Quick Answer: The ASHA report on new mpox cases in California shows why symptom awareness still matters, especially with overlapping signs like genital sores or rashes that can be mistaken for STDs. While mpox-specific tests aren't available at home, ruling out other infections with a discreet STI test can offer fast clarity and help guide next steps.
Who This Guide Is For (And Why It Matters)
If you’ve noticed a new rash or sore, especially after a hookup or recent exposure, and you’re not sure whether it’s an STD or something else, this article is for you. Maybe you live in a city where mpox has made a comeback, or maybe you’re just feeling anxious about a symptom that doesn’t quite make sense. This is for people who care about their health but don’t want to walk into a clinic with no answers and all the fear. It’s for folks dealing with shame, confusion, or simply lack of access.
Take Devin, 32, who noticed a single blister after a weekend festival in San Francisco. “I thought it was herpes,” he said, “but it didn’t itch or hurt.” Three days later, the sore crusted over, and he realized mpox was back in the news. Stories like this remind us that the line between STDs and other infections isn’t always clear. That’s why testing, even just to rule things out, can offer real peace of mind.
In this article, we’ll unpack what counts as an STD test, how timing affects results, when retesting makes sense, and what to do if symptoms persist. Mpox might not be testable at home, but your body is still telling you something, and we’ll help you listen.

People are also reading: My Partner Has Gonorrhea, But I’ve Been Faithful
What Actually Counts as an STD Test?
Not all “STD tests” are created equal, and most of what we fear (or misinterpret) comes down to not knowing what the test can or can’t detect. When you order an at-home kit, you’re usually getting a combination of highly sensitive NAAT or PCR tests for bacterial infections like chlamydia and gonorrhea, plus antibody or antigen tests for things like syphilis and HIV. These are real clinical-grade diagnostics, not just “screening tools.”
For example, CDC guidelines confirm that NAAT is the gold standard for detecting gonorrhea and chlamydia. These tests look for the genetic material of the bacteria itself, not just signs your body is reacting. It means you can detect an infection even before symptoms fully develop.
What makes all of this especially important now is how closely some symptoms mimic one another. Mpox, for instance, often starts with a single painless lesion, exactly what many people expect from genital herpes or a syphilis chancre. If you’re not testing, you’re guessing. And guessing means waiting longer for treatment, or spreading something unknowingly.
At-home tests usually involve collecting a urine sample, genital swab, throat swab, or a small fingerprick of blood. Everything is discreet, often delivered in unmarked packaging. STD Rapid Test Kits provides several options, including the Combo STD Home Test Kit that checks for multiple infections at once.
Window Periods: What to Know for Each STD
Before you panic, or breathe a sigh of relief, timing matters. Every STD has a “window period,” which is the time between exposure and when a test can reliably detect the infection. If you test too early, you might get a false negative even if you’ve been infected. This is different from the “incubation period,” which is how long it takes for symptoms to show up. And here’s the kicker: for some infections, you can be contagious before you ever see a sign.
That’s why a new sore, rash, or irritation, especially if it appears just a few days after sex, might not be caught by a test yet. The body needs time to produce enough detectable material: bacterial DNA, viral RNA, or antibodies, depending on the test type. Mpox, like syphilis, can take days or even weeks to develop visible lesions, and doesn’t always trigger symptoms right away. That means what you're seeing might not be the thing you're testing for, but it's still a sign something's off.
| STD | Common Test Type | Sample | Typical Window Period | When Accuracy Peaks |
|---|---|---|---|---|
| Chlamydia | NAAT/PCR | Urine or swab | 7–14 days | 14+ days |
| Gonorrhea | NAAT/PCR | Urine or swab | 7–14 days | 14+ days |
| Syphilis | Antibody (treponemal/non-treponemal) | Blood | 3–6 weeks | 6–12 weeks |
| HIV | Ag/Ab combo or NAAT | Blood or oral fluid | 2–6 weeks (Ag/Ab), 10–33 days (NAAT) | 6–12 weeks |
| Trichomoniasis | NAAT/Rapid antigen | Swab or urine | 5–28 days | 2–4 weeks |
Figure 1. Master window period table for common STDs. Mpox is not routinely included in this chart because it's not part of standard STI panels, but its symptoms often overlap.
