Quick Answer: Testing positive for HPV does not mean you have cancer. Follow up with your doctor for the next steps and additional screening specific to the type of HPV you have.
The First 24 Hours: What Not to Do (And What Actually Helps)
Marissa, 27, opened her online results alone in bed. It was 2AM. She’d taken the test “just in case” before starting a new relationship. “I felt like I was infected with something dirty,” she later told her friend, “like I had to warn people off.” That night, she spiraled through cancer forums, STI Reddit threads, and old ex-texts, searching for a source, a scapegoat, or a fix.
If this is where you are, pause. Close the doom tabs. The most important thing to do in the first 24 hours after a positive HPV result is nothing rash. No mass texts to former partners. No rushed treatments. No self-diagnosing stages of cervical cancer from a blog post in 2013. What helps is grounding: write down what the result actually says (e.g., high-risk type vs “abnormal cells” vs wart-causing strain). Breathe. Set a follow-up appointment. You are not contagious in the way media makes you believe, and this doesn’t change your worth, your safety, or your sex life overnight.
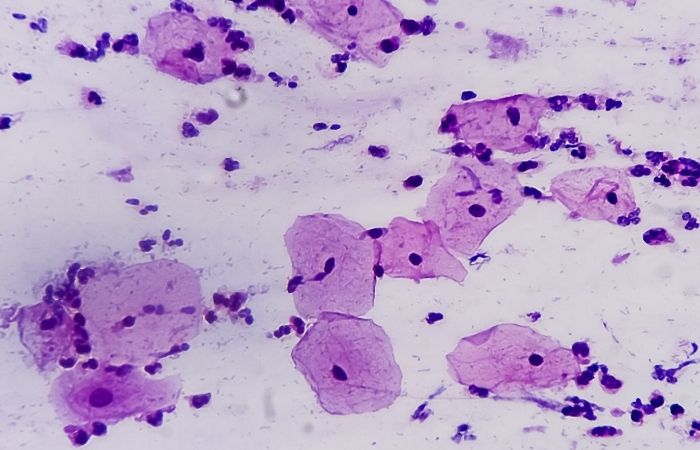
Are You Reading It Right? How to Confirm Your HPV Result
HPV test results can sound more ominous than they are. Most of us aren’t taught how to interpret terms like “ASC-US,” “positive for high-risk strains,” or “inconclusive for DNA.” If you received your results through a clinic portal or at-home testing service, look for a breakdown. Many results indicate the presence of the virus without showing disease. For example, a test may confirm you have a high-risk HPV strain (like type 16 or 18), but your Pap smear may still be normal. That means there's no evidence of abnormal or precancerous cells yet, and that’s a critical difference.
Even if the test was done at home, you can take a screenshot of your result and bring it to a telehealth consult or Planned Parenthood. A provider can help confirm whether your result suggests the need for additional screening like colposcopy or just a wait-and-retest plan. Don’t assume the worst based on a “positive” flag alone.
| Result Phrase | What It Means | Next Steps |
|---|---|---|
| HPV Positive, High-Risk Type Detected | You have a strain linked to cancer risk, but not cancer itself | Follow up with Pap or colposcopy in 6–12 months |
| HPV Positive, Low-Risk Type | Linked to genital warts, not cervical cancer | Usually no treatment unless symptoms appear |
| Abnormal Pap + HPV Positive | Precancerous changes possibly underway | Colposcopy or biopsy recommended |
| HPV Negative | No virus detected | Routine screening schedule applies |
Figure 1. Common phrases in HPV results and what they actually mean. Always confirm specifics with a provider.
Who to Talk To (And Scripts for When You Can’t Find the Words)
It’s not just about your cervix or testicles, it’s about your relationships. An HPV diagnosis often raises the hardest question no one preps you for: who needs to know? If you’re in a new relationship, you might wonder if this changes how they see you. If you’re monogamous, it might stir trust issues. And if you're navigating hook-up culture, it can feel like a stop sign on intimacy.
There is no legal requirement to disclose HPV in most settings, especially since it’s so common. But there are emotional benefits to honest, shame-free communication. One approach is to normalize it as you would with cold sores (also a virus), using language like:
"Hey, I just found out I tested positive for a strain of HPV. It’s super common, and most people clear it without knowing they ever had it. It doesn’t mean I did anything wrong, I just want to be real with you about it."
For long-term partners, clarity helps prevent spirals. Let them know this doesn’t prove infidelity or mean someone cheated. HPV can stay dormant for years. A past partner may have passed it on long before you ever met. If needed, invite them into your follow-up plan instead of just reporting the result. Some couples even test together to feel more in sync. The more you own the narrative, the less power it has to control your dynamic.
People are also reading: The Future of STD Testing: Telemedicine, AI, and At‑Home Kits
Is There Treatment for HPV? Depends on What Shows Up (Or Doesn’t)
This is one of the biggest misconceptions about HPV: that a positive test demands immediate treatment. The reality is that most strains clear naturally, especially in people under 30. Your immune system often clears the virus within two years, and no medication is required. In fact, for most people, there is no direct treatment for the virus itself, only for the conditions it can cause.
