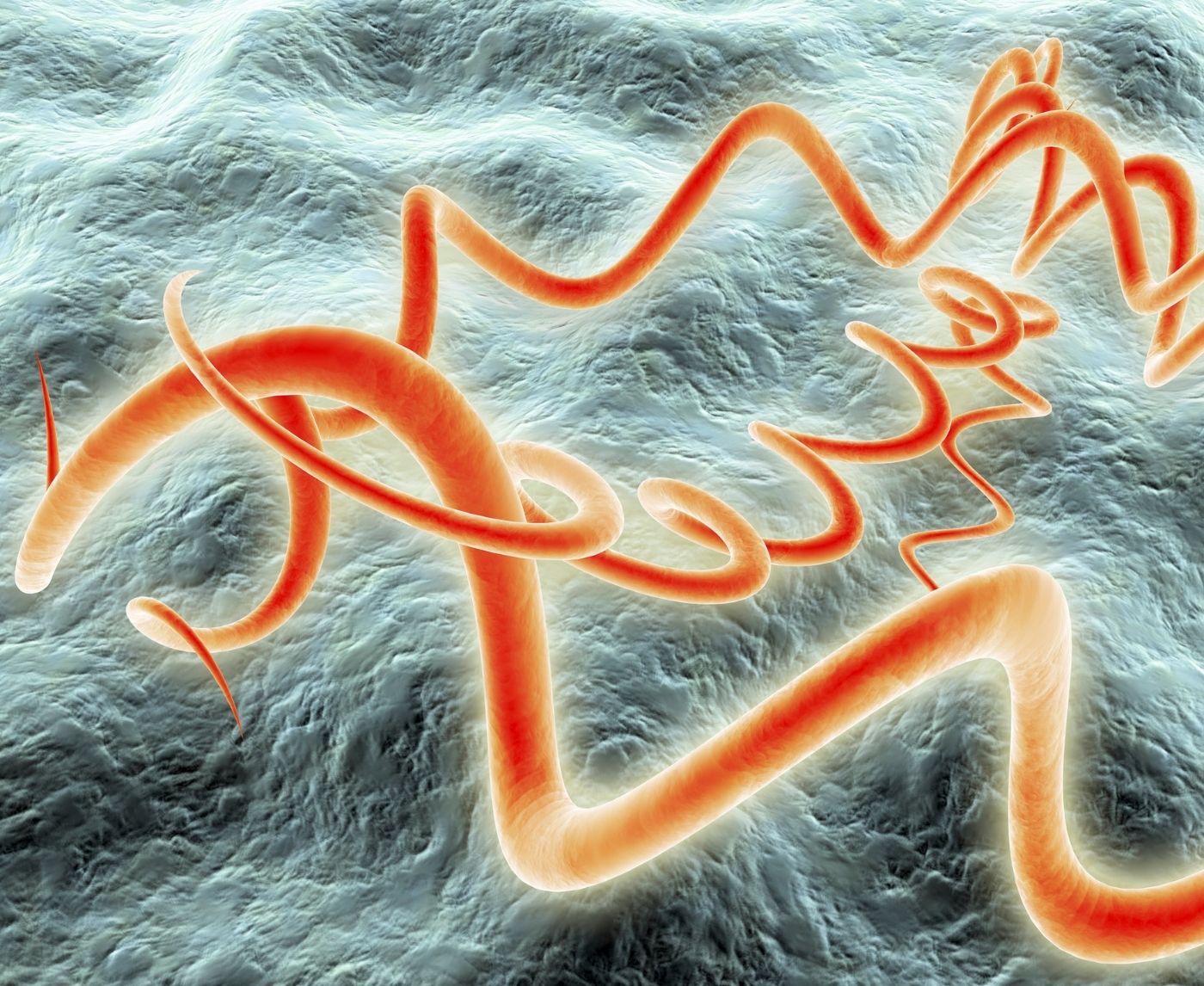
Quick Answer: Syphilis is resurging across all demographics, often spreads silently, and can cause severe complications if untreated. Early testing, even without symptoms, is crucial.
Why This Isn’t Just a Numbers Story
In 2022 alone, over 207,000 new syphilis cases were reported in the U.S., a number that continues climbing in 2025. But the most alarming stat isn’t raw case count. It’s who’s getting missed. The surge includes people who don’t fit the old risk profiles: women in monogamous relationships, queer men using condoms, people who recently tested negative for everything else. It’s showing up in rural towns, college dorms, and maternity wards.
Part of the problem is syphilis’s stealth. Its early symptoms can look like skin irritation, a mosquito bite, or nothing at all. The first stage often includes a painless sore (called a chancre), which can appear on the genitals, mouth, anus, or even inside the vagina or rectum, places people don’t usually examine closely. And when it vanishes in a week or two, people assume they’ve healed. In reality, syphilis is just moving underground.
