Quick Answer: Condoms greatly reduce STD risk, but they don’t prevent all infections. Skin-to-skin STDs like herpes and HPV can still spread, even with protection. Testing is the only way to know your status.
“I Never Had Unprotected Sex. So How Did I End Up Positive?”
Ty, 28, thought he’d cracked the code of safe sex. “Condoms every time, no excuses,” he said. “Even for oral, which most people don’t bother with. I was that guy.” But three weeks after a new partner, something didn’t feel right. “I had this weird raw spot, almost like a paper cut. No pain, just… different.” He waited it out. Then came the burning when peeing. Then panic.
“I got tested just to rule it out. I was convinced I was being paranoid. But nope. Herpes.” He stared at the result for hours. “I kept saying, ‘But we used a condom. We were safe.’”
Ty isn’t alone. Research shows that even with 100% condom use, herpes can still spread. One pooled analysis found a 30% lower risk for people who always used condoms compared to those who never did. That’s a reduction, not a shield.
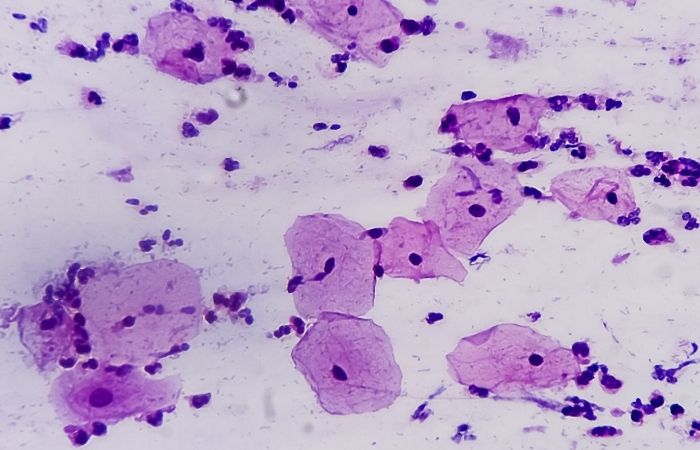
This Isn’t Just a Condom Issue, It’s a Skin-to-Skin Issue
Most people think of STD risk as something that passes through fluids. Semen. Blood. Vaginal secretions. And for infections like HIV, gonorrhea, and chlamydia, that’s true, latex and polyurethane condoms are extremely effective at reducing transmission risk. That’s the tricky part: infections like herpes and HPV don’t need fluids, they just need skin. Even the WHO confirms that condoms can reduce herpes risk, but they can’t fully prevent transmission.
And some infections, like HPV, can be transmitted even when the infected person has no visible symptoms at all. You can’t avoid what you don’t know is there. That’s what makes regular STD testing so essential.
People are also reading: How Soon After Sex Can You Test for STDs?
Symptom-Check Spiral: When Something Feels Off, But You Used Protection
It starts small. A tingle. A dry patch. A single red bump. Maybe it’s razor burn, or maybe it’s something else. You try to logic your way out of it. “It can’t be an STD, we used protection.” You start googling. “Can you get herpes with a condom?” “Itchy after protected sex?” “STD symptoms no discharge?” You click fast, heart racing, stomach tight. You need reassurance, but the answers are muddy. Confusing. Contradictory.
This is where a lot of people stall out. They either talk themselves into believing everything’s fine, or spiral into worst-case scenarios and still don’t test. Neither helps. Because here’s the thing: most STDs don’t have dramatic symptoms. Many have none at all. And those that do? They can look like anything: eczema, ingrown hairs, a yeast infection, a UTI.
If you’ve had any sexual contact, oral, vaginal, anal, or even genital grinding, you could be exposed to something. Especially if you’ve never tested before, or it’s been over a year. Protection helps. But protection doesn’t = certainty.
“I Feel Fine.” Why That’s Not a Reliable STD Strategy
It’s one of the most common reasons people skip testing: no symptoms. No burning, no itching, no bumps, no weird smells. Nothing to panic over. And if you used a condom too? Double safe, right?
Unfortunately, that logic misses one crucial fact: many STDs don’t show symptoms at all. Or when they do, the signs are subtle enough to dismiss, especially if you’re already convinced you’re protected. Chlamydia, for instance, is known as the “silent infection.” Up to 70% of people with it never experience any symptoms. HPV often goes completely undetected unless you get a pap smear or see a visible wart. Even gonorrhea can quietly hang out in the throat, rectum, or urethra with zero signs, until it causes complications like pelvic pain or infertility.
Feeling okay isn’t proof. It’s a placeholder. And testing is the only way to turn that “I think I’m fine” into “I know I’m clear.”
Let’s Talk Oral Sex: The Forgotten STD Risk Zone
There’s a reason oral sex doesn’t feel like “real” sex to a lot of people. No penetration, no pregnancy risk, no mess. But STDs don’t make that distinction. You can get gonorrhea, chlamydia, syphilis, herpes, HPV, and even HIV through oral sex. And many of them hide in the throat or mouth with little to no warning signs.
Condoms during oral are rarely used. Dental dams? Even less. There’s stigma, awkwardness, and sometimes just lack of awareness. That’s where testing becomes essential. It fills the gap left by real-life decisions. Because we all make compromises. We all weigh pleasure, connection, and spontaneity against the “rules.” Testing doesn’t judge you for that, it works with it.
