Quick Answer: A new study makes it clear that injectable Cabotegravir and Rilpivirine is effective for seniors in controlling their HIV. This spells good news for seniors because one may expect fewer daily oral medications to become a reality very soon. Discreet home-based testing for HIV is required to take care of seniors between their injectable doses.
In August 2025, Open Forum Infectious Diseases published a cohort study observing older individuals’ response to injectable antiretroviral therapy for HIV infections. The injectable formulation of Cabotegravir and Rilpivirine administered every two months demonstrated excellent viral suppression rates even for seniors aged 60+. It is easy to see why this is especially significant for patients struggling to cope with more than one condition or struggling to continue their treatments.
We’re building on that news. This article unpacks what this new data means for aging HIV-positive populations, how at-home testing plays a supporting role in this treatment shift, and why long-acting regimens don’t replace monitoring, they just change how we approach it. We’ll walk through what counts as an STD test, the latest on window periods and timing, accuracy trade-offs between rapid and lab-based options, and how to time retesting if you’re switching therapies or living with a chronic diagnosis.

People are also reading: Yes, You Can Get an STD From a Vibrator (Even If It Was Just You)
Who This Guide Is For (And Why It Matters)
If you’re over 50 and living with HIV, or caring for someone who is, you already know the healthcare system wasn’t built with your experience in mind. You might be balancing multiple medications, clinic fatigue, or that creeping sense of “I just don’t want to take one more pill.” For some, every dose brings a reminder of a diagnosis they’ve carried for decades. For others, privacy, mobility, or even transportation to appointments is a daily hurdle.
This is where long-acting treatments change the game. But fewer pills doesn’t mean fewer responsibilities. This guide is for older adults living with HIV, people newly diagnosed at midlife or beyond, and anyone using or considering long-acting injectable therapy. We’ll talk about how to time your testing, whether at home or in clinic, what to expect from different test types, and how to stay ahead of complications. We’ll also break down how at-home testing, especially during gaps between injections, can keep you informed, empowered, and in control.
What Actually Counts as an STD Test?
Let’s be clear: not all tests are created equal. If you’ve been living with HIV for a while, you’ve probably had every type of test imaginable, blood draws, swabs, urine samples, and fingersticks. But as you transition to a new regimen, knowing which test does what becomes even more important.
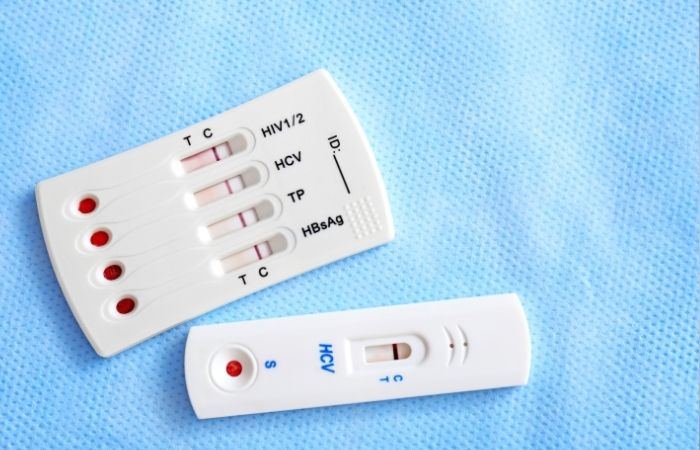
For HIV, most diagnostic tests fall into three buckets: NAAT/PCR tests (which detect genetic material), antigen/antibody combo tests (which detect early-stage infection), and rapid tests (which often use lateral flow to detect antibodies). According to the CDC’s current testing guidelines, the gold standard for early HIV detection and viral load monitoring remains lab-based NAAT testing. But for many at-home users, FDA-approved oral swab or fingerstick rapid tests are a discreet, quick, and private way to monitor status.
Here’s where that matters: if you're on a long-acting injectable regimen, you may go weeks without visiting a clinic. Self-testing becomes your tether. A quick at-home test halfway between injection appointments can offer peace of mind or flag a problem early. You can explore discreet options through STD Rapid Test Kits or order a private kit to stay on top of your status.
Window Periods: What to Know for Each STD
Even if you’re virally suppressed and stable on treatment, timing still matters. “Window period” refers to the time between exposure to an infection and when a test can reliably detect it. If you test too early, whether for HIV, syphilis, or any other STD, you might get a false negative even if you're infected.
This gets more complex as you age. Immune response can slow slightly, and the timing of your last injection may influence how and when viral rebound could occur (in the rare case of missed appointments or resistance). Understanding window periods helps you avoid false reassurance and time your at-home or clinic-based tests more effectively.
| STD | Common Test Type | Sample | Typical Window Period | When Accuracy Peaks |
|---|---|---|---|---|
| HIV | Ag/Ab combo or NAAT | Blood or oral fluid | 2–6 weeks (Ag/Ab), 10–33 days (NAAT) | 6–12 weeks |
| Syphilis | Antibody (treponemal) | Blood | 3–6 weeks | 6–12 weeks |
| Chlamydia | NAAT | Urine or swab | 7–14 days | 14+ days |
| Gonorrhea | NAAT | Urine or swab | 7–14 days | 14+ days |
| Trichomoniasis | NAAT or Rapid antigen | Swab or urine | 5–28 days | 2–4 weeks |
Figure 1. Window periods for common STDs and HIV. This timing helps you avoid testing too early, and missing the chance to detect an infection.
