Quick Answer: After sexual assault, testing is recommended at several points: within the first week (baseline), again at 2 weeks, and again at 6–12 weeks depending on the STD. Early testing helps with treatment and documentation, but later tests are often needed for accuracy.
Why This Guide Exists (And Who It’s For)
This isn’t just for survivors of violent rape. It's for anyone who's been touched without permission. Anyone who was too drunk to consent. Anyone who feels off after a night that didn’t end the way they thought it would. It’s for people unsure whether what happened “counts” as assault, and who are still trying to protect their health in the aftermath.
If you’re scared of going to a clinic, if you don’t want your name on a chart, or if you just want to take control from your own home, this guide includes real options. Not every survivor has access to post-assault care. But everyone deserves to know if they’ve been exposed to HIV, chlamydia, gonorrhea, syphilis, or herpes.
This isn’t about proving anything. It’s about protecting yourself. Testing is care, not confession.
People are also reading: Can You Get an STD in a Monogamous Marriage? Yes, Here’s How
What STDs Are You At Risk For After Assault?
Depending on the kind of contact, survivors may be at risk for several infections, even if there are no visible symptoms. The most common STDs after sexual assault include:
| STD | How It Spreads | Can It Show Symptoms? |
|---|---|---|
| Chlamydia | Vaginal, anal, or oral sex | Often silent, but may cause discharge or pain |
| Gonorrhea | Vaginal, anal, or oral sex | May cause burning, discharge, or sore throat |
| Syphilis | Any contact with sores (oral, genital, or anal) | Painless sores may appear then vanish |
| HIV | Blood, semen, vaginal fluids | No early symptoms in many cases |
| Herpes (HSV 1/2) | Skin-to-skin or mucosal contact | Blisters may show up within 2–12 days |
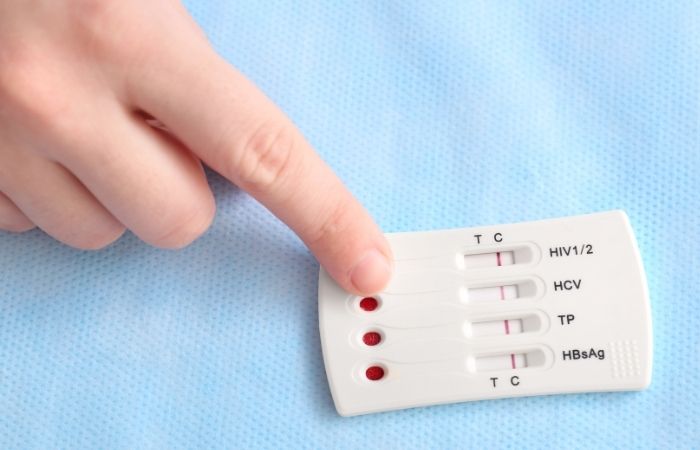
Figure 1. Common STDs to screen for after sexual assault, including transmission routes and symptom likelihood.
If there was penetration (oral, vaginal, or anal) without protection, or if bodily fluids were exchanged, your risk may be higher. But you can still get an STD without full penetration. Skin-to-skin infections like herpes and HPV don’t care whether it was “real sex.” That’s why testing isn’t about judging what happened, it’s about knowing what’s possible.
When Should You Test After Assault?
Timing matters, and it’s okay if you can’t do it all at once. Here’s the typical testing timeline survivors follow. Some tests are useful right away, while others need time for the infection to become detectable.
| STD | Earliest Test Time | Best Time to Test | Should You Retest? |
|---|---|---|---|
| Chlamydia | 5–7 days | 14 days | Yes, if exposed again |
| Gonorrhea | 5–7 days | 14 days | Yes, if symptoms appear |
| Syphilis | 3–6 weeks | 6–12 weeks | Yes, if initial test is negative |
| HIV | 10 days (NAAT) | 4–6 weeks (Ag/Ab combo) | Yes, again at 12 weeks |
| Herpes | 2 weeks (if symptoms) | 4–6 weeks (blood test) | Only if symptoms persist |
Figure 2. Suggested STD testing timeline after sexual assault based on infection type and window period.
If you were seen at a hospital or SANE clinic, they may have done a baseline test and offered HIV prevention (PEP) within 72 hours. If not, it’s still worth testing now. Even if weeks have passed. Even if you feel fine. The body doesn’t always show signs when something’s wrong.
Why Some Tests Come Back Negative (At First)
False negatives aren’t always errors. Sometimes, they just mean the test was taken too soon. Most STDs have what's called a window period, the time between exposure and when the infection can be picked up on a test. If you test during that window, especially in the first few days, you might get a negative result even if you were exposed.
We’ve heard stories like this hundreds of times:
“I got tested five days after it happened. Everything came back clear. Then a month later, I felt off. Retested. Boom, chlamydia.”
