The Missing Test on Most “Full” STD Panels
When most people get tested for STDs, they assume they’re being screened for everything: chlamydia, gonorrhea, syphilis, HIV, HPV, and herpes. But unless you specifically ask, or you’re already showing symptoms, your doctor likely won’t screen you for Herpes Simplex Virus (HSV).
This applies to both HSV-1 (usually oral) and HSV-2 (usually genital). Even though nearly half of U.S. adults carry HSV-1, and one in eight have HSV-2, herpes remains a blind spot in sexual health care.
According to CDC guidelines, routine herpes testing isn’t recommended for asymptomatic people. And the U.S. Preventive Services Task Force (USPSTF) gives routine screening for HSV a “D” rating, meaning they actively recommend against it in the general population.

People are also asking: How do I know if antibiotics are working?
Why the Medical System Leaves Herpes Out
The official reasoning behind skipping herpes testing boils down to three main factors:
- Test Accuracy Concerns: Blood tests for HSV detect antibodies, not the virus itself, and can sometimes produce false positives, especially with low exposure risk or early infections.
- No Cure, Limited Treatment: Because herpes is a lifelong virus that’s often asymptomatic, many providers believe a positive result would create more emotional harm than medical benefit.
- Stigma & Mental Health: Doctors worry that diagnosing a patient with herpes might cause unnecessary anxiety or shame, especially if the person might never experience symptoms.
But here’s what they’re not telling you: people aren’t anxious because they’re diagnosed. They’re anxious because no one talks about it.
When healthcare providers avoid herpes testing, they’re not protecting patients; they’re keeping them in the dark. And that silence? It’s fertile ground for misinformation, misdiagnosis, and emotional fallout.
The Hidden Toll of Not Knowing
Herpes isn’t dangerous for most people, but it’s emotionally loaded. And not knowing your status can come at a real cost:
- Transmission Without Consent: You could unknowingly pass HSV to a partner who assumes you’re negative.
- Surprise Diagnoses: Many people first find out they have herpes during a painful outbreak, or after giving it to someone else.
