Quick Answer: Gonorrhea doesn’t always mean someone cheated. It can stay asymptomatic, go undiagnosed for months, or be misread in testing. Faithfulness doesn't make you immune, and a positive test doesn’t prove infidelity.
It’s Not Always About Cheating, Here’s Why Gonorrhea Can Show Up Anyway
Gonorrhea carries a cultural weight most STDs don’t. There’s a snap judgment: if it shows up, someone must have strayed. But biology isn’t a gossip columnist, it’s more complicated than that. The bacterium that causes gonorrhea, Neisseria gonorrhoeae, can live in the body without obvious symptoms for weeks, sometimes months. Especially in people with vaginas, infections can go unnoticed, spreading silently between partners who may genuinely believe they’re STD-free.
Case in point: Rafael, 32, had been in a monogamous relationship for over a year when his partner tested positive during a routine check-up. “I felt blindsided,” he told us. “But when I tested, I was positive too. And neither of us had cheated. We traced it back to a hookup I had just before we started dating. I’d never gotten tested because I had no symptoms.”
What stories like Rafael’s reveal is how dangerous silence can be. Gonorrhea doesn’t need drama to exist, it thrives in the in-between. In the assumption that no symptoms = no infection. In the hope that “it’s probably just a UTI.” In the three-month gap between a fling and a new relationship, when everyone’s trying to start fresh and no one wants to talk about testing.
Why the Test Might Not Be Telling the Whole Story
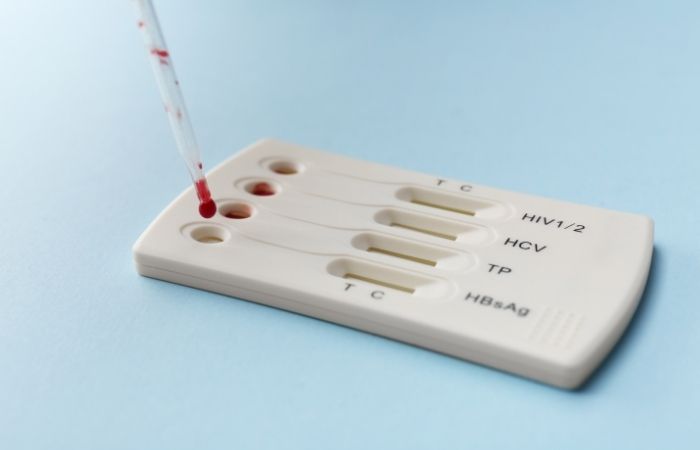
There’s another piece of this that rarely gets talked about: testing isn’t perfect. While modern gonorrhea tests are highly accurate, they're not infallible. False positives and negatives, though rare, can and do happen. And depending on when you test, how the sample is collected, and where the infection is located (throat, rectum, urethra), results may miss or misread an active infection.
That's why it's important to know about timing, accuracy windows, and test types when you find out you have gonorrhea. A common mistake? Testing too soon after potential exposure. This can result in a false negative, leading people to think they're in the clear, only to test positive weeks later, which can spark unfair accusations.
Let’s break it down.
| Test Type | Sample Collected | Accuracy Window | Risk of False Result |
|---|---|---|---|
| NAAT (Nucleic Acid Amplification Test) | Urine, vaginal, rectal, or throat swab | 7 to 14 days post-exposure | Low, but possible if too early or wrong site |
| Culture Test | Swab from suspected site | 3 to 7 days post-exposure | Moderate; more likely to miss throat/rectal infections |
| At-Home Rapid Test | Urine or swab (user-collected) | 14+ days for best accuracy | Depends on user handling and timing |
Table 1. Gonorrhea test types, samples, and when results are most reliable. Even highly accurate tests can mislead if taken at the wrong time or from the wrong site.
So if your partner has tested positive and you haven’t, or vice versa, it doesn’t automatically mean betrayal. It could mean different exposure dates. It could mean the infection was dormant. It could mean someone was tested too early, or didn’t test the right body site. It could mean exactly what no one wants to believe: the test isn’t a lie, but it’s not the full truth either.

People are also reading: HIV Rates Are Shifting, What That Means for Testing From Home
“But We’re Monogamous”, When Love and Lab Results Collide
It’s hard to overstate the emotional bomb that a gonorrhea result can drop into a relationship built on trust. When one partner is positive and the other swears they’ve been faithful, it feels like a math equation that doesn’t add up. But monogamy isn’t a test result, it’s a dynamic, and human bodies aren’t calculators.