That doesn’t mean the first test was wrong. It means your body needed more time to develop a detectable amount of the infection, or for your immune system to start producing antibodies, in the case of HIV or syphilis.
If you’ve already tested early, give yourself credit for taking action. But don’t let a single result close the chapter. Plan a follow-up test at 2–6 weeks depending on the STD. And if something changes, if symptoms show up or exposure continues, test again.
Check Your STD Status in Minutes
Test at Home with Remedium7-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $129.00 $343.00
For all 7 tests
Privacy and Control: What to Expect with At-Home Kits
If you’re worried about someone finding out, you’re not alone. Privacy is the number one reason survivors choose at-home testing over clinics. Here’s what that actually looks like:
Kits arrive in plain envelopes. No brand names. No “STD” on the label. You collect the sample yourself, urine, swab, or fingerprick, then follow the steps in the kit. Some give you results in minutes. Others are mailed to a lab and return your results online, usually in 1–3 days.
The 6-in-1 STD At-Home Rapid Test Kit checks for multiple infections using simple steps you can do at home. You stay in control the whole time. No appointments. No waiting rooms. No judgment.
If you're testing while living with others, consider timing the kit for a weekday delivery. Many survivors choose a locker pickup or alternate shipping location if they share a home or mailbox.
If you’re in a rural area, testing by mail might be your fastest or only option. For many people living off-grid or traveling, these kits are the difference between no care and real answers.
What If the Test Is Positive?
Breathe. Positive does not mean permanent. Almost all STDs are curable. Positive does not define you, your history, or your future. It simply means your body needs some TLC.
What you need to do next depends on what you’ve tested positive for:
- Chlamydia or Gonorrhea: Easily cured with antibiotic medication in pill or injectable form. No lasting damage if caught early.
- Syphilis: Cured with penicillin. Early stages are reversible.
- Herpes: Controllable with antiviral medication such as valacyclovir. No cure, but outbreaks can be minimized or prevented.
- HIV: Life-changing, but no longer life-threatening. Medications are now available that make your viral load undetectable and untransmittable.
If you used a home test kit, you may need to look into a local clinic or online service to get a prescription filled. If you are uncomfortable going into a public clinic, try Googling “confidential STD treatment near me” and see what comes up.
Should You Tell a Partner?
This part is hard. Especially after assault. Especially if you’re not sure what counts as a “partner” in the first place. But if someone else was exposed, before or after the incident, letting them know helps protect them too.
Here’s what you can say:
“I’ve been tested for STDs and something came back positive. You might want to get checked too.”
You don’t owe details. You don’t have to disclose the assault if it’s not safe or healing to do so. Anonymous partner notification tools are available through many clinics and public health departments. Some apps even send anonymous texts or emails with local testing options.
STD Rapid Test Kits offers private testing kits you can send to others. If your partner is scared to go to a clinic, they can test in their own space, on their own terms.

People are also reading: Can You Get an STD from a Tongue Piercing? Here’s the Truth
Retesting: When and Why It’s Still Important
Retesting isn’t paranoia, it’s protocol. Even if your first test was negative, most doctors recommend retesting between 2–12 weeks depending on the infection. This isn’t about punishing you for what happened. It’s about protecting your future health.
Here’s how to think about it:
- After Treatment: Wait 3 to 4 weeks before retesting.
- If Asymptomatic: Test at the end of each window period to detect infections such as HIV or syphilis.
- If Symptoms Appear: Don’t wait. Test as soon as possible, especially if there is discharge, sores, itchy feelings, or fever.
Some survivors choose to retake a test simply because they want to. Maybe the first test was rushed and fuzzy. That’s okay. Reclaiming your body is a process. You don’t have to justify your reasons for wanting to be sure.
You're Not Alone: What Survivors Say About Testing
Sexual assault steals control. Testing can be a way to take some of it back. But it’s not always easy. Many survivors describe the testing process as emotionally triggering, others call it empowering. There’s no one right reaction. Only your right to make the next choice.
“The test didn’t make me feel better right away. But the result gave me something real to hold onto. Something that wasn’t just panic or shame.”
We’ve talked to survivors who couldn’t walk into a clinic, so they tested in their bathroom with the fan running. Others waited months, then woke up one day ready. There’s no deadline. There’s only access, and we’re trying to expand it.
If you need help beyond testing, consider these options:
- RAINN (Rape, Abuse & Incest National Network): 24/7 confidential chat with trained support specialists
- Therapy for survivors: Look for trauma-informed care or LGBTQ+ affirming providers via Psychology Today’s directory
- Local crisis centers: Many offer free STD testing, mental health support, and legal help
You don’t have to face this alone. And you don’t have to do everything at once.
