Quick Answer: If you’re dealing with a persistent genital itch, it might be a simple irritation, like dryness, shaving burn or a detergent reaction, but it could also signal a more serious issue such as a sexually transmitted infection (STI) like Genital Herpes, Trichomoniasis or Chlamydia. The key is, when the itch lasts beyond a few days, is accompanied by other symptoms (rash, sores, discharge, pain), or keeps returning, book a test or see a health professional.
Meet the Itch: A Story You Might Recognize
Marisol, 31, was trying to focus at her job when that same familiar itch flared up again, right along the fold of her groin. She hadn’t had sex in a few weeks, but this wasn’t the first time it had crept up. She blamed it on sweating, then on her razor, then her laundry soap. But now it was starting to sting a little. The over-the-counter cream she picked up last time hadn’t helped for long. And a memory flashed back: an ex from six months ago had mentioned a cold sore once. Her stomach dropped. Was this really just dry skin?
This isn’t uncommon. That uncertainty, the not knowing, can trigger more anxiety than the itch itself. And if you’ve ever scratched yourself into a full-blown panic spiral, this article is for you.
Why Genital Itching Happens (And What It’s Not)
Genital itching doesn’t always mean you’ve picked up an STD. In fact, most cases aren’t caused by infections at all. The skin in your pubic area is thinner, more delicate, and more exposed to irritants than almost anywhere else on your body. Sweat, shaving, synthetic underwear, new soaps, friction during sex, hormonal changes, any of these can disrupt the skin barrier and set off a maddening itch.
But there’s a tricky overlap: many STIs also begin with subtle symptoms like itching, dryness, or irritation. That’s why it’s so easy to misread the signals, or to delay testing out of shame or confusion.
| Cause | Typical Features | When to Worry |
|---|---|---|
| Dry skin or irritation | Itch with no visible bumps or discharge; often after shaving, sweating, or new product use | If it lasts more than 3–5 days or spreads |
| Fungal infection (e.g., jock itch) | Red, ring-like rash that may burn or peel; often in folds | If OTC creams don’t help in a week |
| Allergic reaction (contact dermatitis) | Itching + redness or swelling after exposure to detergent, condoms, etc. | If it worsens or causes pain with urination/sex |
| STI (e.g., Herpes, Trich, Chlamydia) | Persistent or recurring itch, sometimes with sores, discharge, or internal discomfort | Always test if new partner, unprotected sex, or symptoms persist |

People are also reading: Why Your Travel Itinerary Should Include an STD Test
Could It Be Genital Herpes?
Herpes isn’t always a blister. In many cases, the first symptom is an unexplained itch or tingle. That “prodrome” phase, where the virus is active but not yet visible, can feel like dryness, skin tightness, or subtle burning. According to the CDC, many people with genital herpes don’t even know they have it.
The itch often starts in a small area, may come and go, and sometimes evolves into sores a few days later. Or not at all. Some people only ever experience the prodrome. That’s why so many people misdiagnose themselves, or don’t test until months later when a partner gets symptoms.
What About Trichomoniasis?
Trichomoniasis (often just called "trich") is one of the most under-diagnosed STIs in the U.S., and one of the itchiest. Caused by a tiny parasite, it often leads to intense genital itching, burning during urination, and unusually strong-smelling discharge in people with vaginas. For penis-owners, symptoms can be much more subtle, maybe just an inner itch, urethral irritation, or discomfort after ejaculation.
Because trich can live inside you for weeks or months before symptoms show (or never show at all), it often gets mistaken for a yeast infection or UTI. And if you’ve ever been treated for a yeast infection that didn’t go away? This might be why.
Testing for trich is available via rapid antigen swabs or NAAT (nucleic acid amplification) tests. You can order both through this at-home combo test kit without stepping into a clinic.