Consider Nina, 29, who tested positive for gonorrhea during a routine STI screening for her new IUD. “I hadn’t slept with anyone but my girlfriend in eight months,” she said. “And when I told her, she got quiet. Then angry. She thought I was accusing her. But I was just scared.” Her partner tested negative, twice. And yet, the truth was more complex. Nina’s infection likely dated back to a brief period of unprotected sex with a previous partner, and her body had quietly harbored it all that time. Meanwhile, her current partner hadn’t been exposed in a way that led to transmission. It was science, not scandal.
Here’s what complicates things further: gonorrhea doesn’t always transmit from one encounter, even with unprotected sex. The odds vary by sex act, infection site, and individual immune response. Some people carry it in the throat after oral sex and never know. Others pass it during vaginal or anal sex without a clue. And even with repeated exposure, it’s possible for only one partner to test positive.
In cases like Nina’s, the key was communication. Not accusation. They retested. They talked to a provider. They chose to move forward. “It shook us,” she said, “but it didn’t break us.”
Check Your STD Status in Minutes
Test at Home with Remedium8-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $149.00 $392.00
For all 8 tests
Can Gonorrhea Really Stay Dormant for That Long?
This is one of the most misunderstood things about gonorrhea: the idea that it “shows up out of nowhere.” While it doesn’t go dormant in the way viruses like herpes do, it can absolutely linger in the body without obvious symptoms, especially in the rectum or throat. Some infections remain hidden for months before being discovered, often during unrelated medical exams or routine STI screening.
The medical term here is “asymptomatic carriage.” It’s more common than most people realize. According to the CDC, many people with gonorrhea, especially women and people with receptive anal sex, never notice symptoms at all. That means an infection can sit quietly in the body, doing damage or waiting to be unknowingly passed along, long before a test ever picks it up.
If that sounds terrifying, here’s the reassurance: routine testing can catch it before it spreads or causes long-term issues. And treatment is straightforward, typically a single injection of ceftriaxone, sometimes paired with oral antibiotics if other infections are suspected. The stigma is often the hardest part to treat, not the disease itself.
Let’s look at what this might mean for partners who haven’t tested yet.
| Scenario | Possible Explanation |
|---|---|
| Partner A is positive, Partner B is negative | Exposure timing, natural immunity, or false negative in Partner B |
| Both partners positive, but only one has symptoms | Common; many infections are silent in one partner |
| Symptoms show up weeks after a new relationship began | Undiagnosed prior infection from a past partner |
| Retesting gives different results | Testing window, site mismatch, or lab sensitivity differences |
Table 2. Common gonorrhea diagnosis outcomes in couples and why they don’t always match our assumptions.
So You Tested Positive, Now What?
First: take a breath. Testing positive for gonorrhea doesn’t mean you’ve been reckless, and it doesn’t mean your relationship is doomed. What it does mean is that your body needs care, and your next steps matter. Gonorrhea is one of the most treatable STDs. With the right antibiotics, most people are cleared in days. But what you do immediately after that diagnosis sets the tone for your recovery, your relationships, and your peace of mind.
If you were tested at a clinic or through an at-home kit like those from STD Rapid Test Kits, the first step is usually confirming that the result was accurate. If the test was done before the 7–14 day accuracy window, or if it was from a single site (like urine only, without rectal or throat testing), your provider might suggest a second test. Especially if you’re asymptomatic but positive, or if you’ve had a recent partner test negative despite symptoms. Retesting isn’t about doubt, it’s about detail.
You’ll also need to talk to a provider about treatment. In most cases, you’ll receive a one-time injection of ceftriaxone, which clears the infection quickly. But don’t stop there. You’ll also need to avoid sex, oral, vaginal, or anal, for at least seven days after treatment. If your partner hasn’t been treated too, there’s a high risk you’ll just pass the infection back and forth, unknowingly.
This is where a lot of people hit the emotional wall. Because treatment is easy, but the conversations aren’t.
What to Say to a Partner When You’re Both Staring at a Positive Test
“You probably think I cheated.” That’s how Emily, 38, began the conversation with her husband after testing positive. She hadn’t. But she knew what the result would sound like. He stared at her in silence. Then said, “Did I?” That was the moment they both realized how little they’d talked about STDs in their relationship. They’d tested when they got together, sure, but never since. That was five years ago.