Warts caused by low-risk HPV can be removed with topical creams, cryotherapy, or laser removal, but they often return unless the virus clears. Abnormal cells caused by high-risk HPV may require procedures like LEEP or colposcopy-guided biopsy, but only if those changes persist or worsen. Otherwise, most doctors recommend a “watchful waiting” strategy with regular Pap or HPV co-testing to monitor.
| HPV Type | Condition | Typical Treatment | Clears on Its Own? |
|---|---|---|---|
| Low-risk (6, 11) | Genital warts | Topicals, freezing, laser removal | Often, but warts may recur |
| High-risk (16, 18) | Cervical/anal cell changes | Monitoring, biopsy, LEEP | Yes, especially in younger people |
| Other high-risk types | Usually no symptoms | Regular follow-up screening | Yes, immune system often clears it |
Figure 2. Common HPV strains and what treatment, if any, is typically needed. This table focuses on outcomes, not just the presence of the virus.
For many, the “treatment” is lifestyle-based: strengthening immunity with better sleep, managing stress, quitting smoking, and following up on time. That doesn’t mean “heal it with vibes” or blame your immune system for getting infected, it means letting your body do what it’s designed to do with time and support.
Call to Action: Stop Guessing, Start Knowing
Whether your test came from a clinic or at home, what matters most is follow-through. If you haven’t tested your partner(s), now is a good time. If you’re overdue for a Pap or want a second check, it’s easy to do that from home too. You can order a discreet kit and test in private without waiting rooms, judgment, or exposure.
The Combo STD Home Test Kit includes screening options that can help detect multiple infections, including those that may show up with or after HPV. It's FDA-approved and delivers fast, confidential results.
Your body deserves clarity, not confusion. Get the answers that move you forward.
Can You Get Reinfected? How to Prevent a Repeat Diagnosis
Let’s bust a myth right here: you can’t “catch the same HPV twice” from yourself, but you can get a different strain, or pass the same one back and forth with a partner if one of you hasn’t cleared it. Reinfection isn’t about poor hygiene or sleeping around, it’s about biology, immunity, and timing. Once your immune system clears a strain, your body is generally protected against that one. But with over 100 types of HPV, there's always another you might encounter.
Condoms reduce, but don’t eliminate, risk. HPV is spread through skin-to-skin contact, not just fluid exchange. That includes areas not covered by condoms, like the base of the penis, vulva, or inner thighs. Still, using protection consistently can significantly reduce transmission, especially when combined with vaccination.
If you haven’t already, ask your provider about the HPV vaccine. It’s not just for teens. Many adults up to age 45 can still benefit, especially if they’ve only had a few partners or haven't been exposed to all nine strains covered by the current Gardasil vaccine.
| Prevention Strategy | What It Helps Prevent | Who Should Consider It |
|---|---|---|
| Condoms or Dental Dams | Reduces risk of new or ongoing HPV exposure | All sexually active people, regardless of relationship type |
| HPV Vaccination (Gardasil 9) | Protects against 9 major HPV types (high and low risk) | Anyone age 9–45 who hasn’t received full dose series |
| Limiting sexual partners during active clearance | Reduces reinfection and viral load during immune response | People recently diagnosed with high-risk HPV |
| Regular screening and retesting | Detects abnormal changes early, tracks clearance | People with cervixes age 21+, or anyone with recent HPV+ |
Figure 3. Effective prevention strategies after an HPV diagnosis. Clearance doesn’t happen overnight, support your body while protecting your partners.
Order Now $33.99 $49.00 Check Your STD Status in Minutes
Test at Home with Remedium
Papillomavirus (HPV) Test




This Is About More Than a Virus: Navigating Shame, Fear, and Stigma
HPV isn’t just a diagnosis, it’s a detour through some deep emotional terrain. A lot of readers have told us they felt “tainted,” “gross,” or even “unworthy of love” after seeing that result. That response isn’t a failure of logic, it’s the cost of silence around STIs. We don’t talk about how common HPV is, or how casually it’s spread, or how little it says about your choices.
Jorge, 34, described the day he found out: “I was crying in the pharmacy aisle, Googling how to break up with my girlfriend. I assumed it meant I cheated without knowing.” But his doctor explained that the virus can sit dormant for years, sometimes a decade, without symptoms. His girlfriend had tested negative for everything before. It didn’t mean betrayal. It just meant biology.
What helped Jorge was reframing: this wasn’t a punishment, it was a prompt to care more actively for his body and his partner. He got vaccinated, shared a printout of CDC stats with his girlfriend, and they kept going. “She said, ‘It’s skin. It happens.’ I’ll never forget that line.”
If you’re struggling with shame, it helps to hear this clearly: Your diagnosis doesn’t define your worth. It doesn’t diminish your desirability. And you’re not alone, not by a long shot. Up to 80% of sexually active people will get HPV at some point. Most never know it. You just happened to look.
How Long Until HPV Clears? What the Science Shows
One of the most common (and painful) questions after a positive HPV result is: how long is this going to stay in my body? The answer varies, but we know this much: the vast majority of healthy people clear the virus within 6 months to 2 years.