- Mental Health Spiral: The shock of an unexpected diagnosis can trigger shame, guilt, depression, and suicidal ideation, especially if you assumed you were tested.
“I felt so betrayed. I asked my doctor to test me for everything before I slept with my new partner. A year later, I had an outbreak and tested positive for HSV-2. Turns out I was never tested for it in the first place.” Sasha, 29
You deserve the right to know your status. Period. Whether you’re symptomatic or not.
Why You Should Still Ask for the Test
Just because it’s not routine doesn’t mean it’s not important. You may want to request herpes testing if:
- You’ve had unprotected sex or oral sex with a new partner
- Your partner has tested positive or gets cold sores
- You’re starting a new relationship and want full disclosure
- You’ve had unexplained symptoms (itching, bumps, burning)
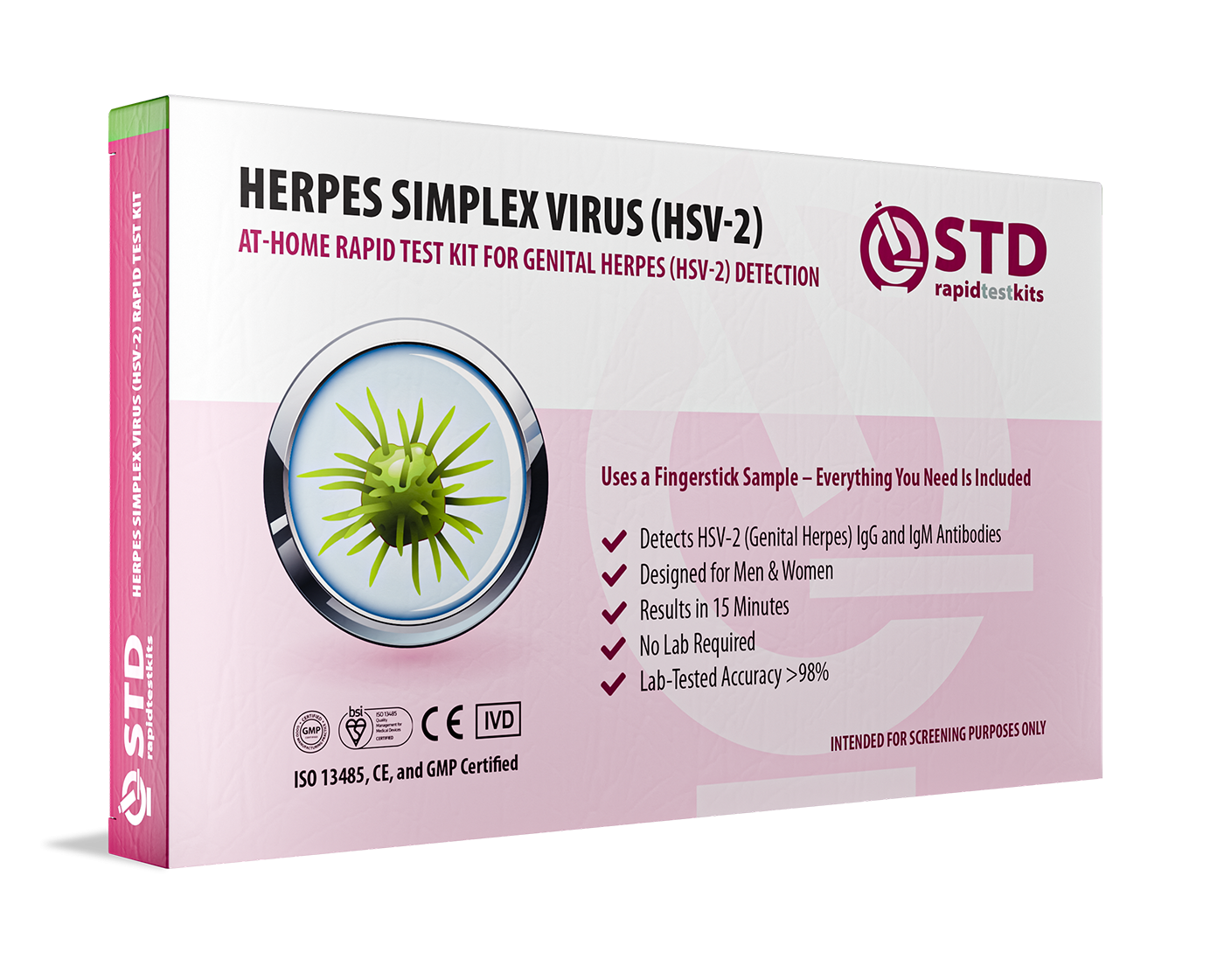
Even if you don’t have symptoms, a type-specific herpes antibody test can give you valuable information. And if you’re unsure about asking your doctor, or you want privacy, there’s always the option to use an at-home Herpes Home Test Kit that screens for HSV-1 and HSV-2 discreetly and accurately.
Check Your STD Status in Minutes
Test at Home with RemediumGenital Herpes Test Kit
 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $45.99 $49.00
How Reliable Are Herpes Tests, Really?
This is where things get tricky. Most herpes blood tests (called type-specific IgG antibody tests) detect whether your body has developed antibodies to HSV-1 or HSV-2. But these tests aren’t perfect.
Here’s what you need to know:
- Window Period: It can take up to 12–16 weeks after exposure for herpes antibodies to show up in your blood.
- False Positives: Especially for HSV-2, low-positive results (index values between 1.1 and 3.5) may be false. Some labs use a second confirmatory test, but not all do.
- No Info on Location: A positive HSV-1 test doesn’t tell you if it’s oral or genital; it just confirms exposure.
Despite the limitations, these tests are still useful, especially when interpreted by someone who understands the nuances. And they can offer huge peace of mind when you’re navigating new relationships, unexplained symptoms, or post-exposure anxiety.