Here’s the truth: STDs don’t care how in love you are. They don’t care about your promises. They care about biology. And if no one’s tested since the last relationship, then something like gonorrhea can enter a monogamous dynamic and feel like betrayal, even when it’s just bad timing and biology colliding.
In moments like this, it helps to get medical language involved. Not to deflect, but to reframe. Saying, “The test showed I have gonorrhea, but that doesn’t mean I just got it,” or “Let’s both get retested and talk to a provider before we panic,” can keep the conversation grounded. It’s not a courtroom. It’s a partnership, and partnerships weather hard truths by anchoring in facts, not fear.
If you're struggling with how to talk to your partner after a positive test, there are also anonymous partner notification options offered by many health departments. You can send a text or email without disclosing your name, letting them know they should get tested. Some at-home testing providers even include this option directly within their kits or portals.
Why Retesting Matters (Even After Treatment)
Here’s something most people don’t realize: treating gonorrhea doesn’t always mean you’re totally in the clear. If your partner hasn’t been treated, you can be reinfected within days. If you’ve had unprotected sex with others since the infection, there could be other STDs present that weren’t caught on the first test. And if you’re immunocompromised, or took antibiotics incorrectly, treatment might not fully eliminate the bacteria.
That’s why the CDC recommends a “test-of-cure” follow-up for certain patients, especially if rectal or pharyngeal (throat) infections were involved. Even for those who don’t fall into that category, many providers encourage retesting about three months after treatment to catch reinfection. Not because they doubt you, but because this infection can recur, and reinfection is common if all partners aren’t on the same page.
Let’s say you were treated last week. You’re symptom-free. But your partner never tested. You get back to your normal routine, sex included. Two weeks later, they test positive. Now you’ve both been exposed again. That’s why syncing your care is critical.
If you’ve already tested but want to confirm you’re clear after antibiotics, an at-home Gonorrhea Rapid Test Kit can offer quick reassurance. Just make sure to wait at least 14 days post-treatment for the result to be meaningful.
People are also reading: Think You’re Safe? Here’s How Gonorrhea Actually Spreads
What If the Test Was Wrong?
It's not common, but it can happen. Gonorrhea tests can give false positives because of contamination, mistakes made in the lab, or some other health problems. If you tested positive but had no symptoms and no risk of exposure, a provider might suggest a second test, especially if the first test was a quick one instead of a lab-based NAAT. On the other hand, false negatives can happen if the wrong place was swabbed or the test was done too soon after exposure.
If your clinic test is positive but your home test is negative, for example, the best test is a lab-based NAAT, which should be done again at least 7–14 days after you think you were exposed. It's important to interpret all test results with your history in mind: symptoms, exposure timelines, sexual practices, and partner history. That’s why context matters as much as the cassette line or digital readout.
It’s okay to ask your provider: “Could this be a false result?” It’s okay to retest. What’s not okay is letting shame or doubt silence your voice. Testing is about information, and every test tells a part of the story. The whole picture? That’s built over time, with communication, retesting, and support.
Check Your STD Status in Minutes
Test at Home with Remedium6-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $119.00 $294.00
For all 6 tests
How to Protect Yourself (and Your Partner) Moving Forward
Whether you decide to stay together, take space, or start new sexual relationships, this experience can be a turning point, not a stopping point. Testing regularly, using condoms, reducing your number of concurrent partners, and having honest conversations before you get intimate are all ways to rebuild safety.
But more than any of those steps, the most powerful thing you can do is remove shame from your story. Because gonorrhea isn’t a moral failure. It’s an infection. It responds to antibiotics, not judgment. It doesn’t care about how many partners you’ve had, how long you’ve been faithful, or how careful you thought you were. And it can happen to anyone, yes, even in “monogamous” relationships.
So if your head is spinning and your heart is heavy, here’s your reminder: you deserve clarity. You deserve care. And your story is still yours to shape. Not in whispers or accusations, but in facts, action, and healing.
Want to retest from home? STD Rapid Test Kits offers discreet, fast options for checking again when you're ready. No shame. No clinic waiting room. Just answers.
FAQs
1. Can you seriously get gonorrhea without cheating?
Yes, 100%. This is one of the most common panic questions we hear, and the answer is not only yes, but it happens more than people think. Gonorrhea can stay in your system with zero symptoms, sometimes for months, and then show up during routine testing. It’s not a lie detector. It’s a bacteria. And it doesn’t care if you're faithful, it only cares if it found a warm place to live.