Before You Panic, Here’s What to Do Next
If your brain is swirling with “what ifs,” you’re not the only one. But facts help calm the fear spiral. Most STDs are either curable or manageable. Early detection prevents long-term complications. Testing isn’t about blame, it’s about health.
Even if you don’t feel ready to talk about what happened, you can still get answers from your own space. Testing lets you reclaim something that was taken: your autonomy. You’re in charge of what comes next.
Don’t wait and wonder, get the clarity you deserve. This at-home combo test kit checks for the most common STDs discreetly and quickly.
Check Your STD Status in Minutes
Test at Home with Remedium3-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $69.00 $147.00
For all 3 tests
FAQs
1. Do I really need an STD test if I don’t feel any symptoms?
Yep. That’s the trap, most STDs are sneaky quiet, especially in the first few weeks. You could be carrying chlamydia, gonorrhea, or even HIV and feel totally fine. That’s why we test based on risk, not symptoms. Waiting until something hurts? Too late. Testing is how you catch it early, treat it fast, and move forward on your own terms.
2. How soon after the assault should I test?
If you’re within the first 5–7 days, it’s a good time to do a baseline test for gonorrhea, chlamydia, and HIV (if using a rapid NAAT). Then mark your calendar: 2 weeks for follow-up, 6–12 weeks for longer-window infections like syphilis or late-stage HIV detection. Think of it like checkpoints, each one gets you closer to certainty.
3. I tested negative right away. Am I in the clear?
Not necessarily. Early testing gives you a snapshot, not the full picture. If you test too early, you might miss an infection still incubating. Retesting 2–6 weeks later is like taking off your foggy glasses, you’ll finally see the full view. And if something still feels off? Trust your gut. Test again.
4. What if my test comes back positive and I don’t know who gave it to me?
That happens more than you think. A positive result doesn’t mean you’re dirty. It means your body met a bacteria or virus, and now it needs backup. If you don’t know who exposed you, or if the exposure was nonconsensual, your priority is treatment and healing, not detective work. You can still get care, meds, and support without having all the answers.
5. Do I have to go to a clinic, or is at-home testing enough?
You absolutely do not have to drag yourself to a fluorescent-lit clinic if that’s not your vibe right now. At-home kits like this combo test cover multiple infections and give you space, privacy, and control. That said, if you get a positive or have symptoms, a follow-up with a provider is smart, especially for prescription treatment or confirmatory testing.
6. Can I test in secret? Like, will anyone find out?
Yes, you can test in total privacy. No “STD” labels on the box, no surprise calls to your house, no emails that scream “EXPOSED!” at the top. You get your kit in a plain envelope, and your results come straight to you. No one else sees them unless you decide to share. Your body, your info, your choice.
7. Should I tell my partner, even if it wasn’t their fault?
If you're in a sexual relationship, giving them a heads-up is the compassionate move. But that doesn’t mean reliving the trauma or oversharing. You can keep it simple: “I got tested after a situation and something came back positive. You might want to get checked too.” Period. If they care about you, they’ll get it. If not, well… consider that data.
8. I’m scared the test will trigger me. Is that normal?
Completely. For many survivors, testing brings everything back. The smell of alcohol wipes, touching yourself for a swab, it can feel like a flashback. That’s why doing it at home can be safer for your nervous system. Light a candle. Wear cozy clothes. Set a timer. You don’t need to be brave. You just need to be kind to yourself while you get it done.
9. What if the assault happened a long time ago, should I still test?
Yes, especially if you never got tested afterward. Some infections stick around for months, or years, without obvious symptoms. We’ve had folks discover an old syphilis infection years later, or test positive for herpes from a partner they haven’t seen since college. If it’s been haunting your brain, get peace of mind. It’s never “too late” to take care of your health.
10. Do at-home STD kits even work?
When used correctly and at the right time? Hell yes. Today’s rapid kits are lab-backed and FDA-cleared, with high accuracy for the big players like chlamydia, gonorrhea, and HIV. Just follow the instructions, collect carefully, and don’t rush the read window. If you’re unsure, snap a pic and compare it to examples, or retest in a week. We trust science. And you can trust your gut too.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted six of the most relevant and reader-friendly sources. Every external link in this article was checked to ensure it leads to a reputable destination and opens in a new tab, so you can verify claims without losing your place.
Sources
1. Sexual Assault and STIs – STI Treatment Guidelines (CDC)
2. Getting Tested for STIs (CDC)
3. Get Tested | STI & HIV Testing and Vaccines (CDC National Prevention Information Network)
4. Sexual Assault Infectious Disease Prophylaxis – StatPearls (NCBI)
5. Sexual Assault – ACOG Clinical Guidance (American College of Obstetricians and Gynecologists)
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: Sierra Kay, MPH | Last medically reviewed: February 2026
This article is for informational purposes and does not replace medical advice.










