Quick Answer: STD symptoms vs no symptoms both require testing based on exposure risk, not just how you feel. Many infections like chlamydia, gonorrhea, and even early HIV can be silent, so the right test depends on timing, partner history, and type of contact, not visible signs alone.
When Your Body Is Loud: What Symptoms Actually Tell You
Sometimes your body does not whisper. It shouts. A sharp burn when you pee. A discharge that wasn’t there last week. A sore that looks like nothing you’ve ever seen before. In those moments, the anxiety feels justified because there is something concrete to point to. You can say, “This changed.”
But symptoms don’t come with labels. Burning can mean gonorrhea, or it can mean a urinary tract infection. A rash could be syphilis, or razor irritation, or a reaction to a new soap. A sore could be herpes, or it could be friction. The body gives clues. It does not give diagnoses.
I once spoke to a college sophomore, we’ll call him Marcus, who noticed a mild sting when urinating after a weekend hookup. “It wasn’t that bad,” he told me. “I almost convinced myself it was dehydration.” Three days later, the discomfort was worse. He tested. It was chlamydia. Treatable. Common. Fixable. But invisible until it wasn’t.
Symptoms narrow possibilities, but they don’t eliminate others. That’s why testing panels are often broader than what your single symptom suggests.
| Symptom | Possible STDs | What It Doesn’t Rule Out | Testing Approach |
|---|---|---|---|
| Burning during urination | Chlamydia, Gonorrhea, sometimes Trichomoniasis | Silent infections in throat or rectum | Urine NAAT test; consider multi-site swab if oral/anal exposure |
| Genital sores | Herpes (HSV-1/2), Syphilis | Early HIV symptoms, other bacterial infections | Swab of sore + blood test for syphilis and HIV |
| Unusual discharge | Chlamydia, Gonorrhea, Trichomoniasis | Asymptomatic HIV or syphilis | Urine or vaginal swab; consider combo panel |
| Rash on palms/soles | Syphilis | Earlier stages of other STDs | Blood antibody test |
| Flu-like illness after exposure | Early HIV | Common viral infections | HIV antigen/antibody test based on window period |
Notice something important. Even when symptoms appear, testing often includes infections that do not obviously match the visible problem. That’s because co-infections are common. If you test for one thing, you may need to test for others.
When Your Body Is Quiet: The Truth About Silent Infections
Now let’s talk about the harder situation. The one where you feel completely fine.
No itching. No discharge. No fever. No sores. You shower. You look. You check. Nothing seems off. And yet, your brain keeps circling back to that night.
Here’s the part that catches people off guard: a large percentage of chlamydia and gonorrhea infections cause no noticeable symptoms at all, especially in women but also in men. Early HIV may feel like a mild flu, or nothing. Syphilis can hide between stages. Trichomoniasis frequently stays quiet in men.
Silence is not safety. It’s just absence of signals.
I once counseled a woman in her late twenties who came in only because her new partner suggested they both test before becoming exclusive. She had zero symptoms. “I almost didn’t go,” she admitted. Her result showed asymptomatic gonorrhea. She would never have known without screening.
Asymptomatic infections matter because untreated STDs can still cause complications and can still be transmitted to partners. Testing without symptoms is not paranoia. It is preventive care.
| STD | How Often Asymptomatic | Potential Risk If Untreated | Recommended Screening Test |
|---|---|---|---|
| Chlamydia | Very common, especially in women | Pelvic inflammatory disease, infertility | Urine or swab NAAT |
| Gonorrhea | Common in women; can be mild in men | Reproductive complications, spread to bloodstream | Urine or swab NAAT |
| HIV | Often mild or unnoticed initially | Immune system damage over time | Antigen/antibody blood test |
| Syphilis | May have painless sore or none noticed | Neurological and cardiovascular damage | Blood antibody test |
| Trichomoniasis | Frequently silent in men | Increased HIV transmission risk | Urine or swab NAAT |
If you’re sitting there thinking, “But I feel normal,” understand this: normal is not diagnostic. Testing decisions are based on exposure and timing more than sensation.