2. My partner tested positive and I didn’t. Does that mean they cheated?
Not necessarily. This kind of mismatch is common and confusing. It could be different test timing, different exposure dates, or even just different body responses. Maybe they were tested too early before and got a false negative. Maybe your immune system suppressed it. Maybe theirs didn’t. Bodies are weird. Trust gets tested, sure, but the test result isn’t always the betrayal people think it is.
3. Is it possible to carry gonorrhea and not know it?
Oh, absolutely. Especially for people with vaginas or people who’ve had anal or oral sex. Gonorrhea loves to hang out in the throat and rectum without making a scene. No burning, no discharge, nothing dramatic, just quietly chilling until a test happens to catch it. That’s why regular testing matters even when you feel fine. Silence doesn’t mean safety.
4. What if I tested positive but haven’t had sex in months?
That can still make sense. Gonorrhea doesn’t always show symptoms right away, and some infections linger undetected. We’ve seen cases where people test positive six months after their last partner, especially if that past partner never got tested. This is why testing with every new relationship (or situationship) is so critical, even if it “ended ages ago.”
5. We’re monogamous. Should we both still get tested regularly?
Yes. Monogamy is a relationship choice, not an STD shield. People enter relationships with past exposures. People sometimes think they tested but didn’t cover all sites (like throat or rectal). Or, honestly, sometimes trust breaks. Regular testing is just relationship hygiene. Like brushing your teeth, but for your sex life.
6. Could my test be wrong?
It’s rare, but not impossible. A false positive can happen due to lab mix-ups, contamination, or, very rarely, cross-reactivity. But false negatives are more common, especially if you tested too early or didn’t swab the right site. If something feels off, it’s okay to test again. You’re not being paranoid, you’re being thorough.
7. Does oral sex really count for STDs?
It does, and gonorrhea especially loves the throat. It can be passed from someone with a throat infection (who might not even know they have it) to their partner’s genitals, and vice versa. It’s why throat swabs should be part of routine STI panels for anyone having oral sex. And if you’ve never had one, it might be time to add it to the mix.
8. What's going on with reinfection?
Reinfection is like a boomerang, it happens when one partner gets treated but the other doesn’t. So even if you took your meds and feel fine, sleeping with a partner who still has the infection means you’ll just get it again. Think of it like ping-pong. You both have to step away from the table, get treated, and then come back clean.
9. How long should I wait before having sex again?
Most doctors say wait seven days after finishing treatment, and make sure your partner is treated too. That gives the antibiotics time to clear the infection and lowers your risk of passing it back and forth. It’s annoying to hit pause, but it’s better than starting a cycle of reinfection that’ll make both of you even more frustrated.
10. Can you test for gonorrhea at home?
Yes, for sure. The Gonorrhea Rapid Test Kit and other home tests are quick, private, and accurate when used correctly. They're great for retesting after treatment, checking on a new partner, or just feeling better without having to go to a clinic. You can do experiments in your bedroom. And your privacy stays your own.
You Deserve Answers, Not Assumptions
Gonorrhea doesn’t write your relationship story, you do. A positive test may shake your confidence, strain your trust, or complicate your love life. But it doesn’t define your worth, and it definitely doesn’t mean the worst. What it does mean is that your body is giving you data. Now it’s time to listen, act, and heal.
Whether you're looking to test again, clarify confusing results, or just take the next step in taking control of your health, at-home testing can give you the privacy and clarity you need. Don't let fear stop you from being calm.
Don't wait and wonder; get the answers you need. This at-home gonorrhea test kit is discreet, fast, and trusted by thousands.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
1. Mayo Clinic – Gonorrhea Overview
2. Planned Parenthood – Gonorrhea Facts
3. Clinical Treatment of Gonorrhea | CDC
4. Gonorrhea - Symptoms and Causes | Mayo Clinic
5. Gonorrhea - Diagnosis and Treatment | Mayo Clinic
6. Gonorrhoea (Neisseria gonorrhoeae infection) | WHO
7. Screening for Chlamydial and Gonococcal Infections | NCBI
8. Sexually Transmitted Diseases (STDs) | NIH NICHD
About the Author
Dr. F. David, MD is a board-certified specialist in infectious diseases who works to stop, find, and treat STIs. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: J. Morales, NP | Last medically reviewed: December 2025
This article is for informational purposes and does not replace medical advice.










