Quick Answer: Testicle pain can be caused by infections (like STDs), torsion (a surgical emergency), injury, or even referred pain. Sudden, severe, one-sided pain with nausea may be torsion and needs ER attention. If pain builds gradually or includes discharge, infection is more likely, especially from gonorrhea or chlamydia.
Why Testicle Pain Triggers Panic
There’s a reason testicle pain can feel more urgent than other types of discomfort. Your testicles aren't just symbolic of masculinity, they’re delicate, vulnerable, and packed with nerve endings. When something goes wrong down there, your brain doesn’t wait to evaluate, it just screams: “Something’s WRONG.”
The problem is, not all testicle pain means the same thing. A dull ache after sex isn’t the same as sudden, stabbing pain while you're lying on the couch. And the cause of that pain could be anything from a minor strain to a twisted spermatic cord that cuts off blood supply. In short: your body’s alarm system is loud, but not specific. That’s where this checklist comes in.

People are also reading: How to Tell Someone You’re HIV Positive (Without Shame or Panic)
Step One: How the Pain Started Tells You a Lot
If the pain came on suddenly, without warning, and feels like someone kicked you in the groin, stop reading and go to the ER. That’s not an exaggeration. Sudden, severe, one-sided pain could be testicular torsion, a condition where the spermatic cord twists and cuts off blood flow to the testicle. You typically have six hours to save it. No pressure, right?
But what if it didn’t hit all at once? What if it came on gradually, or you only noticed it hours later during a shower? That’s more typical of an infection, especially if there’s any swelling, redness, discharge, or pain with urination. Epididymitis, often caused by chlamydia or gonorrhea, is one of the most common culprits, especially in sexually active men under 35.
Infections tend to build slowly. Torsion punches you in the gut out of nowhere. Here’s how the two usually compare:
| Feature | Testicular Torsion | Infection (e.g., Epididymitis) |
|---|---|---|
| Onset of Pain | Sudden, severe, often during rest | Gradual, over hours or days |
| Swelling | Often present, may appear quickly | Usually present, may feel warm or firm |
| Discharge or burning urination | Rare | Common, especially with STDs |
| Nausea or vomiting | Common (due to nerve pain) | Rare |
| Age most affected | Teens to early 20s | Late teens to 40s |
| Best action | ER now , may need emergency surgery | STD test and antibiotics within 24–48 hours |
Figure 1. Key differences between torsion and infection-related testicle pain, when time matters most.
Step Two: Is There Swelling, Redness, or Heat?
Gently feel around the affected area, ideally in a warm shower when the scrotum is relaxed. Is one side larger than the other? Does it feel hot to the touch? Is there redness or tenderness on the back of the testicle? These are classic signs of epididymitis, which is often linked to a recent STD exposure, especially unprotected sex or oral-genital contact.
But not all swelling is infectious. A condition called hydrocele (fluid buildup) or varicocele (enlarged veins) can also cause dull discomfort without any infection. They don’t need urgent care, but they do need diagnosis.
If it’s swollen and you also feel feverish or have urinary symptoms, there’s a good chance it’s an infection. That means antibiotics, not wishful thinking. Don’t wait for it to go away, it usually gets worse if untreated.
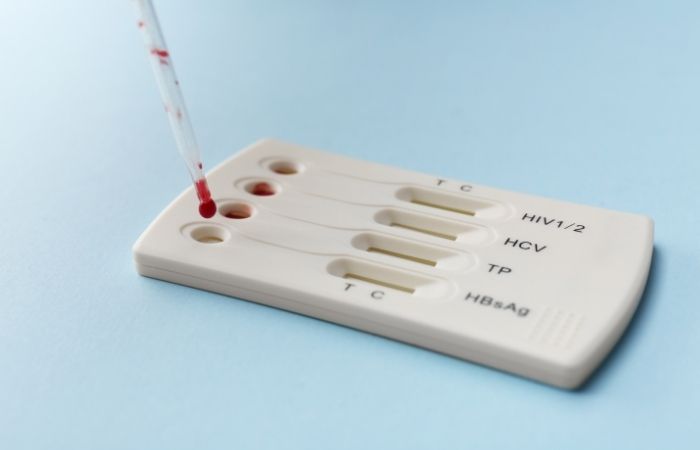
Check Your STD Status in Minutes
Test at Home with Remedium3-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $69.00 $147.00
For all 3 tests
Step Three: Could It Be Something Else Entirely?