People are also reading: This STD Can Steal Your Fertility Without a Warning Sign
The 2 A.M. Question: Which Test Should You Actually Order?
This is where things get practical.
If you had vaginal, anal, or oral sex with a new partner and you don’t know their recent test status, a comprehensive panel is usually smarter than testing for just one infection. That means screening for chlamydia, gonorrhea, syphilis, and HIV at minimum. Depending on your situation, you may add trichomoniasis or hepatitis screening.
If your partner texted you saying they tested positive for something specific, you test for that infection, and often for others. Because transmission overlaps. Because co-infection exists. Because guessing is unreliable.
If you have clear symptoms, you still often test broadly. The symptom guides urgency, not exclusivity.
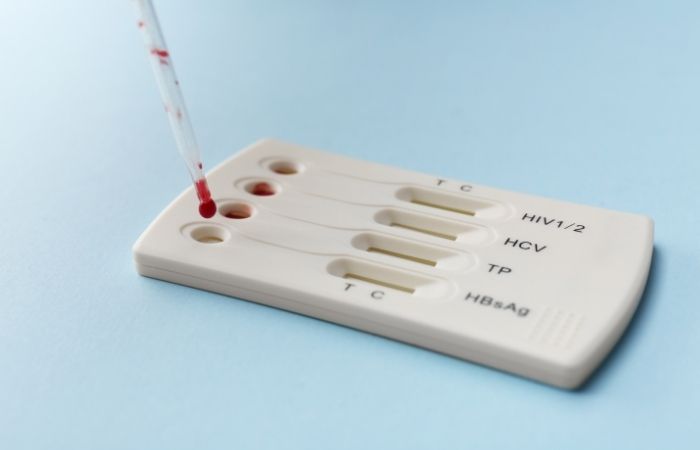
This is where at-home options become powerful. A discreet at-home STD test kit allows you to screen privately without sitting in a waiting room replaying your life choices. For many people, that privacy is the difference between testing and delaying.
If you want broad coverage, a combo panel that checks multiple infections at once often makes the most sense. It answers more than one question. It reduces the risk of false reassurance. And it lets you move forward with clarity instead of suspicion.
Timing Changes Everything: Symptoms Don’t Equal Detection
Here’s something that frustrates people: you can have symptoms and still test too early. Or have no symptoms and still test positive later.
There’s a difference between incubation period and window period. Incubation is when symptoms appear. Window period is when a test can reliably detect infection. They are not always the same.
Imagine someone who develops mild irritation four days after exposure. They test on day five. Negative. Relief. But the window period for accurate detection of chlamydia is typically around one to two weeks. That early negative might simply be too soon.
Testing at the right time matters more than how you feel. In the next section, we’ll break down timing scenarios so you can match your exposure to the right test window.
For now, if you’re unsure, choosing a reliable Combo STD Home Test Kit can provide broad initial screening, especially if you’re within or beyond the typical two-week mark after exposure.
Exposure, Timing, and the Window That Actually Matters
Let’s slow this down and get concrete. Because most panic spirals don’t come from symptoms. They come from uncertainty. You’re not just wondering what you might have. You’re wondering when it would even show up.
A window period is the time between exposure and when a test can reliably detect infection. That’s different from when symptoms start. Some infections show symptoms late. Some never do. Some show symptoms early but aren’t detectable yet. This mismatch is where false reassurance lives.
I’ve seen it happen. Someone tests five days after unprotected sex. Negative. They breathe again. Two weeks later, they retest, positive for chlamydia. Nothing changed except timing.
| STD | Earliest Likely Detection | Optimal Testing Window | Notes |
|---|---|---|---|
| Chlamydia | 5–7 days | 14 days after exposure | Often asymptomatic; urine or swab NAAT |
| Gonorrhea | 5–7 days | 14 days after exposure | Can infect throat and rectum without symptoms |
| Syphilis | 3 weeks | 6 weeks after exposure | Blood test; early sore may go unnoticed |
| HIV | 10–14 days (RNA) | 18–45 days (Ag/Ab test) | Early flu-like symptoms are inconsistent |
| Trichomoniasis | 7 days | 2–4 weeks | Commonly silent in men |
If it’s been less than a week since exposure, you may be testing for baseline information rather than definitive results. That doesn’t make testing wrong. It just means you may need a follow-up test at the optimal window.
