is totally possible. That’s why comprehensive testing matters, and so does telling your doctor the full story, even the awkward parts.
7. Is it contagious? Like, can I give it to my roommate or baby?
There’s no need to panic, but yes, it’s possible. Eye gunk can carry bacteria, and if it gets onto towels, bedding, or hands that touch someone else’s eyes or genitals, there’s a risk. Wash your hands obsessively. No towel-sharing. No makeup-lending. Your roommate will thank you. And babies? Keep them safe by keeping your face to yourself until you’ve been treated.
8. Can I still wear contacts?
That’s a hard no. Contacts trap bacteria, irritate the conjunctiva, and slow healing. They also get slimy and uncomfortable fast. Switch to glasses until you’ve completed treatment and your eye is fully back to normal. Your cornea deserves better right now.
9. Should I tell my partner even if the symptoms are just in my eye?
Absolutely. Eye chlamydia isn’t some random fluke, it’s a sign the bacteria is present in your system. That means your partner could have it too, possibly with zero symptoms. Giving them a heads-up isn’t just kind, it helps stop the boomerang effect of reinfection. And no, it doesn’t have to be a scary convo. “Hey, I found out I had an eye infection from chlamydia, just wanted to let you know so you can test too.” That’s it.
10. How long does it take to clear up after treatment?
Most people feel relief within a couple of days of starting antibiotics, but you should still complete the full course. Discharge, redness, and swelling usually fade within a week. And remember, just because your eye looks better doesn’t mean the infection is gone from the rest of your body unless all sites were tested and treated.
You Deserve Answers, Not Assumptions
Eye infections are annoying. Eye infections that won’t go away, respond to nothing, and make you question your last hookup? That’s a whole new level of stress. But stress doesn’t have to run the show. You don’t need to live in Google searches, Reddit rabbit holes, or denial loops.
Whether it’s one red eye or one suspicious symptom, there’s one way to stop the spiral: get tested. You’re not being dramatic. You’re being proactive. You’re protecting your partners and yourself. And if it turns out you do have ocular chlamydia? You can treat it, fast and fully, with the right steps.
Don’t wait and wonder, get the clarity you deserve. This at-home combo test kit checks for the most common STDs discreetly and quickly.
How We Sourced This Article: We used the most up-to-date advice from top medical groups, peer-reviewed research, and reports from people who have lived through the issues to make this guide useful, kind, and correct.
Sources
2. World Health Organization – Trachoma Facts
3. Planned Parenthood – Chlamydia Overview
4. Chlamydia Trachomatis Infection — Symptoms and causes (Mayo Clinic)
5. Chlamydial Infections — STI Treatment Guidelines (CDC)
6. Conjunctivitis (StatPearls) — NIH Bookshelf
7. Clinical Overview of Conjunctivitis (CDC)
8. Adult Inclusion Conjunctivitis (Merck Manuals)
9. Adult Inclusion Conjunctivitis Diagnosed by PCR — PMC
10. About STI Risk and Oral Sex (CDC)
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: L. Morgan, NP-C | Last medically reviewed: January 2026
This article is meant to give you information, not to give you medical advice.