That’s what happened to Dez, a 34-year-old who thought she had cleared a yeast infection. Weeks later, she developed a rash that wouldn’t go away, but urgent care sent her home with steroids. It took a third appointment, a pushy request for full STD screening, and a callback from her doctor to finally hear the word: syphilis.
Table 1: How Syphilis Hides in Plain Sight
| Stage of Syphilis | What It Can Look Like | Why It Gets Missed |
|---|---|---|
| Primary (3–90 days after exposure) | Painless sore or ulcer (chancre) on genitals, mouth, anus | No pain, heals on its own, often mistaken for ingrown hair or cold sore |
| Secondary (weeks to months later) | Flu-like symptoms, widespread rash (often on palms/soles) | Looks like allergies, viral illness, or eczema; rash is not itchy |
| Latent (no symptoms) | Silent phase with no external signs | Person feels healthy and may not test without suspicion |
| Tertiary (years later, if untreated) | Organ damage, neurological issues, heart problems | Rare today due to treatment, but possible without early detection |
Figure 1. Common stages of syphilis and why they’re so often missed during early screening.

People are also reading: What Does an HIV Rash Look Like? Early Signs and Treatment
The Pregnancy Crisis No One’s Talking About
One of the darkest aspects of syphilis’s comeback is its impact on pregnancies. Congenital syphilis, when the infection passes from mother to fetus, has more than doubled in the past five years. And the outcome isn’t always a dramatic stillbirth or obvious birth defect. Some infants appear healthy, only to later develop bone deformities, blindness, or neurological issues.
The tragedy? This is preventable. Syphilis can be cured with a single penicillin shot during pregnancy, but that only works if it’s diagnosed in time. And with testing gaps in prenatal care, especially for uninsured or low-income mothers, many don’t know they’re positive until it’s too late.
One composite case: Lucía, a 22-year-old who had no prenatal care until her third trimester due to fear of immigration enforcement. She had no visible symptoms. When she finally got tested at 31 weeks, she was positive, and her baby required emergency treatment after birth. Her story isn’t rare anymore.
Check Your STD Status in Minutes
Test at Home with RemediumSyphilis Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $33.99 $49.00
What’s Fueling the Rise?
There’s no single cause behind the resurgence. Instead, it’s a perfect storm of factors:
- COVID-era disruptions led to fewer people getting routine STD checks, and many clinics diverted staff away from sexual health services.
- Dating apps made casual hookups easier, but the public health messaging didn’t keep pace.
- Condoms have seen declining usage among younger populations, particularly when birth control or PrEP are involved.
- There’s a stigma-driven silence around syphilis, often drowned out by louder conversations about HIV or chlamydia.
And let’s not forget testing misconceptions. Many people think they’re being tested for everything when they ask for an STD panel, but most standard panels don’t include syphilis unless you specifically request it.
That’s what caught Jordan, 29, off guard. He’d tested negative twice in one year and thought he was in the clear. But those panels didn’t include syphilis. When a partner tested positive, he realized he’d been positive for months.
We’ll talk more in the next section about how to test smart, and what to watch for even if you feel fine.
How to Know If You Have It (Even Without Symptoms)
Here’s the frustrating truth: by the time most people get diagnosed with syphilis, they’ve already been through weeks or months of confusion. The sore may be gone, the rash may have faded, and there may be nothing left to “see.” But the infection is still active, and still transmissible.
That’s why testing isn’t just for people with obvious signs. If you’ve had unprotected sex, especially oral or anal (where symptoms may be hidden), or if a partner has tested positive for any STD, it’s worth getting checked. Even kissing or sharing toys can pose a risk depending on exposure points.
Dr. Ramirez, an infectious disease specialist in Atlanta, puts it bluntly: “If someone says ‘I feel fine, so I didn’t think I needed to test,’ I remind them syphilis is literally designed to trick your immune system and your brain. You can feel healthy and still be a carrier.”
So how do you test? There are three main routes, each with pros, tradeoffs, and timing nuances. Let’s break them down.
Table 2: Comparing Syphilis Testing Options
| Test Type | Where It's Done | Time to Results | Best Use Case |
|---|---|---|---|
| At-Home Rapid Test | Self-administered (fingerstick blood) | 10–15 minutes | Quick peace of mind, especially if access is hard to get to |
| Mail-In Lab Kit | Sample sent to certified lab | 2–4 business days | Higher sensitivity, good for confirmation or routine screening |
| Clinic-Based Test | Doctor’s office, sexual health clinic | Same-day to 1 week | Ideal if symptoms are present or you want immediate treatment |
Figure 2. Common syphilis testing methods and when each one makes sense based on symptoms, urgency, and access.