Check Your STD Status in Minutes
Test at Home with RemediumTrichomoniasis Test Kit
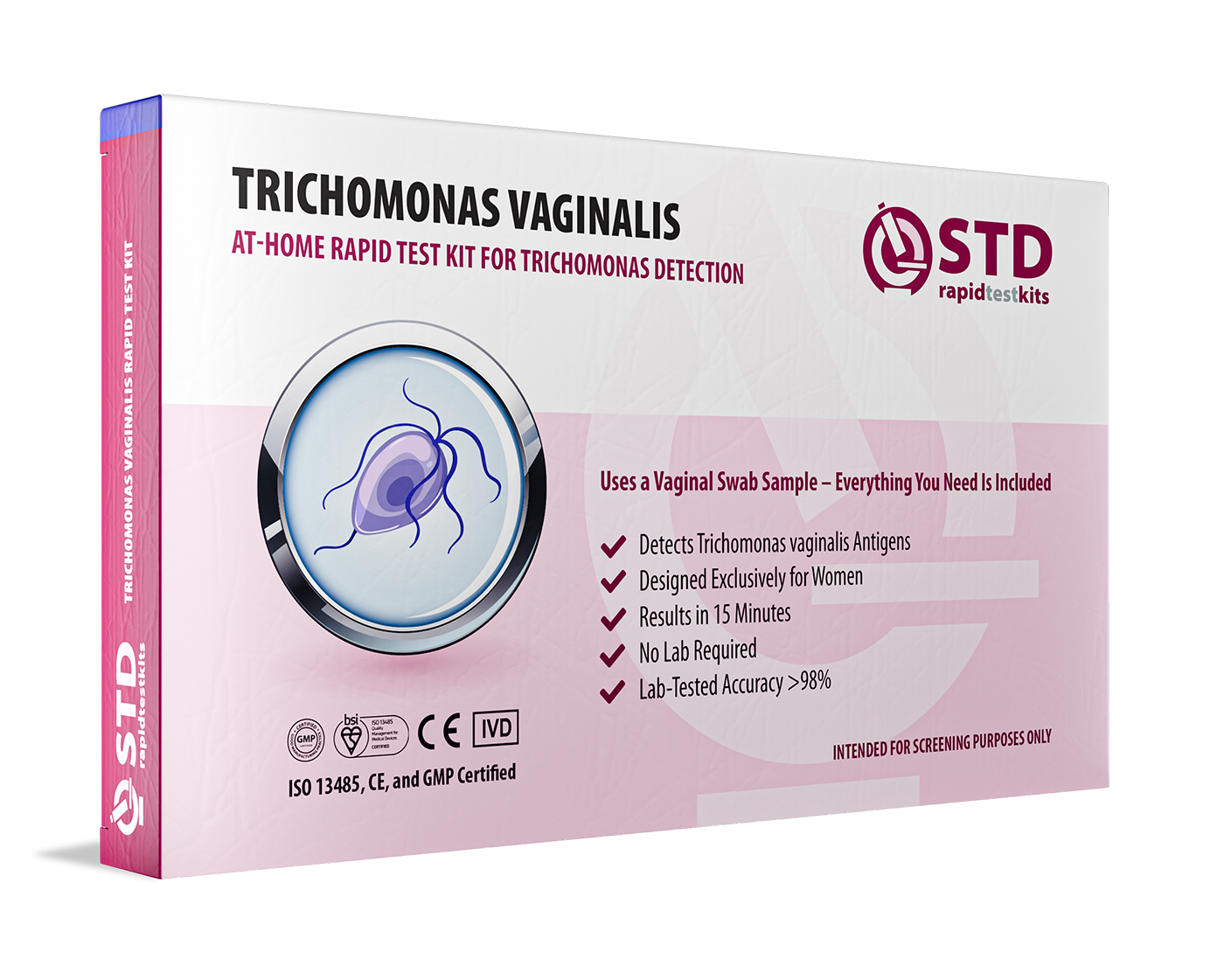
 For Women
For Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $33.99 $49.00
Could It Be Chlamydia (Even With No Discharge)?
While many people associate Chlamydia with discharge or painful urination, genital itching can also occur, especially if the infection has spread into the urethra or cervix. The tricky part? Chlamydia can stay asymptomatic for weeks, months, or forever. That means itching may be your only warning sign.
In some cases, mild internal itching, like a weird awareness of your urethra, shows up before more obvious symptoms. And if you’ve had unprotected sex in the past 2–6 weeks, you should test even if you think it’s “just friction.” Chlamydia is often silent but highly contagious.
Fortunately, Chlamydia is curable with antibiotics. The key is testing at the right time, usually at least 14 days after exposure for best accuracy.
Yeast, Bacterial Vaginosis, or STIs?
Here’s the plot twist: not all genital infections are sexually transmitted, but they can still look and feel the same. Yeast infections are known for their signature itch, but bacterial vaginosis (BV) can cause irritation too, without the thick white discharge people expect. For some, it’s more of a sour smell, a swollen feeling, or discomfort with sex that gets worse over time.
People often treat BV or yeast with over-the-counter meds, but those don’t touch STIs. And sometimes, people treat STIs when it’s really eczema or dermatitis. That’s why accurate diagnosis matters. The symptoms overlap. The treatments don’t.
Two Case Studies: When the Itch Wasn’t What It Seemed
Case 1: Ty, 28, noticed persistent itching at the base of his penis. He figured it was due to cycling and sweat, maybe even the lube from a hookup a few nights ago. No bumps, no discharge. Just that annoying itch. After a week, it got worse. He ordered a test out of paranoia, and turned out he had Herpes. The sores showed up days later. His takeaway? “I wish I hadn’t waited. I could’ve started meds sooner and maybe prevented a full outbreak.”