Not all pain in the testicles is actually coming from the testicles. Weird, right? But it’s true. Sometimes the discomfort is “referred pain”, your body’s way of mixing up the message. Pain from the lower back, kidneys, prostate, or even a hernia can radiate into the scrotum and confuse the hell out of you.
If the pain feels deep in your lower abdomen or pelvis, or you’re also dealing with back pain or trouble peeing, don’t just focus on the testicle. A prostate infection or kidney stone could be the real culprit. Likewise, lifting something heavy and then feeling a tug or pressure down below? That could be an inguinal hernia, where part of your intestine pushes into the groin area.
This doesn’t mean you’re making it up. It means your nerves are cross-talking. And you need a provider who knows how to listen to the full story, not just the symptoms.
The Checklist: What to Watch For (and What It Might Mean)
It’s hard to think clearly when you’re in pain. So here’s a simplified guide. This checklist doesn’t replace a doctor, but it can help you make better decisions while you wait for care, or decide if you should head to urgent care, the ER, or grab an at-home test kit.
| If you have... | It could be... | What to do |
|---|---|---|
| Sudden, intense, one-sided pain + nausea | Testicular torsion | Go to the ER immediately (risk of losing testicle) |
| Gradual pain + swelling + discharge or burning pee | Epididymitis (often STD-related) | Test for chlamydia/gonorrhea and start antibiotics |
| A dull ache that comes and goes + visible veins | Varicocele (enlarged veins) | Book a urology consult, usually not urgent |
| Pain after heavy lifting + groin bulge | Inguinal hernia | Get checked for hernia; may need surgery |
| Pain after ejaculation or sex + pelvic pressure | Prostatitis or referred pelvic pain | See a provider; may need antibiotics or anti-inflammatories |
| Redness + fever + one testicle warm or tender | Infection (bacterial or viral) | Start antibiotics and test for STDs |
| No pain, but a hard lump inside the testicle | Possible testicular cancer | Get an ultrasound ASAP (not always painful) |
Figure 2. Symptom-based checklist comparing urgent and non-urgent causes of testicular pain.
“I Thought It Was Torsion. It Was Gonorrhea.”
Marcus, 22, had never had a serious health scare before. So when he woke up with sharp pain in his left testicle and a bit of swelling, his mind jumped to the worst. He googled “testicle pain sudden,” and torsion came up. His stomach dropped. He sat on the edge of his bed debating whether to call an ambulance or try urgent care.
He went in. The ER doctor examined him, did a urine test, and ordered an ultrasound. Turns out, he didn’t have torsion, but he did have a raging case of epididymitis caused by gonorrhea. The swelling, the aching, even the morning panic attack, it all tracked.
With antibiotics and rest, he was fine within a week. But the bigger takeaway? “I almost ignored it. If I had waited a few more days, it could’ve gotten a lot worse,” he said. “And I didn’t even know STDs could mess with your balls like that.”
Not Sure If It’s an STD? Here’s What to Check
Testicle pain from an STD doesn’t always come with classic signs like discharge or burning. That’s the frustrating part. Infections like chlamydia or gonorrhea can travel up the urethra and infect the epididymis, causing pain on one side, swelling, and tenderness. But sometimes the only real clue is discomfort in the testicle itself, especially after sex, masturbation, or prolonged arousal without release.
That’s why it’s worth testing even if you're not seeing “typical” STD symptoms. No fever? No problem. STDs don’t play fair, and they often don’t follow the textbook. You don’t need a full-blown outbreak or lesion to be infected. You just need one unlucky exposure, and a little inflammation goes a long way in that tightly packed area.
If you’ve had unprotected sex, a new partner, or symptoms in the last 2–4 weeks, an at-home combo STD test kit can give you answers fast, discreetly, and without waiting rooms. You deserve to know what’s going on, without shame and without delay.