If it’s been two weeks or more, most bacterial STDs can be detected reliably. If it’s been six weeks or more, blood-based infections like syphilis are more confidently ruled out.
Check Your STD Status in Minutes
Test at Home with Remedium7-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $129.00 $343.00
For all 7 tests
No Symptoms, But Your Partner Tested Positive
This scenario hits differently.
Your phone lights up. “Hey, I tested positive for gonorrhea. You should get checked.”
Your stomach drops. You feel completely fine. You replay the encounter in your head. You start scanning your body for signs that weren’t there five minutes ago.
If a partner tests positive, you test, even without symptoms. Period.
Transmission does not require visible signs. You can carry and spread chlamydia or gonorrhea without feeling anything at all. Early HIV may feel like nothing more than fatigue, if anything.
In this situation, targeted testing for the known infection is essential. But comprehensive testing is often wise, especially if the partner had not been tested in a while. Overlapping exposures are common, and people rarely carry only one question.
This is where a broad panel like a Combo STD Home Test Kit becomes practical. Instead of testing in fragments, you screen comprehensively and move forward with certainty.
The “I Feel Fine” Trap
Let me say something gently but clearly: feeling fine is not a medical clearance.
Many people equate absence of symptoms with absence of infection. It makes sense psychologically. We trust what we can see. But STDs do not follow our need for obviousness.
I once worked with a couple who both felt completely healthy. They were about to stop using condoms. They decided to test “just in case.” One partner tested positive for asymptomatic chlamydia. Neither had any idea. No discharge. No pain. No fever. Just a lab result quietly changing the trajectory of their health.
Testing when you feel fine is not dramatic. It’s mature. It protects your body and your future partners. It protects fertility. It protects peace of mind.
Symptoms That Mislead People the Most
There are certain physical sensations that send people spiraling, and others that falsely calm them.
A mild itch after shaving can feel catastrophic. Meanwhile, a completely silent throat infection after oral sex can go unnoticed for months. A painless sore from early syphilis can disappear on its own, convincing someone it was nothing. That disappearance does not mean the infection is gone.
Burning during urination is often blamed on dehydration. Mild pelvic discomfort is blamed on stress. Fatigue is blamed on work. We rationalize because we want relief.
But testing is simpler than guessing.
If you’ve had unprotected vaginal, anal, or oral sex in the last three months and haven’t tested, screening makes sense, even without symptoms. If you’ve had multiple partners, screening makes sense. If a condom broke, screening makes sense.
You do not need dramatic symptoms to justify care.
Rapid Test vs Lab Test: Does It Matter?
It depends on what you need.
Rapid at-home tests offer speed and privacy. You collect the sample yourself. You get results quickly. For many people, that accessibility is everything. The difference between acting and procrastinating.
Mail-in lab tests offer high sensitivity and often broader panels. They require mailing a sample and waiting for processing, but they can feel reassuringly comprehensive.
Clinic visits offer in-person evaluation, which is especially important if symptoms are severe or persistent. If you have intense pain, fever, testicular swelling, or unusual discharge with systemic symptoms, clinical care is essential.
But for screening after exposure, especially when symptoms are mild or absent, at-home options from STD Rapid Test Kits provide discreet, practical solutions that reduce delay.
Delay is what increases risk. Not testing method choice.
People are also reading: Used a Condom? You’re Still at Risk for These STDs
Retesting: The Step Most People Skip
Let’s say you test negative at two weeks. Good. But what if exposure was ongoing? What if you were within the early part of a window period? What if you were treated for something?
Retesting is not paranoia. It’s protocol.
After treatment for chlamydia or gonorrhea, retesting is often recommended after about three months to ensure reinfection hasn’t occurred. Not because treatment failed, but because partners may not have been treated or new exposures happen.
If you tested very early after exposure, repeating the test at the optimal window period increases reliability. That second test often brings the closure the first one couldn’t.