Case 2: Lena, 34, had itching on her outer vulva for months. She’d tried yeast creams, switched soaps, even bought new underwear. Nothing worked. She thought it might be herpes, until a nurse practitioner looked at her and immediately suspected lichen sclerosus, a chronic skin condition. A biopsy confirmed it. Treatment changed her life. “All those years I blamed myself or thought I had an STD… turns out it was my skin attacking itself.”
How Long Should You Wait Before Testing?
If you’ve recently had sex and started itching afterward, the first instinct might be to panic, or to Google endlessly for answers. But the timing of testing really matters. Each STI has a “window period”, the time between exposure and when it shows up on a test.
Here’s a reference to help you decide when to test, and when to retest if needed:
| Infection | Earliest Reliable Test | Best Time to Test | Retesting Needed? |
|---|---|---|---|
| Chlamydia | 7 days | 14 days | Yes, if tested early |
| Gonorrhea | 6–7 days | 14 days | Yes, if tested early |
| Trichomoniasis | 7 days | 14+ days | Sometimes |
| Herpes (HSV-2) | 10 days (PCR) | 4–6 weeks (antibody) | Yes, unless tested via active sore |
If you’re still unsure, you can always test now and plan to retest again in a few weeks. Most people would rather know than keep guessing, and the emotional toll of uncertainty often outweighs the discomfort of testing.
When It’s Not an STI, But Still Serious
Some genital itches have nothing to do with sex. But that doesn’t mean they aren’t real, or that they don’t need treatment. Chronic skin conditions like lichen sclerosus, eczema, and psoriasis can show up as dry, cracked, or itchy patches on the genitals. These often go misdiagnosed for years, especially among people assigned female at birth.
Hormonal changes (such as menopause or postpartum dryness), latex or spermicide allergies, or even stress-induced dermatitis are other non-infectious causes. According to a 2023 study that was published in the Journal of Clinical and Aesthetic Dermatology, up to 28% of cases of chronic vulvar itching were not infectious and were often misdiagnosed as herpes or yeast.
The bottom line? If creams aren’t working, or symptoms persist longer than two weeks, see a provider, ideally a sexual health specialist or dermatologist with vulvar or penile expertise.

People are also reading: Hepatitis B vs C: How to Tell the Difference, Get Tested, and Stay Safe
What to Do While You Wait for Answers
Waiting for results can feel like torture. So here’s how to stay sane and avoid making it worse:
First, skip the harsh soaps. Use plain water or a fragrance-free cleanser. Stick to loose, cotton underwear. Avoid shaving, waxing, or applying creams not prescribed by a doctor, especially steroid creams, which can thin the skin over time if misused.
It’s also okay to pause sex until things calm down. Not because sex is dirty, but because you deserve comfort and clarity. And if the itch has you spiraling into shame or panic, know that you’re not alone. This isn’t about being “clean” or “dirty.” It’s about your body asking for attention. You’re doing the right thing by listening.
Talking to Your Partner Without Panic
If you’re in a relationship, or recently hooked up, it’s natural to worry about what to say. But one itchy symptom doesn’t mean you’re accusing anyone of anything. Try this:
“Hey, I’ve been dealing with some irritation and I’m not sure what’s causing it. I’m going to get tested to be safe, and I just wanted to let you know in case it’s something we both should look at.”
You don’t need all the answers before you start the conversation. Just honesty and compassion. If your partner freaks out, remember: their reaction is about them, not about your worth or responsibility. Your health comes first.
Privacy, Discretion, and Peace of Mind
If walking into a clinic feels too daunting, or isn’t possible due to location, work, or fear of being seen, you’re not out of options. STD Rapid Test Kits ships discreetly in unmarked packaging, with at-home results in minutes for most common infections. No waiting rooms. No judgment. Just clear answers.
Many users say testing from home actually made it easier to focus on what mattered: getting treated, getting answers, or breathing a huge sigh of relief. You can test solo, with a partner, or even keep a few kits on hand for post-hookup peace of mind. Testing doesn’t make you paranoid, it makes you proactive.
Your Itch Doesn’t Define You, But It Might Be Telling You Something
Let’s be real: genitals are sensitive, and so are the conversations around them. But your discomfort is valid, and your curiosity about your own body is brave. Whether it turns out to be a minor irritation or something that needs medication, testing is never a mistake. The itch is your body talking. Listening isn’t overreacting, it’s responsible.
If you’re ready to stop guessing and start knowing, this discreet at-home combo test checks for Chlamydia, Gonorrhea, Trichomoniasis, Syphilis, and more, without judgment, appointments, or delay.
