When You Should Get Tested (Hint: Not Just Once)
First: Yes, you should get tested. Even if you wore a condom. Even if you feel fine. Even if it was just once.
STDs don’t always show up right away, some need time to incubate before becoming detectable. This is called the window period. For example:
- Chlamydia/Gonorrhea: usually detectable in 5–7 days
- HIV (antigen/antibody test): best detected after 2–4 weeks
- Syphilis: 3–6 weeks for antibodies to appear
- Herpes: may take weeks or months to show in blood tests
Your best bet? Test now, then again in 2–3 months.
People are also looking for: Will an STD affect my fertility?
What to Expect Emotionally (Yes, That’s Part of It)
STDs don’t just mess with your body, they hijack your brain. Guilt. Rage. Shame. Obsession. Even if you’re not infected, the emotional toll can feel brutal.
This is normal. You may cycle through anger at your partner, shame toward yourself, and even relief that they told you at all. Some people don’t. But you get to feel all of it, and still deserve care.
One tip: Talk it out with someone you trust. A friend, a therapist, or even an anonymous hotline. You don’t have to go through this alone.
The Silent Danger: Why You Can’t Rely on Symptoms
Here’s the kicker: most STDs don’t show symptoms right away, and some never do.
Chlamydia is infamous for staying silent. HPV can take years to reveal itself. Gonorrhea might show signs in men, but often hides in women. Just because you feel fine doesn’t mean your body is.
Only testing tells the truth. Not guessing. Not waiting. Not Googling photos at 2AM. (Don’t do that.)
What Type of Test Should You Take?
Let’s be blunt: not all STD tests are the same. And the right test depends on what you were exposed to, and how.
Here’s what most people need after potential exposure:
- Urine or swab test: For chlamydia and gonorrhea (genital, oral, or rectal depending on contact)
- Blood test: For HIV, syphilis, and herpes (usually type 2)
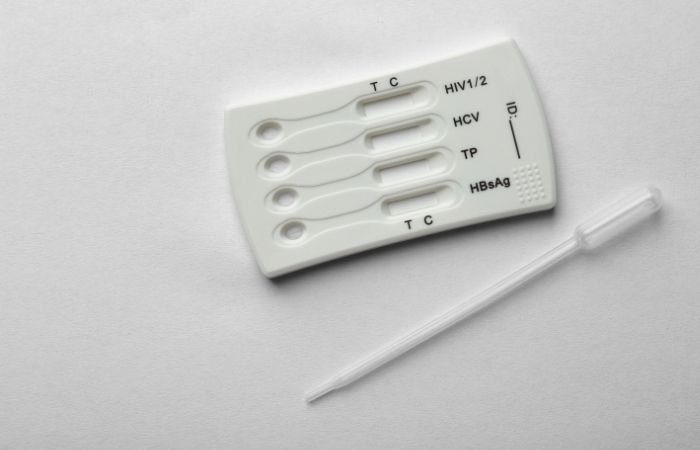
- Rapid combo kits: Home kits like the Complete 8-in-1 STD At-Home Rapid Test Kit screen for multiple infections at once
If oral or anal contact was involved, make sure the clinic knows. Many infections hide in the throat or rectum, and standard urine tests won’t catch them.
Check Your STD Status in Minutes
Test at Home with Remedium7-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $129.00 $343.00
For all 7 tests
What If It Was Oral or Anal Sex?
Quick reality check: STDs aren’t picky about body parts. Oral and anal sex carry serious risk, especially for gonorrhea, syphilis, herpes, and HPV.
That sore throat might not be just allergies. If your partner had an STD and you went down on them, ask for oral swab testing. It’s not always offered unless you request it.
The same goes for anal exposure, symptoms are rare, but infection rates are high. Include rectal swabs in your testing plan if relevant.
How Much Risk Are You Actually Facing?
Let’s talk odds, without sugarcoating. If your partner has an STD, your risk depends on:
- The type of STD: Some are easier to transmit than others. HIV and syphilis pass through blood or sores; chlamydia and gonorrhea spread through fluids.
- Your protection use: Condoms reduce risk but don’t eliminate it, especially for skin-to-skin STDs like herpes or HPV.
- The sex act itself: Anal sex carries higher transmission rates for HIV and gonorrhea; oral sex still carries risks, just lower.
Here’s a general idea of risk if you didn’t use protection:
- Chlamydia: ~40–60% chance of passing during vaginal/anal sex
- Gonorrhea: ~50% risk per act for receptive vaginal or anal sex
- Herpes: ~10% risk per sexual act, even with no symptoms
- HIV: ~1 in 250 chance from vaginal sex, higher for anal (up to 1 in 70)
Bottom line: You’re not guaranteed to catch something, but you’re not guaranteed safe either. Testing is your reality check.