What Happens If You Test Positive?
A positive herpes result can feel like a gut punch, especially if you had no symptoms. But it’s not the end of your sex life, your desirability, or your health. Not even close.
Here’s what comes next:
- Learn the Type: HSV-1 is most commonly oral but can be genital. HSV-2 is usually genital and more likely to recur.
- Talk to a clinician: They can help interpret your results, suggest antivirals, and discuss what (if anything) you need to change.
- Disclose to Partners: This can feel scary, but most people are more understanding than you think. And being honest builds trust.
- Decide on Treatment: Daily suppressive therapy isn’t always necessary, but it can reduce outbreaks and transmission risk.
Herpes is manageable. What’s unmanageable is being blindsided and unsupported. Testing gives you clarity, and clarity gives you control.
How to Ask Your Doctor for a Herpes Test Without Shame
It’s okay to be nervous. Herpes still carries stigma, and many people feel judged just for asking. But you have every right to advocate for your own health.
Here’s a script you can use:
“I’d like to be tested for herpes, even if I don’t have symptoms. Can you order a type-specific IgG blood test for both HSV-1 and HSV-2?”
If they push back, stay calm. You can say:
“I understand the test isn’t perfect, but I’d feel more comfortable knowing my status. I’d prefer to test and make informed decisions.”
Still getting resistance? That’s your cue to find another provider or go with a discreet Herpes 2 Rapid Test Kit you can use from home.

People are also asking: Can I treat gonorrhea with leftover antibiotics?
The Emotional Fallout No One Talks About
Testing for herpes isn’t just a medical decision, it’s an emotional one. For many people, a positive result opens up a floodgate of grief, shame, rage, or deep insecurity. It can feel like your whole identity shifts in a moment.
But here’s what thousands of people have learned, often the hard way:
- You’re still lovable. This virus doesn’t change your worth.
- You’re not alone. More than 500 million people globally carry herpes.
- You’re still sexually empowered. Herpes doesn’t make you “unsafe.” Being honest and informed does.
“I was devastated at first. But after the second date where I disclosed, and he said, ‘Thanks for telling me. That doesn’t change how I feel’; I started healing. I realized I wasn’t dirty. I was just human.”
Devon, 31
The stigma will die faster if we stop treating herpes like a shameful secret and start treating it like the incredibly common, manageable virus it is.
A Brief History of Herpes Testing (and How We Got Here)
Herpes has been around for thousands of years, but routine blood testing for HSV is relatively new and still controversial.
In the early 2000s, type-specific IgG antibody tests became widely available. Before that, herpes diagnosis mostly relied on physical symptoms and viral cultures. But as testing expanded, so did confusion, especially when patients began testing positive with no symptoms and no clear answers.
This led to widespread concern about false positives, unnecessary anxiety, and overdiagnosis. That’s when major medical bodies, like the USPSTF, started advising against routine herpes testing in the general population.
But here’s the rub: just because a test isn’t routine doesn’t mean it’s not helpful. And just because the system isn’t built for proactive herpes care doesn’t mean you can’t demand it anyway.
Common Misconceptions About Herpes Testing
“If I had herpes, it would’ve shown up on my STD test.”
Not unless you asked for it. Herpes isn’t included in most panels.
“Doctors must know best, they wouldn’t skip a test I need.”
Sometimes providers follow protocol, not patient preference. You still have to advocate for yourself.
“If I test positive, I’ll never be able to date again.”
Many people with herpes are in loving, fulfilling relationships. Disclosure is tough, but rejection isn’t inevitable.
“Herpes isn’t a big deal, so testing doesn’t matter.”
It might not be a medical emergency, but knowing your status is part of sexual integrity and informed consent.
Check Your STD Status in Minutes
Test at Home with RemediumGenital & Oral Herpes Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $75.00 $98.00
For all 2 tests
“Wait… So My Doctor Never Tested Me for Herpes?”
Yup. That’s the wild truth most people don’t learn until years later, routine STD panels almost never include herpes testing. Even if you asked for “the full panel.” Even if you had symptoms. Even if your partner tested positive.