Rapid Test vs Lab Test: Pros, Cons, and Tradeoffs
Imagine two different mornings. In one, you’re pacing your kitchen, heart pounding, waiting for a rapid HIV test result to develop in your hand. In the other, you’re driving two hours to a clinic for a lab draw, worried about who might see you walk in. Both are real. Both matter. And both have different strengths.
At-home rapid tests offer privacy, speed, and accessibility. But their sensitivity can be lower than lab-based tests, especially early in an infection. That said, if you’re stable on a long-acting injectable regimen and looking to confirm suppression or detect viral rebound, a rapid self-test is a powerful tool between appointments.
| Method | Privacy | Speed | Sensitivity/Accuracy | Good Fit When |
|---|---|---|---|---|
| At-Home Rapid | Very high | Results in ~20 minutes | Moderate–High (best after 90-day window) | You want privacy and fast feedback between injections |
| Mail-In Lab | High | 1–3 days after mailing | High (NAAT or Ag/Ab) | You need confirmation or earlier detection post-exposure |
| Clinic Visit | Moderate | Same-day to a few days | Very high (NAAT, antigen, antibody panels) | You have symptoms, need confirmatory care, or can’t test alone |
Figure 2. Comparison of HIV and STD testing methods. Each has a place, what matters is what you need right now.
When to Test After Exposure
If you’ve just had a possible exposure, whether through condom break, needle sharing, or a partner who recently tested positive, it’s tempting to test right away. But testing too soon can give you a false sense of security.
If it’s been less than 5 days, most tests won’t detect infection yet. It’s better to wait unless you’re experiencing acute symptoms (like fever, rash, or swollen lymph nodes) or were exposed in a high-risk situation. In that case, seek clinical care immediately for possible PEP (post-exposure prophylaxis).
If it’s been 7 to 13 days, you can begin testing with some early detection tools, like NAAT or antigen/antibody combo tests, though you’ll likely need a follow-up test. After 14 days, accuracy improves dramatically, especially for standard self-tests.
Case study: A 62-year-old man on a stable injectable regimen took a rapid test 5 days after his partner disclosed a new diagnosis. It came back negative. Two weeks later, he tested again, this time, positive. Because he caught it early, he was able to resume his injection cycle after starting short-term treatment. Testing at the wrong time almost led him to skip care.
Check Your STD Status in Minutes
Test at Home with RemediumHIV Rapid Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $33.99 $49.00
Do You Need to Retest? Here’s How to Know
If you’re switching regimens, or you’ve had a break in care, retesting is often essential. After treatment, residual virus fragments can lead to false positives if you test too soon. Without treatment, or if you missed an injection, a 30-to-45-day retest window can help you catch issues early.
Scene: Latrice, 68, forgot to go in for her 2-month injection while traveling. When she returned, she wasn’t sure whether to wait for her next appointment or test at home. She used a rapid self-test and was shocked to get a reactive result. It turned out her viral load had rebounded. Her provider restarted therapy and adjusted her schedule. That self-test gave her an early warning.
Bottom line: even if you’re on an injectable, you still need testing. Use it as a check-in, not a punishment.
Privacy, Shipping, and Discreet Support
If you’re ordering tests online, you might wonder: will my roommate see? Will the box say “HIV” on it? Can I control the timeline? The answer is yes, you can stay in charge.
Our kits arrive in unmarked packaging. There’s no branding or label that reveals what’s inside. You can track your delivery, and many customers report getting their results within 24 to 72 hours of testing, depending on whether they use rapid kits or mail-in options.
For older adults, this control matters. Maybe you live with adult children, a partner who doesn’t know your status, or caregivers who aren’t in the loop. Discreet, fast, and private options mean you can monitor your health without navigating extra stigma or risk. This is especially helpful during travel, caregiving transitions, or between regular injection appointments.
What If You Test Positive?
If a self-test comes back positive, whether you're on injectables or not, it’s easy to feel a wave of panic. Take a breath. Testing positive doesn’t mean your treatment failed, and it doesn’t mean you’re infectious right away. But it does mean it’s time to act.
Start with confirmatory testing, especially if it’s been a while since your last clinic visit. If you’re already diagnosed and managing HIV, a positive test could mean your viral load has increased due to a missed injection, resistance, or another health change. According to HIV.gov's test result guidance, any unexpected result should be reviewed with a provider right away.