Timing Matters: When to Test for Syphilis
Syphilis has one of the trickiest incubation periods of any STD. You might test too early and get a false negative, even if you're already infected. So let’s clarify when to check and when to retest.
If you had a possible exposure within the last few days, it’s tempting to test immediately. But most tests won’t detect the infection that early. You’ll need to wait at least 3–6 weeks for the body to produce detectable antibodies. That’s when accuracy starts to climb.
That said, if you're experiencing symptoms, a sore, swollen lymph nodes, unexplained rash, you should test immediately, regardless of timing. And if you test negative but your symptoms persist, you may need a second test in a few weeks.
Kamil, from the opening story, tested negative at first. But his test was done just nine days after the encounter. It wasn’t until week four, when his rash spread and he tested again, that the syphilis showed up.
If your gut says something's off, or if a partner tests positive, listen to that inner alarm. And remember: it’s better to test twice than regret not testing at all.
Take Control, Discreetly and On Your Terms
If you’re reading this in the middle of a panicked Google spiral, here’s the truth: you don’t have to wait weeks for a clinic appointment or justify your concerns to a judgmental provider. At-home testing puts the power in your hands, literally.
You can order a reliable, finger-prick syphilis rapid test kit from the privacy of your home. It’s fast, accurate within the right window, and ships in discreet packaging. No awkward conversations, no waiting room nerves.
And if you’re worried it’s too late, or that you’ve already infected someone, it’s even more important to know your status now. A single test can answer the questions your brain won’t stop asking. And from there, you can take action.
Explore more at STD Rapid Test Kits to find what fits your needs. Peace of mind is only a few drops of blood away.
Why Retesting Isn’t Just for the Paranoid
Let’s say you already tested and the result came back negative. Relief, right? Maybe. But syphilis can trick even the most accurate tests, if you test during the wrong window or if your immune response is delayed, which can happen due to pregnancy, immune suppression, or certain medications.
Retesting is crucial in three common scenarios:
First, if you tested early (within 3 weeks of exposure) and had no symptoms. In this case, the antibodies may not have reached detectable levels yet. Second, if you’re in an ongoing relationship with a positive partner. A single negative test doesn't mean you're safe forever. And third, if you were treated for syphilis and want to confirm it’s gone.
Ty, a 41-year-old with a new monogamous partner, tested negative while his boyfriend tested positive. It took three rounds of testing over two months before his own results turned positive. “I thought I was being paranoid,” he said. “Turns out I just tested too soon.”
If you’ve recently taken antibiotics for something unrelated, that can also affect your test result, especially if the medication partially treated the infection without curing it. This “masked” syphilis can show up later during a follow-up screen.
Bottom line: the more vulnerable the situation, the more important the retest. Waiting two weeks can feel like forever, but it could be the difference between catching it early or letting it linger for months unnoticed.

People are also reading: Azithromycin or Doxycycline: Which Antibiotic Works Faster for Chlamydia?
How It Spreads When You Least Expect It
One of the most misunderstood aspects of syphilis is how easily, and how subtly, it spreads. Unlike chlamydia or gonorrhea, syphilis doesn’t require ejaculation or even penetrative sex. It can pass through simple skin-to-skin contact with a sore during oral, anal, or vaginal activity. It can even spread via kissing if there's a chancre near the lips or inside the mouth.
This means even people who use condoms correctly every time aren’t 100% protected. Because syphilitic sores can appear on the scrotum, labia, or anus, they often sit outside the coverage zone. And because they’re painless, most people never notice them until long after they’ve disappeared.
That’s why prevention isn’t just about protection, it’s about information. The more you know your body, your partner's history, and your own testing rhythm, the less likely you are to get blindsided.
If your only sexual health strategy is “they looked clean” or “we didn’t do anything risky,” syphilis doesn’t care. It finds the gaps. And with so many people skipping annual STD panels or assuming syphilis isn’t included, those gaps are getting wider.
Check Your STD Status in Minutes
Test at Home with Remedium6-in-1 STD Rapid Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $119.00 $294.00
For all 6 tests
Case Spotlight: The Rash That Wasn’t Allergies
Mia, 33, thought she was reacting to a new body wash. A bumpy rash had spread across her back and arms, then moved down to her palms and soles. Her primary care doctor said it was probably an allergic reaction or viral rash. She was given antihistamines and sent home.
Over the next three weeks, she noticed her fatigue worsen and a dull ache in her joints. When she brought it up again, her provider hesitated, then finally suggested a full STD panel. The bloodwork came back positive for secondary syphilis.
“I felt gross and confused,” she told us. “I thought you had to have open sores or something. I didn’t feel sick enough to be infectious.”