Check Your STD Status in Minutes
Test at Home with Remedium7-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $129.00 $343.00
For all 7 tests
Before You Assume, Take the Next Step
Jon, 42, was sure it was nothing. A little itch near his inner thigh, maybe heat rash or tight boxers. He ignored it. Then it flared after sex. Then again a month later. He finally tested and learned it was Trichomoniasis, treatable, but silently spreading for months. “If I’d just tested when it first showed up,” he told us, “I would’ve saved myself a lot of awkward convos and stress.”
We’re not sharing this to scare you, but to remind you that the only “wrong” move is doing nothing when something feels off. You know your body. You know when something’s changed. And even if it turns out to be irritation or dryness, testing clears the air and gives you back your calm.
Your genitals don’t need to be a mystery. You deserve answers that come without judgment, without shame, and without waiting weeks for a clinic slot. That’s why at-home testing exists, not because we’re too lazy to see a doctor, but because access matters. Privacy matters. Mental health matters.
Whether it’s dryness, friction, herpes, or something else entirely, there’s one truth: You’re not dirty. You’re not gross. You’re just paying attention. And that’s brave as hell.
Order your at-home combo test kit here and take that next step with confidence, not fear.
FAQs
1. Can itching really be the only symptom of an STD?
Yes, and that’s what throws people off. You don’t need a full outbreak, burning pee, or wild discharge to have something going on. Herpes, trich, even early chlamydia can all start with nothing more than an annoying little itch. If it feels new or just off, trust that gut feeling and check it out.
2. How long should I wait before panicking about genital itching?
Let’s skip the panic and go for curiosity instead. If it’s day one after shaving or hot yoga? You’re probably fine. But if it’s been more than 3–5 days and it’s still driving you up the wall, especially with no obvious cause, it’s time to test or call in a pro. Your peace of mind is worth it.
3. Can razor burn or friction feel like an STD?
All the time. Ingrown hairs, micro-cuts, heat rash, they all throw people into a WebMD tailspin. But they usually clear up fast (a few days max). If you’re still itchy a week later or it starts stinging instead of healing, don’t just guess. Test.
4. Does everyone with herpes get blisters?
Nope. In fact, many people never see a single sore. Sometimes it’s just a weird tingling or dryness that comes and goes. That’s why herpes spreads so easily, people don’t always know they have it. If you’ve had unprotected sex and a mystery itch pops up, herpes should be on the rule-out list.
5. I tried yeast meds, but I'm still itchy. Now what?
If the cream didn’t work, don’t assume you need a stronger one, assume you might have misdiagnosed. BV, trich, and even allergic reactions can mimic yeast infections. If you’re treating the wrong thing, it won’t go away. A test clears that up fast.
6. I tested negative but the itch is still there. Could the test be wrong?
It could be too early. Or the itch might not be from an infection at all. If you tested before day 10 or 14 after exposure, some STIs won’t show up yet. Recheck your timeline, or better yet, plan to retest at the two-week mark if you're still unsure.
7. Do condoms stop all kinds of genital itching?
Not quite. They block fluid-based infections like chlamydia and gonorrhea, but skin-to-skin spreaders like herpes or HPV? Less so. Plus, some folks are sensitive to latex, spermicide, or even lube ingredients. So yes, you can itch even if you played it safe.
8. Can oral sex cause itchy STDs?
Yep. Herpes is the big one here, it can pass mouth-to-genitals even if the giver doesn’t have visible sores. Gonorrhea and syphilis can show up this way too. If the itch followed a no-condom oral session, it’s not “just dryness.” Get tested to be sure.
9. I feel weird bringing this up to a partner. Do I have to?
No one wants to say, “Hey, so… my junk’s itchy.” But if you’re testing or suspect something, a simple heads-up goes a long way. You don’t need a diagnosis to open the convo. Try: “I’m checking on a symptom just to be safe, I’ll keep you in the loop.” It’s not TMI. It’s maturity.
10. Can stress really cause all this?
Short answer: yes. Stress messes with your immune system, hormones, and skin. It can even trigger flare-ups of conditions like eczema or herpes. But that doesn’t mean it’s all in your head. Stress is a factor, not a fake-out. If you’re under pressure and itchy, look at both sides: body and brain.
You Deserve Answers, Not Assumptions
If you’ve made it this far, you’re probably tired of second-guessing your own body. That’s valid. Testing doesn’t mean you’re promiscuous. It doesn’t mean you’ve done something wrong. It means you care enough to face the truth, whatever it is, with clarity and courage.
Don’t wait and wonder, get the clarity you deserve. This at-home combo test kit checks for the most common STDs discreetly and quickly.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate.
Sources
1. Planned Parenthood – Herpes Info
2. Cleveland Clinic – Genital Itching Guide
5. Vulvar Pruritus: A Review of Clinical Associations – PMC
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: Janelle R., NP, MPH | Last medically reviewed: October 2025
This article is meant to be informative only; it should not be used in place of medical advice.