Rapid Test vs Lab Test: Pros, Cons, and Tradeoffs
Let’s be honest, most people who test at home do it for one of two reasons: privacy or panic. Maybe you don’t want your hookup history sitting in a clinic file. Maybe the rash appeared while you’re visiting family or on a work trip. Maybe you just don’t want to sit in a waiting room, trying not to squirm. All of those reasons are valid, and rapid tests offer a lifeline in those moments. But like all tools, they have limits.
Rapid at-home kits give results in minutes. That immediacy can be a huge relief, especially when symptoms appear suddenly. But they may sacrifice a bit of accuracy, particularly early in the window period or if instructions aren’t followed precisely. Lab-processed tests (whether done at home or in a clinic) tend to be more sensitive, especially for infections like HIV or syphilis. If you’re unsure, it’s okay to start with one and confirm with the other.
| Method | Privacy | Speed | Sensitivity/Accuracy | Good Fit When |
|---|---|---|---|---|
| At-Home Rapid | Very high | Minutes | Moderate–High | You need an immediate read and value privacy |
| Mail-In Lab | High | 1–3 business days after mailing | High | You want lab-grade accuracy without visiting a clinic |
| Clinic Visit | Low–Moderate | Same-day to several days | Very high | You have persistent symptoms or need in-person care |
Figure 2. Testing method comparison across speed, privacy, and accuracy. Mpox-specific tests are only available through health departments or clinics but STD symptoms that mimic mpox can be ruled out from home.
When to Test After Exposure
Imagine this: it’s been five days since you hooked up with someone new. Now you’ve got a weird sore, or maybe just irritation, and your brain won’t shut up. You’re thinking about everything from herpes to mpox to something random like an ingrown hair. You want answers. But testing right now could give you a false sense of security.
Here’s the truth: if it’s been fewer than 7 days, most tests might not catch the infection yet. That’s especially true for bacterial STDs like chlamydia and gonorrhea. But if symptoms are intense or worsening fast, you should absolutely seek care, especially since early mpox symptoms can include fever, fatigue, and a single lesion. If it’s been 7 to 13 days, you’re in a gray zone: many infections will be detectable, but if your results are negative and symptoms persist, plan to retest later. At 14 days or more, most infections will show up clearly on rapid or lab tests.
Case in point: Luis, 29, tested five days after noticing a blister. His test was negative for herpes, syphilis, and gonorrhea. But ten days later, he had swollen lymph nodes and a scabbed-over sore. A clinic swabbed the lesion, confirmed mpox.