This is exactly how syphilis survives: it mimics benign things and spreads in silence. The scary part isn’t just the disease, it’s how easily it hides in plain sight.
Table 3: Real-Life Scenarios and Testing Advice
| Situation | Should You Test? | Recommended Timing |
|---|---|---|
| You had oral sex with a new partner last weekend | Yes, even if no symptoms | Wait 3–6 weeks, then test |
| You saw a sore that healed quickly, no pain | Yes | Immediately, then retest in 2–4 weeks if negative |
| Your partner tested positive for syphilis | Absolutely | Now, and again in 6 weeks |
| You tested negative but have symptoms | Yes, symptoms override test result | Test now and again after 2–3 weeks |
| You were treated for syphilis recently | Yes, to confirm clearance | 3–6 months post-treatment |
Figure 3. Common real-world encounters and how to time your test for accuracy and peace of mind.
FAQs
1. Can you really get syphilis from oral sex?
Yup. Even if it felt “low-risk,” syphilis doesn’t need penetration to spread. A sore inside the mouth or on the genitals can pass it during oral. We’ve seen cases where people thought they were being safe but didn’t realize that one sore, totally painless, was enough.
2. I thought syphilis was a thing of the past?
You’re not alone. A lot of people assume it vanished with old-timey medicine ads. But nope, syphilis is not only back, it's rising fast. In some states, it's outpacing chlamydia. What’s changed is how quietly it spreads now, and how easy it is to miss.
3. What does syphilis actually look like early on?
Honestly? It often doesn’t look like much. Some people get a small, painless bump or sore that clears up on its own. Others notice a rash, usually on the torso or hands and feet. And plenty of people? Nothing at all. That’s what makes it so sneaky, and why testing is key.
4. How long should I wait to test after a hookup?
If we’re talking syphilis specifically, the sweet spot is 3 to 6 weeks after exposure. That’s when your body has likely made enough antibodies to show up on a test. But if you’ve got symptoms or your partner tested positive? Test now, then again in a few weeks just to be sure.
5. I got tested last month, am I covered?
It depends. First, did your test actually include syphilis? (It’s not always part of standard panels unless you ask.) Second, have you had any new exposures since then? Testing is a snapshot, not a long-term guarantee. If something changed, it might be time to recheck.
6. Are at-home syphilis tests legit?
Yes, as long as you use them during the right window. Most are blood-based and detect antibodies, which means they’re accurate starting around 3 weeks after exposure. They’re super convenient and can be surprisingly empowering, especially if you’re avoiding clinics or just want privacy.
7. Can syphilis come back after treatment?
Not exactly. If you’re treated properly, it’s cured. But you can absolutely catch it again if you’re exposed. We’ve seen people test positive, get treated, and test positive again a year later because their partner hadn’t been treated, or they had a new exposure.
8. Do I have to tell partners if I test positive?
It’s hard. We get it. But yes, ethically and often legally, it’s important to let them know so they can get tested too. You don’t have to do it alone; some health departments offer anonymous partner notification services, or you can use scripts from clinics that take the pressure off.
9. What happens if I’m pregnant and have syphilis?
Then testing and treatment become even more urgent. Syphilis can seriously harm the baby if untreated, think brain, bone, and organ issues. But the good news? If caught early, it’s treatable during pregnancy, and most babies are born totally healthy when care starts in time.
10. Is syphilis dangerous if I ignore it?
Unfortunately, yes. Left untreated, syphilis can eventually affect your brain, nerves, heart, and more, even years after the original infection. That’s why this isn’t just a “take antibiotics and move on” situation. Early testing saves a ton of future pain.
You Deserve Answers, Not Assumptions
Syphilis isn’t a relic of the past, it’s very much a crisis of the present. But unlike past generations, you have tools your grandparents never had: fast testing, real answers, and discreet support. Whether you’re nervous, confused, or just playing it safe, taking the step to test is an act of power, not panic.
Don’t let silence be your symptom. This at-home combo test kit checks for syphilis and other common STDs quickly, privately, and with results in minutes. The sooner you know, the sooner you can stop the spread, starting with yourself.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate.
Sources
1. Planned Parenthood – Syphilis Overview
2. County‑level Syphilis Data | STI Statistics – CDC
3. Resurgence of syphilis, the great imitator – PMC
4. The Resurgence of Syphilis: A Critical Public Health Concern – Glikas et al.
5. Why Is Syphilis Spiking in the U.S.? | Johns Hopkins Bloomberg School of Public Health
6. Upward Trends of Syphilis in the Non‑Pregnant Adults – Frontiers in Public Health
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: Tasha N. Webb, MPH | Last medically reviewed: November 2025
This article is for informational purposes and does not replace medical advice.