Quick Answer: Chlamydia may not show up on a test until 7 to 14 days after exposure. If you tested earlier, symptoms may still be caused by an active infection. Retesting at the right time is key.
Who This Article Is For, and Why It Matters
This guide is for anyone who's staring at a negative chlamydia test result but still feels like something's off. It's for the person who hooked up on a trip, tested two days later, and can’t stop wondering. For the person who got treated last year but is still having pain. For the person who did everything “right”, and still doesn’t feel right.
It’s also for those of us who worry we’re being dramatic. Who Google symptoms at 2AM and then talk ourselves out of getting help. If that’s you, you deserve clarity, without judgment or shame. This article breaks down what could be going on, when to retest, and what to do if your test missed something important.
Testing is self-care. So is retesting.

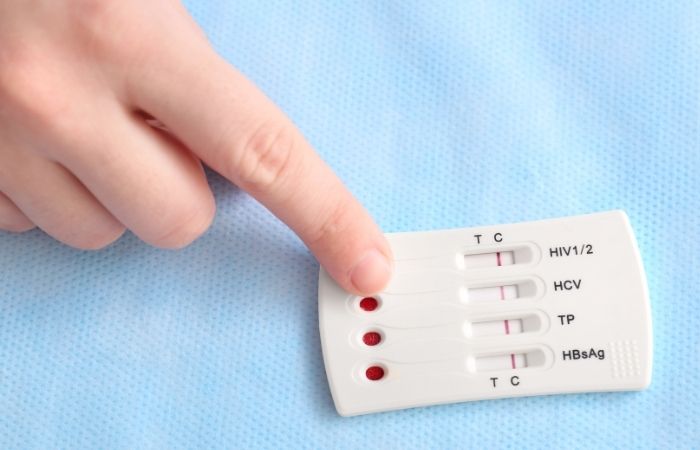
People are also reading: Why That Faint Line on Your STD Test Might Not Be Nothing
Can You Really Have Chlamydia With a Negative Test?
Yes, especially if you tested too early, used the wrong type of test, or didn't collect the sample properly. Even highly accurate tests like NAAT (nucleic acid amplification tests) aren't magic. They rely on enough bacteria being present at the time of collection to trigger a positive result.
False negatives for chlamydia happen most commonly when:
| Cause | Explanation |
|---|---|
| Tested too early | Most tests can’t detect chlamydia until at least 7 days after exposure. Testing before that may result in a false negative. |
| Low bacterial load | If the infection hasn’t multiplied enough, it might not register on a test, even if it’s already in your body. |
| Poor sample collection | Swabbing too gently, missing the urethra or cervix area, or not collecting first-catch urine can lead to incorrect results. |
| Window period confusion | Many people think “no symptoms = no infection” or “negative = done.” But window periods complicate both assumptions. |
Figure 1. Common reasons for false negative results on a chlamydia test.
According to the CDC, the preferred test for chlamydia detection is NAAT, which has high sensitivity and specificity, when timed correctly. But even NAATs can miss early infections, particularly in asymptomatic individuals or those with atypical presentation.
Understanding Window Periods: When Chlamydia Can Be Missed
So let’s talk timing. The window period is the time between when you’re exposed to an STD and when it can reliably be detected on a test. For chlamydia, that’s generally 7 to 14 days. If you test too soon, say, 2 or 3 days after a risky encounter, you could get a false sense of security.
| Time Since Exposure | Test Sensitivity | Recommendation |
|---|---|---|
| 0–3 days | Very low | Wait to test. Bacteria may not be detectable yet. |
| 4–6 days | Low–Moderate | Testing may show results but can miss early infections. Consider retesting at 14 days. |
| 7–13 days | Moderate–High | Tests more likely to detect chlamydia. Retest if symptoms persist. |
| 14+ days | High | Best time for peak accuracy. |
Figure 2. Chlamydia detection window and retesting recommendations by time since exposure.
Real talk: many people test early because they’re anxious. That’s valid. But that early test? It might just be the beginning, not the end, of your diagnosis journey.
“I Tested Negative. Then It Got Worse.”
Jordan, 26, tested negative for chlamydia four days after a condom broke with a new partner. “I thought I was good to go,” he says. “But then I started getting discharge and pain when peeing. I almost didn’t go back in, figured it was anxiety.” He retested at 16 days post-exposure and came back positive.
“I was pissed at myself for trusting the first test. But nobody told me I had to wait. Nobody told me about the window thing.”
Jordan’s story is more common than most realize. And it’s why follow-up testing is often recommended if symptoms persist or if you tested before the 14-day mark.
Could It Be Something Else? When Symptoms Mimic Chlamydia
So your chlamydia test came back negative, but you’re still uncomfortable, and that matters. The truth is, other conditions can mimic chlamydia almost symptom for symptom. From burning and discharge to pelvic pain and spotting, your body’s warning signs might be pointing in the right direction… just not to the right name.