“I was glad I tested early,” he said. “But that second test? That’s what gave me the answer.
Check Your STD Status in Minutes
Test at Home with RemediumGenital Herpes Test Kit
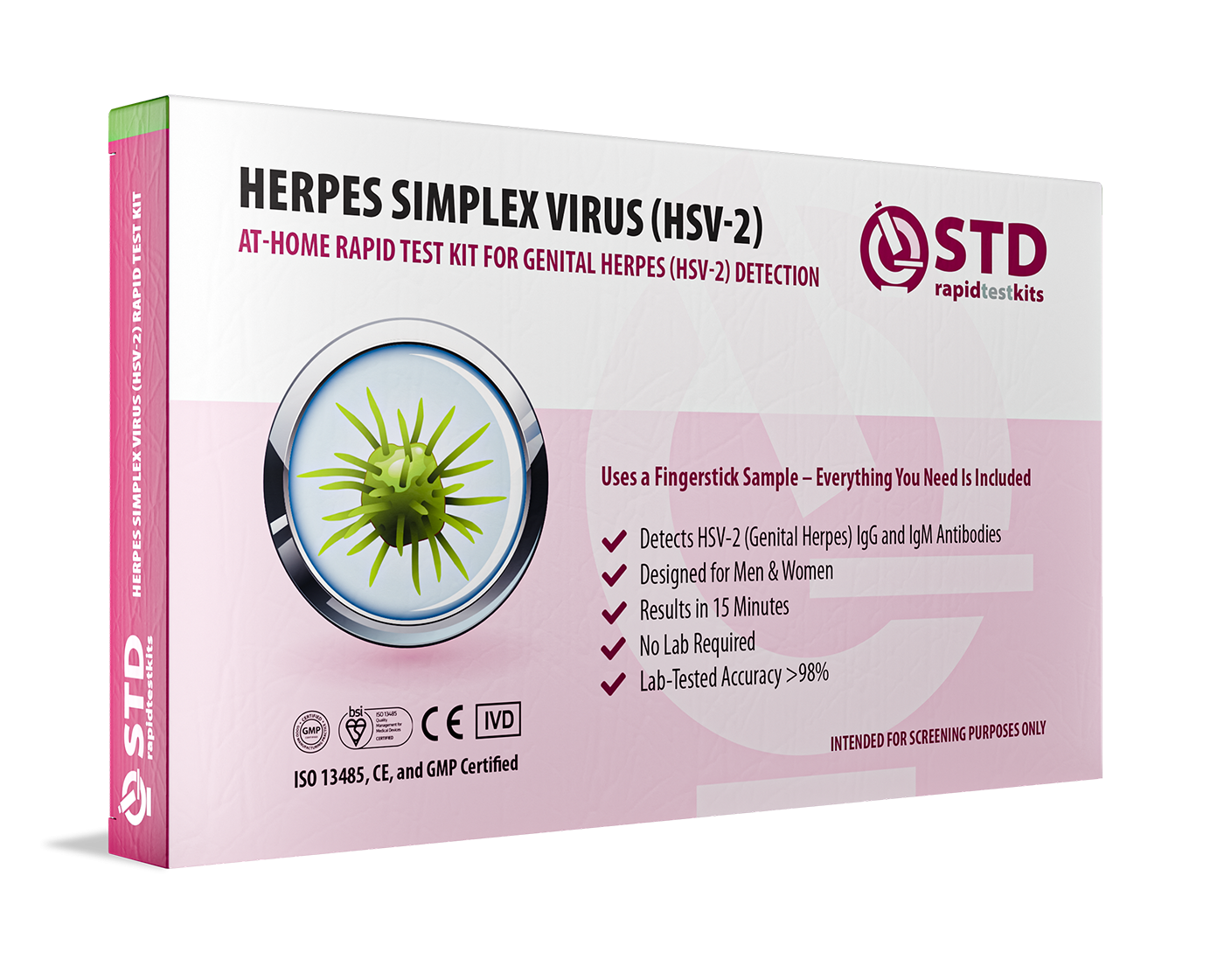
 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $45.99 $49.00
Do You Need to Retest? Here’s How to Know
Retesting is one of the most underused tools in sexual health. Whether you're dealing with confusing symptoms or just want to be sure, there are solid reasons to test more than once. If you tested too early after exposure, you’ll want to retest in the window period’s later range. For herpes and syphilis, that might mean 6 to 12 weeks. If you’ve already been treated for an infection, retesting confirms clearance and can catch reinfection, especially if your partner wasn’t treated at the same time.
Picture Aimee, 34, who tested positive for chlamydia, got treated, but never told her partner. She tested again a month later, positive again. “That retest saved me from getting PID,” she said. “I wouldn’t have known otherwise.”
Retesting doesn’t mean you did something wrong. It means you’re paying attention. Return to STD Rapid Test Kits to explore retest options and take control of your next step.
Privacy, Shipping, and Discreet Support
Waiting is the hardest part, and when it comes to sexual health, waiting in a clinic or pharmacy can be a dealbreaker. That’s why privacy matters just as much as accuracy. All test kits from STD Rapid Test Kits are shipped in plain, unmarked packaging. No one, not neighbors, roommates, or mail carriers, will know what’s inside. The name on your bank statement? It’s discreet, too.
Shipping typically takes 1 to 3 business days. If you're traveling, living remotely, or simply trying to manage anxiety, you can plan around delivery and testing windows. Results are yours alone, and you choose who to share them with. Unlike clinic-based results that may go into shared electronic records, at-home tests put the control back in your hands.
Need help along the way? Support teams are available with live assistance, not chatbots, so you’re never left interpreting results alone. Whether it’s a faint line or a blank cassette, you’ll have backup.

People are also reading: What No One Tells You About Gonorrhea and Shared Toys
What If You Test Positive?
Take a deep breath, most STDs are treatable. A positive result might feel like a wrecking ball at first, but it’s actually a beginning, not an ending. The next steps are clearer than you think. First, confirm your result if you used a rapid test. Especially for things like syphilis or HIV, a follow-up with a clinic or telehealth provider can lock in the diagnosis and start treatment.