Why Retesting Matters (Even After a “Negative”)
Here’s where most people get tripped up. You take a test right away, it’s negative. You exhale. You move on.
Bad move. Many STDs don’t show up immediately. That’s why experts recommend a follow-up test 2 to 3 months after your last exposure, even if your first test is clear.
This is especially crucial for HIV, syphilis, hepatitis B/C, and herpes. These viruses have longer window periods. The CDC backs this up: “If exposed to HIV or syphilis, retesting is recommended at 90 days post-exposure.”

People are also looking for: How do I know if I have trichomoniasis?
What Is “Expedited Partner Therapy” and Does It Help You?
If your partner has chlamydia or gonorrhea, you might hear about something called Expedited Partner Therapy (EPT). It allows a provider to give your partner treatment, and send you meds too, without you needing your own appointment.
It’s legal in most U.S. states and backed by the CDC as a proven way to stop reinfection. But it’s not a replacement for testing. You could have multiple infections, or none at all. Only a test can tell.
Still, if you’re offered treatment: take it. Then test. Then retest.
Case Study: “He Said He Had Herpes After We Hooked Up...”
“It was a one-night thing. Great chemistry, tons of trust, until the next morning.” , Kayla, 29
Kayla met a guy while traveling. They hooked up. He told her the next day he had genital herpes, and had been on antivirals, but hadn’t mentioned it beforehand.
“I was furious. Not because he had it, but because he didn’t tell me. I felt violated,” she says. “But I still cared enough to ask how he managed it.”
Kayla got tested immediately, then again three months later. She stayed negative, but not without some hard emotional fallout.
“The worst part wasn’t the STD risk. It was realizing how little I’d asked, how much I’d assumed.”
Now she talks openly about herpes in her relationships. “It doesn’t scare me anymore. But silence? That still does.”
Common Misconceptions That Keep People From Getting Tested
Let’s bust a few myths that stop people from protecting themselves:
“If I don’t have symptoms, I must be fine.”
False. Most STDs are asymptomatic, especially early on.
“If my partner got treated, I’m safe too.”
Nope. You may not have the same infection, or you could pass it back.
“We used a condom, so I’m immune.”
Condoms help, but they don’t block everything, especially skin-to-skin STDs like herpes and HPV.
“I only need to test once.”
If you were exposed, you may need follow-up testing depending on the STD’s window period. Knowledge isn’t just power, it’s protection. Testing doesn’t make you dirty. It makes you responsible.
Check Your STD Status in Minutes
Test at Home with Remedium3-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $69.00 $147.00
For all 3 tests
FAQs
1. Can you get an STD after one encounter?
Yes. Some STDs can be transmitted after a single sexual contact, especially chlamydia, gonorrhea, or herpes.
2. Should I wait before testing?
Yes, for most accurate results. Some infections take days or weeks to show up. Consider testing now and again in 2–3 months.
3. What if I used a condom?
Condoms reduce but don’t eliminate all risk, especially for STDs that spread via skin-to-skin contact like herpes and HPV.
4. What tests should I ask for?
Ask for urine, swab, and blood tests. Include throat or rectal testing if oral/anal sex occurred.
5. Can I get treated without testing?
In some cases (like chlamydia), yes, through Expedited Partner Therapy. But testing is still recommended.
6. Do STDs always show symptoms?
No. Most don’t. You could carry and spread an STD without knowing.
7. How much does STD testing cost?
Costs vary. At-home kits like those from STD Rapid Test Kits are discreet and affordable.
8. How long should I wait before retesting?
If exposed to HIV or syphilis, retest after 3 months. Many STDs need a follow-up test.
9. Is at-home testing accurate?
Yes, if you use FDA-approved kits from trusted providers like STD Rapid Test Kits.
10. What if I test positive?
Get treated promptly. Many STDs are curable. For chronic ones like herpes or HIV, early care makes a huge difference.
Final Thoughts: You’re Not Dirty, You’re Just Human
You slept with someone who has an STD. That doesn’t make you reckless, dirty, or broken, it makes you part of the 1 in 2 sexually active adults who’ll face this reality at some point.
The most powerful thing you can do right now is act: test, treat if needed, and talk openly. It’s not about shame, it’s about care. For yourself, and for whoever comes next.
You don’t have to go to a clinic, explain yourself to a stranger, or wait in judgmental silence. You can get tested from home, on your terms. Quietly. Quickly. Accurately.
Because your health is yours, and you deserve answers, not anxiety.
Sources
1. CDC STD Screening Guidelines
2. Mayo Clinic: STD Testing Overview
3. Healthline: When to Get Tested for STDs
4. Lancet HIV: Testing Frequency and Risk