Here are some possibilities that could explain your symptoms even if your test was technically accurate:
| Condition | Overlapping Symptoms | Key Differences |
|---|---|---|
| Trichomoniasis | Itching, discharge, irritation, spotting | Often missed on standard STD panels unless specifically tested; frothy discharge is more common |
| Bacterial Vaginosis (BV) | Odor, discharge, mild burning | Not an STD, but often triggered by sexual activity; pH-related imbalance |
| Yeast Infection | Itching, thick discharge, swelling | No odor; clumpy white discharge; doesn’t typically cause spotting or pain with urination |
| UTI (Urinary Tract Infection) | Burning urination, pressure, urgency | Urinary frequency is more prominent; typically no discharge |
| Herpes (HSV-1 or HSV-2) | Burning, stinging, discomfort in genitals | Often appears as sores or raw skin, but some cases have no visible lesions |
Figure 3. Common infections that present like chlamydia, and how to tell the difference.
Even peer-reviewed studies confirm that symptom overlap makes self-diagnosis risky. This is why combo testing and full STI panels are often recommended when symptoms persist.
Check Your STD Status in Minutes
Test at Home with RemediumChlamydia Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $33.99 $49.00
At-Home vs. Lab vs. Clinic: Does It Change the Outcome?
The test type you used plays a big role in how reliable your results are, and whether you might need to retest. Here's what to know:
| Test Type | Speed | Accuracy | Limitations |
|---|---|---|---|
| At-Home Rapid Test | Minutes | Moderate–High | May miss early or low-load infections; user error can affect results |
| Mail-In Lab Kit | 1–3 days | High | Collection quality and timing still matter; no same-day results |
| Clinic-Based NAAT | Same day to several days | Very High | Access barriers, cost, stigma may delay testing |
Figure 4. Comparing common STD testing methods and what can affect results.
If you used a rapid test for chlamydia and you’re still having symptoms, retesting with a lab-grade NAAT can provide clarity. Many people use a rapid test for peace of mind immediately after exposure, then follow up with a lab test at 14+ days.
When to Retest After a Negative Result
If you don't feel like you have chlamydia but your test came back negative, it's smart to get tested again. This is when it makes sense:
- If you tested less than 7 days after exposure, wait 14 days and test again. It could have been missed in the early tests.
- If symptoms last longer than 7 to 10 days, get retested or see a doctor for a more thorough checkup.
- If you used a rapid or home kit, think about getting a lab-based NAAT to confirm, especially if your symptoms get worse.
- If your partner tests positive, you should test again no matter what your first result was.
And if you’re still unsure? Ask yourself: What would help me stop obsessing about this? Often, the answer is retesting, not because you didn’t believe the first test, but because peace of mind is powerful.
What If It’s Not an STD at All?
Sometimes, the test is right, and your symptoms are real, but the cause isn’t chlamydia or even an STD. The body can react to a wide range of non-infectious issues with the same warning signs: inflammation, discharge, burning, spotting. That doesn’t make your experience any less valid, it just means the path forward might look a little different.
Here are some reasons your symptoms might persist, even when STDs are ruled out:
| Non-STD Cause | How It Mimics STD Symptoms | Why It’s Often Missed |
|---|---|---|
| Inflammation from friction or allergens | Burning, irritation, minor spotting | Common after vigorous sex or new lubricants; not usually tested for |
| Pelvic floor dysfunction | Deep pelvic pain, pressure, pain during sex | Often mistaken for infection; requires specialized diagnosis |
| Hormonal changes | Spotting, dryness, altered discharge | Can mimic infection, especially during perimenopause or hormonal birth control use |
| Interstitial cystitis | Urgency, burning, bladder pain | Mimics UTI or chlamydia but is not caused by infection |
| Post-antibiotic imbalance | Irritation, discharge, yeast overgrowth | Often follows recent STD or UTI treatment; can prolong symptoms |
Figure 5. Common non-infectious causes of STD-like symptoms and why they go undiagnosed.
This is where trauma-informed care really matters. You shouldn’t have to fight to be believed just because your swab or urine came back “clean.” Your discomfort is real, and there’s always a next step.
Do I Need a Test of Cure?
A “test of cure” is when you’re retested after treatment to confirm the infection is fully gone. For chlamydia, most people don’t need a test of cure, unless you’re pregnant, had severe symptoms, or your provider suspects reinfection.
However, what most people do need is a retest three months after treatment, per CDC guidelines. This isn’t just about you. It’s also about catching reinfection if your partner wasn’t treated, or if you’re still sexually active with someone who might be carrying it silently.
So if you’re reading this after treatment, and wondering why the symptoms are still lingering or coming back… the retest still matters.
CDC guidance on chlamydia testing and reinfection recommends routine follow-up within 3 months, especially for younger adults and anyone with a new partner.
People are also reading: Anal Itch, Burn, or Bleed? How to Tell If It’s an STD or Something Else
Emotional Whiplash: From Relief to Confusion to Fear
Testing negative should feel like a win, but when your body still feels off, that relief can turn into a minefield of questions. Maybe your doctor told you everything looks normal. Maybe the nurse at the clinic said you’re probably just stressed. Maybe your partner suggested it’s “in your head.”
Let’s be clear: your symptoms aren’t imaginary, and your intuition about your body is valid. This is the point where many people spiral or shut down. We want to stop that pattern in its tracks.