Then comes partner notification. It’s awkward, but it doesn’t have to be agonizing. Many public health departments or services offer anonymous messaging, and clinics can often help you draft what to say. If you’re nervous, scripts are available, and the goal is care, not blame.
Jamari, 41, got a positive syphilis result after noticing a painless sore. “I cried in my car,” he said. “Then I texted my last two partners. One of them had symptoms and didn’t even know it. We both got treated.” That’s the real power of testing, it interrupts transmission, saves future health, and starts honest conversations.
FAQs
1. Is mpox still a thing?
Yep, especially in cities like L.A. and San Francisco, where clusters are showing up again. Just because it’s not on the news doesn’t mean it vanished. It’s still circulating, especially in communities of men who have sex with men, and it's often mistaken for STDs like herpes or syphilis.
2. Can mpox really look like an STD?
Totally. One of the biggest issues with mpox is that it can show up as a single sore or blister, often in the genital or anal area. That’s why so many people assume it’s herpes, until other symptoms kick in, like swollen lymph nodes or fatigue. If you’re unsure, start by ruling out the usual suspects with a home test.
3. Is there an at-home mpox test?
Not right now. Mpox needs a special swab test done on an actual sore and sent to a lab, usually through a clinic or health department. But if you’re staring at a bump and freaking out, you can still use an at-home STD kit to check for things like chlamydia, gonorrhea, and syphilis while you monitor for other signs.
4. I got a rash after sex. Could it be mpox?
It could be, but it could also be irritation, shaving bumps, or an STD. The key is what the rash looks like and how fast it changes. Mpox often starts as firm, raised lesions that eventually scab over. If you also feel run down or develop a fever, that’s your cue to get checked in person.
5. Can I have an STD and mpox at the same time?
Unfortunately, yes. Co-infections happen more often than you’d think. The sore you see might be mpox, but you could also have gonorrhea or chlamydia simmering quietly. That’s why a combo test is smart, it gives you a fuller picture of what’s going on.
6. How long should I wait before testing after a risky hookup?
Aim for 14 days. That’s the sweet spot for catching most infections. Testing earlier is possible, but you may need to retest if results are negative and you still feel off. There’s no shame in doing it twice, it’s about clarity, not punishment.
7. What if I test negative but still have symptoms?
Listen to your body. A negative result is helpful, but it’s not the end of the story, especially if you tested early. Some infections take time to show up. If your symptoms stick around or get worse, follow up. This is where retesting or clinic visits come in handy.
8. Do home STD tests work if I have a sore?
Depends. If the sore is leaking, bleeding, or super inflamed, it’s best to let a provider swab it directly. But if you’re testing for internal infections or bloodborne STDs, at-home tests still work. Just don’t try to swab an open wound at home, leave that to the pros.
9. Can I get treated based on an at-home test result?
In many cases, yes. Some telehealth providers will prescribe treatment based on documented at-home test results, especially for common infections like chlamydia or gonorrhea. If your test is positive, reach out to a provider right away. Most STDs are fast and easy to treat when caught early.
10. What should I say to a partner if I test positive?
Start with honesty, not fear. You don’t need to confess, you need to communicate. Try: “I just got my test results, and I think you should test too.” You’re not just protecting them, you’re showing you care enough to speak up. And that’s powerful.
You Deserve Answers, Not Assumptions
We know what it’s like to spiral over a rash, a sore, or something that just feels off. With mpox making quiet rounds again in places like California, now’s not the time to guess. While you can’t test for mpox at home, you can rule out the most common STDs quickly and privately, so you’re not stuck in the dark.
Don’t wait and wonder, get the clarity you deserve. This at-home combo test kit checks for the most common STDs discreetly and quickly.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
1. New Mpox Cases in California Raise Concern – ASHA
2. CDC – 2021 STI Treatment Guidelines
3. HIV.gov – HIV Testing Overview
4. Monkeypox (Mpox) – CDC Overview (symptoms, rash, transmission)
5. Mpox (Monkeypox) Fact Sheet | WHO (rash and disease basics)
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: M. Alvarez, MPH | Last medically reviewed: January 2026
This article is for informational purposes and does not replace medical advice.