Think of testing as a process, not a single event.
The Emotional Side No One Talks About
There’s a moment after you click “order” on a test kit where the panic shifts. It becomes action instead of anxiety.
I’ve heard people describe it as reclaiming control. One man told me, “I realized I was more scared of not knowing than of the result.” That sentence stays with me.
Whether you have symptoms or not, the real weight is uncertainty. Testing replaces imagination with information.
And information is power.
The Exposure Map: Matching Your Experience to the Right Test
Not all exposure is equal. And not all testing should look the same.
A single episode of unprotected vaginal sex carries different risk considerations than oral sex. Receptive anal sex carries different considerations than insertive. A long-term monogamous relationship with no prior testing history carries a different profile than a one-time hookup with someone whose status is unknown.
This is where people either over-test randomly or under-test dangerously. The smarter move is strategic testing.
Picture this. You had oral sex with someone new. No intercourse. No ejaculation in your mouth. You feel fine. You assume the risk is low. But oral transmission of gonorrhea and chlamydia is real, and throat infections are frequently asymptomatic. A urine-only test would miss that. A throat swab matters in that scenario.
Now imagine a condom broke during vaginal sex. No symptoms. It has been three weeks. In that case, urine NAAT testing for chlamydia and gonorrhea, along with blood testing for HIV and syphilis, is appropriate.
The type of contact shapes the type of test.
| Exposure Type | Primary Testing Focus | Sample Type | Timing Guidance |
|---|---|---|---|
| Unprotected vaginal sex | Chlamydia, Gonorrhea, HIV, Syphilis | Urine + blood | 2 weeks for bacterial; 4–6 weeks for blood-based |
| Receptive anal sex | Chlamydia, Gonorrhea, HIV, Syphilis | Rectal swab + blood | 2 weeks initial; retest at 6 weeks if early |
| Oral sex (received) | Gonorrhea, Chlamydia | Throat swab | 2 weeks optimal |
| Partner tested positive | Known infection + full panel | Based on infection | Test immediately; retest at window peak |
| Multiple partners in 3 months | Comprehensive panel | Urine + blood ± swabs | Every 3 months if ongoing risk |
If you are unsure which exposure category you fall into, err on the side of comprehensive testing. It is better to rule out multiple infections at once than to chase one result at a time.
If You Test Positive: The Moment After the Result
Let’s talk about the screen lighting up with a positive result.
Your heart speeds up. You reread it. You wonder if you misinterpreted the line. You think about who to tell. You think about what it means.
Take a breath.
Most bacterial STDs, including chlamydia and gonorrhea, are treatable with antibiotics. Syphilis is treatable, especially when caught early. HIV is manageable with modern medication that allows people to live long, healthy lives and reduce transmission risk dramatically.
A positive test is information. It is not a verdict on your character.
The next steps are straightforward. Confirm the result if required. Begin treatment promptly. Inform partners so they can test and treat. Avoid sexual contact until medically cleared.
This is where knowledge replaces fear. And fear often shrinks quickly once you have a plan.
Check Your STD Status in Minutes
Test at Home with Remedium6-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $119.00 $294.00
For all 6 tests
Prevention Is Not About Shame, It’s About Strategy
Testing is not a confession. It is a maintenance habit.
Condoms lower the risk, but they don't completely get rid of it, especially for infections that spread through skin-to-skin contact, like herpes and syphilis. Sexual health clinics often do routine screenings every three to six months for people who are sexually active and have new or multiple partners.
If you are in a new relationship, testing together before becoming exclusive can build trust rather than suspicion. It reframes the narrative from accusation to collaboration.
I’ve seen couples turn testing into a shared health ritual rather than a reactive panic. That shift changes everything.
The Decision Framework: Symptoms vs No Symptoms
Let’s simplify everything we’ve covered into a mental framework you can actually use.
If you have symptoms, test broadly and test promptly. Do not self-diagnose. Symptoms narrow possibilities but do not eliminate others.
If you have no symptoms but recent exposure, test based on window period timing. Two weeks covers most bacterial infections. Six weeks strengthens blood-based screening confidence.