This is a better way:
- Check your symptoms. They are important.
- If the time or type of test could have affected accuracy, retest.
- If the symptoms don't make sense, think about getting a wider test or a combo kit.
- If all of the tests come back negative, talk to your doctor about other possible causes that aren't STDs, such as BV, yeast, interstitial cystitis, or hormonal imbalances.
And most importantly? Don't let the results of one test tell you how valuable you are, how sane you are, or how you feel about your body. You can ask more questions.
Whether It’s Round Two or a First Try, You Deserve Answers
If your first test didn’t settle the question, that’s okay. Sometimes we need to check again, not because we don’t trust the science, but because we trust ourselves.
Explore discreet options like the Combo STD Home Test Kit that checks for multiple STDs at once. No clinics. No awkward questions. Just you and the truth.
FAQs
1. Can I still have chlamydia if my test was negative?
Yes, and you’re not the only one asking this at 3AM. If you tested too early (like within the first 5–6 days after sex), there might not have been enough bacteria in your system yet for the test to pick it up. It’s like showing up to a crime scene before the clues are even visible. If something still feels off, trust your gut and retest after 14 days.
2. Why do I still have burning or discharge if I tested negative?
Because your body didn’t read the “all clear” text the test sent. Jokes aside, this is way more common than people realize. Burning, discharge, pain, it can all come from other things, like a UTI, trichomoniasis, or even irritation from a new lube. A negative test doesn't mean your symptoms are fake. It just means the test didn’t find that specific bug… yet.
3. How soon can I retest for chlamydia after a negative?
Most experts say to wait until 14 days after exposure. That’s when tests are most reliable. If you tested earlier because you were freaking out (totally fair), just plan for a follow-up test once you hit the two-week mark. Think of it like double-checking your receipt before leaving the store, you just want to make sure nothing important got missed.
4. Is it normal to test negative but still feel “off” down there?
Completely. You’re not imagining things. Lots of people feel soreness, spotting, or just a weird vibe in their bodies even after a negative result. Sometimes it’s an early infection. Sometimes it’s friction, hormones, or something non-STD like BV or yeast. Your body talks. Keep listening. And don’t let one test shut the conversation down.
5. Do at-home chlamydia tests work, or should I go to a clinic?
Both can work, if you use them right and at the right time. At-home rapid tests are great for privacy and speed, but they can miss very early infections. Clinics tend to use lab-grade NAATs, which are more sensitive. If you started with a rapid and still have symptoms, no shame in backing it up with a lab test.
6. Could this be something else like BV or trich?
Yes, and honestly? It might be. BV, yeast, trichomoniasis, they all mimic chlamydia in annoying ways. You might get discharge, itching, irritation, or even spotting and pain during sex. This is why combo tests exist and why providers sometimes treat based on symptoms before the results even come in.
7. Do I need to get retested if my partner tested positive?
Absolutely. Even if your own test said negative, your partner’s positive result changes the story. Maybe you tested too early. Maybe you picked up a low-level infection that hadn’t built up yet. Either way, retest, because that exposure is now confirmed, not hypothetical. In some cases, you might even be treated preemptively.
8. My symptoms came back after treatment, what gives?
It could be reinfection (yep, it happens fast if your partner wasn’t treated too), or leftover inflammation that takes time to settle down. Some people also get a yeast infection after antibiotics, which feels like a cruel joke. The key? Don’t assume you’re fine just because the meds are done. If things still hurt, test again.
9. Could this be all in my head?
Short answer: no. Longer answer: your nervous system and immune system are buddies. If you're anxious, hyper-aware, or scared (understandably), it might make the sensations feel louder, but that doesn’t mean they aren’t real. A real symptom is still real, even if it’s amplified by stress. Your concern is valid.
10. What if I can’t afford another test right now?
You're not alone. Health care should go easy on the wallet, but here we are. Look for local clinics, LGBTQ+ clinics, or organizations that provide free or reduced-rate testing. Home testing kits come with varying price tags, and combos are often cheaper than purchasing tests separately. The bottom line: you deserve the truth, regardless of the price.
You Deserve Answers, Not Assumptions
A negative result can feel like the end, but it's not always the last word. It's important to pay attention to what your body is telling you. You can keep asking questions, retesting, and asking for clarity without saying sorry if something still doesn't feel right.
At-home tests can be a powerful tool in your hands. They let you check discreetly, on your own terms, and as often as needed. This at-home combo test kit offers peace of mind that’s private, fast, and trusted.
You’re not overreacting. You’re advocating for yourself.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
1. Mayo Clinic – STD Testing: What You Need to Know
2. Planned Parenthood – What Is Chlamydia?
4. False positive results on HIV tests
5. CDC STI Screening Recommendations
About the Author
Dr. F. David, MD is a board-certified infectious disease doctor who specializes in preventing, diagnosing, and treating STIs. He is dedicated to making his work available to more people, whether they live in cities or off the grid. He combines clinical accuracy with a straightforward, sex-positive approach.
Reviewed by: Janelle Parker, NP, AAHIVS | Last medically reviewed: December 2025