In fact, according to CDC data, about 90% of new HPV infections go away on their own. High-risk types may take longer, and factors like smoking, chronic stress, and immune suppression can prolong persistence. That’s why providers often suggest retesting after 12 months rather than rushing into treatment. They’re not ignoring you, they’re giving your immune system time to do its thing.
If your result came from an at-home test or a rapid cervical swab, you might feel like retesting right away “just to be sure.” But remember: the virus doesn’t disappear in days. Give it space. Wait the full window before checking again. And if new symptoms appear, warts, pain, discharge, then yes, follow up right away.
Return to STD Rapid Test Kits to find discreet, verified tools to check your status from home. Peace of mind is one test away.

People are also reading: It Burns When I Poop After Sex. Is That an STD?
FAQs
1. Can I still have sex if I tested positive for HPV?
Absolutely. HPV doesn’t mean a lifetime of celibacy. Most people who’ve had sex have been exposed to it at some point, whether they knew it or not. If you’re symptom-free (no warts, no active lesions), sex is generally safe, especially with condoms or dental dams. If you’re in a relationship, this is something you work through, not something that ends your sex life.
2. Do I have to tell every single person I’ve ever slept with?
Nope. HPV isn’t tracked the way chlamydia or HIV is. Because it can lie dormant for years, there’s no way to know exactly when or from whom you got it. If you’re currently seeing someone or think a recent partner might be affected, honesty helps, but going on a confessional tour? Not required.
3. Does HPV mean I have cancer, or that I will get it?
No, and no. Testing positive just means you’ve got one of the many strains of the virus. Some are linked to cancer, yes, but even those take years to develop into something dangerous, if they do at all. Regular screenings catch changes early. Most people with high-risk types never develop cancer. Think of it like a warning light, not a crash.
4. What if I feel fine, do I still need to follow up?
Yes, even if you feel 100% fine. Most people with HPV never feel a thing, which is exactly why screening exists. HPV can quietly cause changes to cervical or anal cells over time. That’s why your doctor will likely suggest a Pap, colposcopy, or just a retest in 12 months. No symptoms doesn’t mean no story.
5. Can men get HPV too?
Definitely, and they often don’t know it. While there’s no approved HPV test for men in general use, guys can still carry and pass it on. It can lead to genital warts, penile, anal, or even throat cancers. Men benefit from the vaccine just like women do, and should be part of the prevention conversation, not left out of it.
6. If I already have HPV, is it too late for the vaccine?
Not necessarily. The vaccine protects against multiple strains. Even if you’ve had one, chances are you haven’t had all nine covered by the Gardasil 9 shot. If you’re under 45, talk to your provider. Many people get vaccinated after a diagnosis to prevent future infections.
7. Can stress or my immune system affect whether it goes away?
Yes, your immune system is the real MVP here. Most people clear the virus naturally within two years. But if your immune system is weakened (think: stress, illness, smoking, medications), clearance can take longer. That doesn’t mean you’re doing something wrong, but it’s a good reason to take care of yourself while your body does the heavy lifting.
8. My partner is upset and thinks I cheated. How do I explain this?
HPV doesn’t come with timestamps. It can live in your system for years without symptoms, which means you or your partner could’ve had it long before meeting each other. It’s not a cheating alarm, it’s a common virus. Try saying, “This doesn’t mean someone did something wrong. It means one of us had it from before, and now we know.”
9. Do genital warts mean I have cancer?
Nope. Genital warts are annoying and awkward, but they’re not dangerous. They’re caused by low-risk HPV types (usually 6 and 11), and while they can recur, they don’t lead to cancer. There are treatments to remove them if needed, but many go away on their own.
10. How long will this virus stay in my body?
For most people, HPV clears within 6 months to 2 years. That’s especially true if you’re under 30 and otherwise healthy. Some strains stick around longer, especially the high-risk ones, but even then, it’s not forever. Your immune system is constantly working behind the scenes. The key is not panic, it’s patience, plus smart follow-up.
You’re Not Alone, And You’re Not Broken
Getting that “HPV positive” result can feel like the beginning of a breakup with your body. It isn’t. It’s a turning point, one that millions of people face, and one that many move through with more clarity, confidence, and connection than they thought possible.
If you’re still staring at your phone, your printout, or your partner across the room, wondering what this changes, start here: it doesn’t change you. It changes what you know. And knowing means power. Knowing means protection. Knowing means healing.
Don't wait and wonder; get the clarity you need.This at-home combo test kit quickly and discreetly checks for the most common STDs.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate.
Sources
3. About Genital HPV Infection – CDC
4. HPV Infection – CDC STD Treatment Guidelines
5. Human Papillomavirus and Cancer – WHO
6. Human Papillomavirus – StatPearls / NCBI
7. HPV and Cancer – National Cancer Institute
8. Human Papillomavirus and Associated Cancers: A Review – PMC
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: Alex Nguyen, RN, MSN | Last medically reviewed: October 2025
This article is only for informational purposes and should not be taken as medical advice.