If your partner tested positive, test regardless of how you feel.
If you are sexually active with new or multiple partners, routine screening every three months keeps surprises small.
Testing is not about panic. It is about clarity.
FAQs
1. “I feel totally fine. Be honest, do I really need to test?”
I’m going to give you the answer you already suspect. Yes. A lot of chlamydia and gonorrhea infections are completely silent. Early HIV can feel like a minor cold or absolutely nothing. Feeling fine is not the same thing as being cleared. Testing isn’t dramatic. It’s maintenance.
2. “But there’s no discharge. Doesn’t that mean I’m okay?”
Discharge gets all the press, but it’s not the only sign, and it’s often absent. I’ve seen people with textbook-positive results who swore nothing had changed. No smell. No fluid. No irritation. Your body doesn’t always wave a red flag. Sometimes it just shrugs.
3. “I had oral sex only. Is that even risky?”
Yes, but in a specific way. Oral exposure can transmit gonorrhea and chlamydia, and throat infections are notoriously quiet. That means no soreness, no visible signs, just bacteria minding their business. If that was your exposure, a throat swab matters more than you think.
4. “My partner tested positive, but I have zero symptoms. Am I probably negative?”
I wish it worked that way. Transmission doesn’t require symptoms. You can carry an infection and feel completely normal. If your partner tested positive, your job isn’t to guess, it’s to confirm. That’s power, not panic.
5. “How soon is too soon to test?”
If it’s been three days, you’re probably testing for reassurance, not accuracy. Most bacterial STDs show up reliably around the two-week mark. Blood-based infections like syphilis may take longer. Testing early isn’t wrong, it just may require a repeat test. Think of it as step one, not the finale.
6. “If symptoms disappear, does that mean I’m in the clear?”
Unfortunately, no. Some early syphilis sores are painless and vanish on their own. That doesn’t mean the infection is gone. Disappearing symptoms can be the calm before the untreated storm. Testing settles the question.
7. “Are at-home STD tests actually reliable, or am I kidding myself?”
Quality at-home tests, used correctly and at the right time, are reliable screening tools. The bigger issue isn’t accuracy, it’s timing. A perfect test taken too early can still give you the wrong reassurance. Match the test to the window period, and you’re using it wisely.
8. “If I test negative once, am I done?”
Maybe. Maybe not. If you tested within the optimal window period and haven’t had new exposure, that negative result carries weight. But if you tested early, or if exposure continued, a follow-up test gives you closure instead of a question mark.
9. “Is it weird to test every three months if I have multiple partners?”
It’s not weird. It’s responsible. Many sexually active adults with new or multiple partners use quarterly screening as their baseline. It keeps small problems small. It also makes conversations with partners easier because you’re coming from a place of routine, not suspicion.
10. “Why does this feel so scary even if it’s common?”
Because STDs carry stigma that doesn’t match medical reality. These infections are common. They are human. They are part of sexual ecosystems, not moral judgments. The fear usually shrinks the moment you replace guessing with information. That’s the shift.
You Deserve Clarity, Not Guesswork
The real difference between STD symptoms and no symptoms is not danger level. It is visibility.
Your body may speak loudly. Or it may stay quiet. Either way, testing is how you listen clearly.
If you're ready to trade in your anxiety for answers, look into STD Rapid Test Kits' private screening options. Taking action moves you from guessing to knowing, whether you choose a targeted test or a full panel.
And knowing is powerful.
How We Sourced This Article: This guide integrates current screening recommendations from leading public health authorities including the CDC and peer-reviewed infectious disease research. We reviewed clinical data on asymptomatic infection rates, window periods, and diagnostic accuracy to ensure timing guidance reflects current standards of care. Our goal was to translate that evidence into practical, emotionally accessible guidance without stigma.
Sources
1. CDC Sexually Transmitted Infections Treatment Guidelines
5. WHO Sexually Transmitted Infections Fact Sheet
6. PubMed Clinical Research Database
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access to confidential screening options.
Reviewed by: A. Martinez, PA-C | Last medically reviewed: February 2026
This article is meant to give you information, not to give you medical advice.