People are also reading: Still Testing Positive After Treatment? Here’s When to Retest
When You Should Go to the ER (Not Just Urgent Care)
Look, most guys don’t love running to the doctor, much less the ER. But when it comes to testicle pain, waiting can cost you more than comfort. There’s a small window of time to treat certain conditions, especially torsion. The difference between saving your testicle or losing it can be measured in hours, not days.
Here’s when to head to the ER, no questions asked
If your pain started suddenly and is intense (not just annoying), and especially if:
- You feel nauseous or have vomited
- One testicle sits higher or at an odd angle
- The pain woke you up or came during rest
- You’re under 25
That’s not something to "wait and see" on. Torsion is most common in teens and young adults, but it can hit anyone. The only way to rule it out is with an ultrasound, and the only fix is surgery. Even if you’re wrong, you’d rather be safe than sterile.
Urgent care or a regular clinic works better when
- The pain is dull or gradual
- You have urinary symptoms (burning, frequency)
- There’s mild swelling, but no fever
- You suspect an STD or haven’t been tested in a while
In those cases, you’re likely dealing with epididymitis, UTI-related inflammation, or minor trauma. Antibiotics can handle it, but early treatment matters. Infections in the testicles can spread fast and become chronic if you wait too long.
What the Pain Feels Like (and What It Might Be Telling You)
Not all pain feels the same, and that’s a clue in itself. Here’s how some of the most common causes of testicle pain actually feel in the body:
- Twisting, tight, sick-to-your-stomach pain? That’s classic torsion. It feels like a body punch that doesn’t go away and may make you physically ill. Don’t wait, get to the ER.
- A hot, swollen, throbbing ache? Could be epididymitis or orchitis (inflammation of the testicle). Usually linked to an infection, often bacterial or STD-related. Antibiotics work, but only if you start them early.
- Sharp pain during sex or after ejaculation? Could be prostate-related or referred pelvic nerve pain. It might also signal congestion or infection in the reproductive tract. Not urgent, but it’s worth checking out, especially if it keeps happening.
- Dull ache that comes and goes, especially when standing? Possibly a varicocele. Feels like pressure or a dragging sensation. Not dangerous, but annoying, and may affect fertility over time.
- A lump with no pain at all? Don’t ignore it. Testicular cancer often starts as a painless lump. If something feels harder, larger, or different than the other side, get an ultrasound. Fast.
Check Your STD Status in Minutes
Test at Home with Remedium6-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $119.00 $294.00
For all 6 tests
Can You Prevent Testicle Pain?
You can’t prevent everything, torsion, for example, sometimes just happens due to how your anatomy is wired. But you can reduce the risk of infection, strain, and misdiagnosed panic attacks. Here’s how:
- Use protection during sex. Chlamydia and gonorrhea are major causes of testicle infections and are preventable with condoms and testing.
- Don’t delay STI screenings. At-home tests make it easier than ever to know your status discreetly.
- Avoid heavy lifting without proper form. Hernias and muscle strains are sneaky causes of referred pain.
- Stay hydrated and pee after sex. Helps prevent UTIs and bacterial buildup.
- Know your normal. Feeling around during showers helps you catch new lumps or swelling early, before pain kicks in.
The goal isn’t to live in fear, it’s to recognize what’s normal for your body so you can act when something feels off. Pain is your body’s alarm. Listen to it, but don’t panic. Respond with facts, not fear.
FAQs
1. Can an STD really cause pain in just one testicle?
Yup. It’s not always the whole package of symptoms like burning pee or discharge. Sometimes it’s just a dull throb on one side, and that’s it. Gonorrhea or chlamydia can sneak up and inflame the epididymis (a tube behind the testicle) without ever touching your urethra. So yeah, one sore ball can totally mean an infection. Don’t wait for it to get worse.
2. How do I know if it’s torsion or just an infection?
Here’s the cheat code: if the pain hit you like a sucker punch, came out of nowhere, made you nauseous, and hasn’t let up, get to the ER. That’s torsion energy. But if it started slow, feels more like pressure or swelling, and maybe you’re peeing weird too? That’s leaning infection. Still needs attention, just not sirens blaring.