Unless you specifically asked for it, and even then, some doctors might push back, HSV-1 and HSV-2 blood tests are usually skipped. Why? Because of stigma. Because of outdated guidelines. Because some providers still think “it’s not clinically necessary.”
The result? You walk around assuming you’re “clean,” while unknowingly carrying something as common as HSV-1. It’s frustrating, and it’s not your fault. The system wasn’t built to give you the full picture. That’s why so many people find out years later, only after a partner has a flare-up… or a cold sore turns into something more.
If that’s you, if you’re sitting there thinking, “How did I not know this?”, please know: you’re not alone. And you’re not behind. The smartest thing you can do now is take control of your own testing timeline.
Herpes Isn’t “Too Complicated” to Test For; It’s Just Inconvenient for the System
Let’s bust a harmful myth: the idea that herpes is “too complicated” to diagnose, so it’s better left alone. That’s medical laziness. Yes, HSV-1 and HSV-2 tests can come with nuances. A positive doesn’t always mean active infection. It doesn’t tell you when you got it. But that doesn’t make testing useless; it just means the results need context.
Imagine if we used that logic for other STDs. “Oh, you might test positive for HIV but not have symptoms, so let’s not test you.” Sounds ridiculous, right? Yet this is still the approach with herpes in many clinics today.
The truth? People want answers. They want to know what’s in their body. They want to protect their partners, take suppressive meds if needed, and make informed choices. That’s not paranoia, that’s responsible sex.
Testing at home puts you back in control. Because knowing your status is always better than guessing.

People are also asking: Should I tell my next partner I had an STD before?
FAQs
1. Why isn’t herpes included in routine STD testing?
Because of high prevalence, potential for false positives, and lack of symptoms in many people, the CDC and USPSTF recommend against routine screening.
2. Can I still get tested if I don’t have symptoms?
Yes. You can request a type-specific blood test or use an at-home test for HSV-1 and HSV-2.
3. How soon after exposure can I test?
It may take up to 12–16 weeks for herpes antibodies to show in your blood. Earlier tests may miss new infections.
4. What’s the difference between HSV-1 and HSV-2?
HSV-1 usually causes oral herpes (cold sores), while HSV-2 is typically genital. Both can infect either area through oral sex.
5. Can I get a false positive?
Yes. Especially for HSV-2, low positive results (1.1–3.5) may require confirmatory testing for accuracy.
6. Is there a cure for herpes?
No, but antiviral meds can reduce outbreaks and transmission. Many people live symptom-free.
7. Should I tell my partner I have herpes?
Yes. It’s part of honest, ethical sexual communication. And it allows your partner to make informed decisions.
8. Can I get tested without going to a doctor?
Yes. At-home herpes test kits are private, reliable, and widely available.
9. Will herpes show up in urine or swab tests?
Only during an active outbreak. Otherwise, blood tests are used to detect antibodies.
10. Is HSV-1 on the rise in the genitals?
Yes. More people are getting genital HSV-1 from oral sex, especially among younger adults.
If It Matters To You. Ask For It.
You’ve probably heard this before: “If it matters to you, ask for it.” But when it comes to herpes testing, that’s not just advice, it’s a necessity.
The medical system may not prioritize herpes screening, but that doesn’t mean you can’t. Knowing your status isn’t about panic or paranoia; it’s about power. It’s about honesty. It’s about protecting your partners and your peace of mind.
Herpes isn’t rare. It isn’t dirty. And it isn’t something to be ashamed of. But it is something you deserve to know about, on your own terms, in your own timeline, and with the support you need to navigate it.
You’re allowed to ask. You’re allowed to care. And you’re allowed to get tested, even if no one offers it.
Sources
1. Planned Parenthood: Herpes Info
2. American Sexual Health Association: Herpes Overview
4. American Sexual Health Association – Task Force Decides Against Routine Herpes Screenings