Scene: A 65-year-old woman living alone in rural Texas missed her injection by two weeks after a flood cut off access to her clinic. She felt fine but used an at-home test just to be sure. The result was positive. She contacted her provider, who confirmed the viral rebound and helped her resume injections with additional labs. The self-test turned out to be her safety net.
Don’t wait to see if it “fixes itself.” The earlier you catch viral load changes, the easier it is to regain control, and stay undetectable.
People are also reading: Polyamory and STDs: What Testing Looks Like With Multiple Partners
FAQs
1. Is this really safe for people in their 60s, 70s, or older?
Absolutely. The latest real-world data showed strong viral suppression in folks aged 60 and up using the Cabotegravir + Rilpivirine injection combo. These aren’t just stats, they’re people navigating aging, other meds, and decades of HIV care. For many, this regimen lightens the load. But like anything medical, talk to your provider to see if it fits your story.
2. Does switching to injections mean I’m done testing forever?
Not quite. Think of injections as shifting the rhythm, not ending the song. You’re no longer taking a pill every day, but that doesn’t mean you skip all monitoring. At-home tests give you a way to check in between injections, especially if something feels off or you’re between appointments. It’s not about paranoia; it’s about staying ahead.
3. How often should I self-test now that I’m on injectables?
There’s no one-size-fits-all rule, but a good habit is to self-test once between each injection, so if you’re getting jabbed every two months, test once about halfway. Think of it like checking the oil in your car before a road trip. You hope it’s fine, but you’ll sleep better knowing.
4. What if my self-test suddenly shows a positive result?
First: breathe. Don’t jump to conclusions. A positive at-home result could mean a few things, and it doesn’t necessarily mean full-blown failure of your treatment. But it does mean you should call your provider and get confirmatory lab testing. Early action is everything here.
5. Can I use self-tests to track my viral load?
Not directly. Most home kits look for antibodies or antigens, not actual viral load numbers. But if you’re someone who’s usually undetectable and suddenly gets a reactive result, that’s a red flag worth following up. At-home tests are a flashlight, not a microscope.
6. I missed my injection. Now what?
Life happens. Maybe you forgot, maybe the bus didn’t come, maybe your clinic flooded, we’ve seen it all. The important thing is not to ignore it. If you’re late by more than a few days, contact your provider. Use a self-test in the meantime if you’re worried. Missing one dose isn’t the end, but going radio silent might be.
7. Are the injection side effects bad?
Most people report mild stuff, soreness at the site, maybe a little swelling or tenderness. It’s kind of like a flu shot but beefier. Very few people stop the treatment because of it. In studies, even older adults with sensitive skin or mobility issues handled it just fine.
8. Is this covered by insurance or Medicare?
Often, yes. Coverage is expanding fast, especially under Medicare Part D and many private plans. Your clinic or a telehealth service can walk you through the paperwork. Don’t assume you’re on the hook for everything, ask. There are support programs out there.
9. Am I still contagious while on this treatment?
If you’re undetectable, you’re untransmittable. That’s the U=U rule. These injections are designed to keep you there, as long as you stay on schedule. So no, you’re not passing anything on, even during sex, if your viral load stays suppressed. That’s not a promise, it’s public health fact.
10. Can I actually use an at-home test by myself?
Most people can, yes. The kits are designed for solo use, no lab coat required. That said, if you have trouble with vision, fine motor control, or anxiety about doing it right, ask a trusted partner, friend, or caregiver to walk through it with you. Taking control doesn’t mean doing it alone.
You Deserve Ease, Not More Appointments
So here is the bottom line: making the transition to long-acting injectables could make your care simpler and reduce your cognitive load associated with taking daily oral medication, but it does not mean moving away from your care management but rather readjusting your care management to your life and not vice versa.
At-home HIV self-testing kits take care of your need to know without all the aggravation. You can treat them as part of your wellness cycle: When's your BP reading? When's your mammogram? When's your med refill reminder? It's especially helpful if you're struggling with aging, complicated health concerns, or just plain old burnout to have something give you a little bit of your power back.
Don’t wait and wonder, get the clarity you deserve. This discreet HIV test kit lets you check your status at home, on your terms, in just minutes.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted six of the most relevant and reader-friendly sources.
Sources
1. Long-Acting Cabotegravir and Rilpivirine in Seniors: Open Forum Infectious Diseases
2. EATG: Long-Acting HIV Combo Maintains Control in Seniors
3. Cabotegravir and Rilpivirine in Aging Populations: PubMed Study Overview
4. HIV.gov – Understanding Test Results and Next Steps
6. The Lancet HIV – Defining Long-Acting Therapy Support Protocols
About the Author
Dr. F. David is a board-certified infectious disease specialist and author whose writing addresses STI prevention, diagnosis, and treatment. He brings precision and direct experience to his work and is committed to extending his reach to all communities; in both urban and off-grid environments..
Reviewed by: M. Collins, MPH | Last medically reviewed: November 2025