3. I don't see any swelling. Could it still be serious?
Absolutely. Swelling isn’t always the first symptom. Internal inflammation can hurt like hell before you see a thing. Plus, referred pain from your prostate, lower back, or even a hernia can trick your body into feeling it in the testicles. Trust what you feel, not just what you see.
4. Can testicle pain go away on its own?
Sometimes, yeah. If it’s from overexertion, minor strain, or post-sex sensitivity, it might fade with rest and time. But if it lasts longer than a day or two, or gets worse instead of better, it’s time to check in. Waiting it out only works if it’s truly something minor, and guessing wrong is not a flex.
5. Is it embarrassing to get this checked out?
Only if you think saving your testicle is embarrassing. Seriously, providers see this stuff constantly. You’re not the first guy to limp in clutching his groin. Nobody’s judging. They just want to make sure it’s not torsion or something that needs treatment fast.
6. What does epididymitis actually feel like?
Imagine someone pressed a hot stone behind your testicle and left it there. It’s usually a slow burn, achy, tender, and sometimes warm to the touch. Walking might make it worse. Sitting too. It’s uncomfortable, but not “drop to the floor” pain like torsion. Antibiotics usually clear it up fast, but the sooner you start, the better it works.
7. I’m vaccinated, do I still need to worry about STDs causing this?
You might be protected against HPV or hepatitis B, but that doesn’t cover the big bacterial hitters like gonorrhea, chlamydia, or syphilis. Vaccines are amazing, but not a get-out-of-testing-free card. If you're sexually active, especially with new or multiple partners, testing is still part of the deal.
8. Is pain after sex or masturbation normal?
Sometimes. Your body can get a little cranky after a long session, especially if you don’t release, or you go several rounds without recovery. But if it becomes a pattern, or the pain hangs around for days, that’s worth a deeper look. Could be congestion, inflammation, or even a minor tear.
9. Do STDs always come with pain?
Not even close. Most STDs are sneaky, they show up silently and spread quietly. That’s why routine testing matters. Pain is one possible symptom, but absence of pain ≠ absence of infection. Some folks carry chlamydia or gonorrhea for months without a clue.
10. How fast can an STD cause testicle pain after exposure?
It varies. Some people feel symptoms within a few days, others not for weeks. It depends on your body, the infection, and whether it moves upstream into the epididymis. If it does, that’s when pain usually kicks in. But you don’t need to wait for pain to get tested. If exposure happened, your body might already be reacting, even if you don’t feel it yet.
You Know Your Body, Don’t Let Pain Catch You Off Guard
Whether it’s a sharp jab in the middle of the night or a dull throb after a hookup, testicle pain deserves your attention. You don’t need to panic, but you do need to act. The scariest part is the uncertainty. Once you know what you're dealing with, everything gets easier: the plan, the treatment, the peace of mind.
If you suspect an infection, don’t guess, test. Our discreet at-home STD test kits screen for the most common causes of testicle-related infections, including gonorrhea, chlamydia, and more.
Your body speaks. Testicle pain is one way it says, “Hey, pay attention.” You don’t need to figure it all out alone. Get answers, get relief, and get back to living without second-guessing every twinge.
How We Sourced This Article: We pulled insights from urology clinics, STD prevention experts, and real patient experiences to create a guide that’s medically sound and emotionally grounded. Around fifteen reputable sources informed the content; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
1. Urology Care Foundation – Testicular Torsion
2. American Cancer Society – Testicular Cancer
3. Testicle Pain Causes — Mayo Clinic
4. Epididymitis: Diagnosis & Treatment — Mayo Clinic
5. CDC — Epididymitis Treatment Guidelines
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist who works to stop, diagnose, and treat STIs. He combines clinical accuracy with a straightforward, sex-positive attitude and is dedicated to making his work available to more people, both in cities and in rural areas.
Reviewed by: S. Halpern, RPN | Last medically reviewed: October 2025
This article is for informational purposes and does not replace medical advice.