Even if your oral sex was “low risk,” or you were the giver instead of the receiver, exposure is still possible. STDs aren’t just about ejaculation or penetration. They’re about contact, and sometimes, that’s all it takes.
Check Your STD Status in Minutes
Test at Home with Remedium10-in-1 STD Test Kit

 For Women
For Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $189.00 $490.00
For all 10 tests
The Testing Timeline: When and Why It Matters
If you had protected sex but something still feels off, or if it’s just been a while since your last screen, timing matters. Most STDs don’t show up on a test instantly. There’s something called a “window period,” which is how long it takes after exposure for an infection to show up accurately on a test.
Here’s a general guide:
- Chlamydia & Gonorrhea: Accurate within 1–5 days, best after 7
- HIV: Detectable with 4th-gen test in 2–4 weeks
- Syphilis: 3–6 weeks, sometimes longer
- Herpes (blood test): Best after 12–16 weeks
This means if you test too soon, you might get a false negative. It’s also why regular, routine testing is smarter than reactionary panic testing. You don’t need to wait for symptoms or scares. You can build testing into your life, just like STI-savvy people do after breakups, before starting new relationships, or every 3–6 months depending on your activity level.
And yes, you can do it without ever walking into a clinic. At-home test kits now cover multiple infections at once, are discreet, and get results in days. You can test from your bathroom, mail it out, and get peace of mind delivered straight to your inbox.
This combo STD home test kit checks for the most common infections in one go, including those you might still get even with condom use.
Why Testing Is the Most Sex-Positive Thing You Can Do
Let’s reframe the whole conversation. Testing isn’t just about finding out what’s wrong. It’s about confirming what’s right. It’s about making sure your body is aligned with your values: safety, respect, and informed consent.
If you’re queer, poly, kinky, or just sex-curious, regular testing is one of the most affirming things you can do. It says, “I care about the people I touch.” It says, “My body deserves the truth.” It says, “I’m not ashamed to know what’s real.”
So no, using condoms doesn’t mean you never need to test. It means you’re already smart about your health. Testing is just the next step. Not because you did something wrong, but because you deserve real answers, not assumptions.

People are also looking for: The Silent Spreaders: 7 STDs That Lurk in Women’s Bodies for Months
You Deserve Answers, Not Assumptions
It’s easy to cling to the idea that condoms are enough. They’re visible. Tangible. Immediate. Testing feels slower, heavier, scarier. But it doesn’t have to be. Testing is just another form of protection, one that speaks louder than a wrapper ever could.
If you’re feeling that itch of uncertainty, or if something just doesn’t feel right, trust that instinct. Don’t wait for a symptom to scream at you. Don’t rely on memory, hope, or the word “clean.” Give yourself the truth. Quietly, privately, confidently.
Peace of mind is one test away. Take control of your sexual health today, from home, without judgment.
This combo STD test kit checks for the most common infections, whether or not you used protection.
FAQs
1. I used a condom, why would I still need to get tested?
Because condoms don’t block everything. Infections like herpes and HPV live on skin, not just in fluids. So even with perfect use, you could still be exposed. Testing just confirms what the condom can't tell you.
2. Which STDs slip through condoms?
The sneaky ones, herpes, HPV, and sometimes syphilis. Anything that spreads through skin-to-skin contact can sneak past the latex line. Think thighs, vulva, scrotum, pubic area. Condoms help, but they’re not a forcefield.
3. I feel totally fine. No symptoms. So… I’m good, right?
Not necessarily. Most STDs don’t scream, they whisper, or stay silent entirely. Chlamydia, HPV, even gonorrhea can show zero symptoms for months. That’s why so many people pass them without knowing. Feeling fine isn’t a diagnosis.
4. Is oral sex really risky for STDs?
Yep, and it’s often overlooked. You can catch herpes, gonorrhea, chlamydia, syphilis, and even HPV from oral. No, it doesn’t matter if they didn’t finish. No, your mouth doesn’t “filter” infections. That myth needs to die.
5. If the condom didn’t break, am I still at risk?
Maybe. Did the condom cover every area that made contact? Was it put on before any genital rubbing? Was it removed properly? Even small slip-ups (literally) can create openings for skin-to-skin STDs. It’s not just about breaks, it’s about coverage.
6. What if my partner says they tested negative?
That’s great, but timing matters. Did they test recently? Was it a full panel? Do they know about window periods? Many STDs don’t show up immediately. Testing is a snapshot, not a forever pass.
7. Can I get tested too soon?
You can. Every infection has its own “window period”, basically the time it takes to show up accurately. For most bacterial STDs, 1–2 weeks is enough. For herpes and HIV, it can be 4–12 weeks. If you test early, test again later to be sure.
8. Do I have to go to a clinic?
Not anymore. You can pee in a cup or swab at home, drop it in the mail, and get results online. No awkward waiting rooms. No side-eye from the receptionist. Just privacy and peace of mind. Order a home test here.
9. How often should I get tested?
If you’re sexually active with more than one partner, every 3–6 months is a smart rhythm. Monogamous? Test when the relationship starts, and again if anything changes. Rule of thumb: every new partner = new baseline test.
10. Does getting tested mean I’ve been risky?
No. It means you’re responsible. It means you care about your body and your partners. It means you know that protection isn't just physical, it’s proactive. Getting tested is not shameful. It’s hot. It’s grown. Do it for you.
Sources
1. CDC – Genital Herpes – Fact Sheet
4. Genital herpes infection – WHO










