Quick Answer: Babies can get STDs from their mothers during pregnancy, labor, or delivery, even if the mother has no symptoms. Common infections like herpes, syphilis, chlamydia, gonorrhea, and HIV can be passed silently without proper testing and timing.
Why This Still Happens in 2025
It’s easy to assume that modern medicine has this figured out. That every pregnant person gets a full STD panel. That anything dangerous gets caught. But the truth is messier. Not all clinics screen for every infection. Some infections hide in the nervous system or lie dormant until stress or hormonal shifts trigger a flare. Many people don’t know they’re carrying something, and some infections, like herpes simplex virus, are still routinely missed in prenatal bloodwork.
STDs passed from mother to child are known as vertical transmission or perinatal transmission. It can happen during pregnancy (through the placenta), during labor (through contact with infected fluids), or after birth (through breastfeeding or close contact). Most of these transmissions happen not because of neglect, but because the infection went undetected. And that’s what makes this issue so emotionally complicated.
What STDs Are Most Likely to Be Passed to Babies?
Different infections behave in different ways. Some travel through the bloodstream. Others live in genital tissues and emerge during labor. Some, like HIV, can be managed almost completely with medication, while others, like herpes, may not be treated unless symptoms appear. Understanding how each infection transmits to a newborn is key to preventing long-term harm.
Here’s a breakdown of the most common STDs that can be passed from mother to child, when transmission typically occurs, and what risks they carry for the baby:
| Infection | Transmission Timing | Primary Risk to Baby | Treatment Available |
|---|---|---|---|
| Herpes (HSV) | During delivery (contact with lesions or shedding) | Seizures, blindness, brain damage, death | Yes – antivirals for mother and baby |
| Chlamydia | During delivery | Eye infections, pneumonia in newborn | Yes – antibiotics |
| Gonorrhea | During delivery | Severe eye damage, joint infections | Yes – antibiotics |
| Syphilis | During pregnancy (crosses placenta) | Stillbirth, brain damage, organ failure | Yes – penicillin (highly effective if caught) |
| HIV | Pregnancy, delivery, breastfeeding | Lifetime infection, immune dysfunction | Yes – antiretroviral therapy (ART) |
| Trichomoniasis | During delivery (rare) | Low birth weight, premature delivery | Yes – metronidazole |
| Hepatitis B | Pregnancy, delivery, post-birth contact | Chronic liver infection, cancer risk | Yes – immunoglobulin + vaccine at birth |
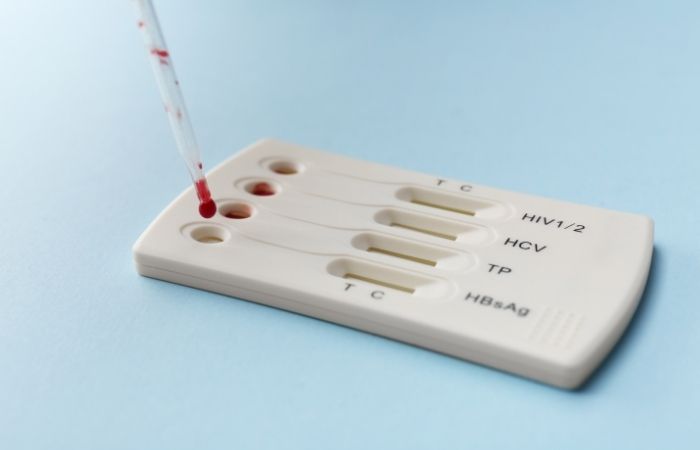
Figure 1. Common maternal STDs and their impact on newborns. Transmission timing varies by infection, which is why both prenatal and delivery-time testing matters.

People are also reading: Blinded by Syphilis: The STD That’s Silently Attacking Eyes
Case Study: “I Thought I Was Clean. I Wasn’t.”
Leila, 28, had been with the same partner for three years. She had her first child with no complications. When she became pregnant again, she skipped some of the optional testing, not out of recklessness, but because she assumed she was safe. At 37 weeks, her midwife noted a small bump near her vulva. It didn’t hurt. It didn’t itch. They swabbed it just in case.
Three days later, the results came back: HSV-2 positive. She had never had a cold sore or a genital outbreak in her life. Her OB scheduled a C-section to prevent vaginal delivery exposure, and her baby was born healthy, but it shook her to her core. “If that bump hadn’t been there,” she said, “I never would have known. And I could’ve passed it to him without a clue.”
Her story isn’t rare. Most maternal-to-child STD transmissions come from asymptomatic infections, and they don’t always present in obvious ways. Skin shedding, vaginal secretions, and even oral contact post-delivery can all contribute to infection if the parent isn’t diagnosed.
Check Your STD Status in Minutes
Test at Home with Remedium8-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $149.00 $392.00
For all 8 tests
Why Some Infections Go Undetected During Pregnancy
Prenatal care in most developed countries includes a basic STD screen, but that doesn’t mean it’s comprehensive. The routine panel typically covers HIV, syphilis, hepatitis B, and sometimes chlamydia and gonorrhea. But tests for herpes, HPV, and trichomoniasis are not always standard unless there are symptoms. And many tests only flag active infections, not past exposure or dormant viral shedding.
The gap becomes even more dangerous when infections reactivate during pregnancy, especially under stress or immune system shifts. For example, a mother might contract herpes years before pregnancy and never show symptoms, only for a silent flare-up near delivery to put her baby at risk. This is why testing once isn’t always enough.
Even when a provider orders a test, timing matters. Some infections take time to appear in the bloodstream or genital tract. If a test is done too early, or too late, it may miss the window for detection. That’s where follow-up screening and clinical judgment come in.
When is the risk of transmission highest during pregnancy?
Transmission risks change as pregnancy progresses. Some infections are more likely to cross the placenta during the first or second trimester. Others only become a threat during vaginal delivery. The following table breaks down the typical transmission risks by trimester and infection type:
| Infection | 1st Trimester | 2nd Trimester | 3rd Trimester | Labor/Delivery |
|---|---|---|---|---|
| Syphilis | High | High | High | Low (usually already transmitted) |
| HIV | Medium | High | High | High (if not on ART) |
| Herpes | Low | Low | Moderate | Very high if active lesions or shedding |
| Chlamydia | Low | Low | Low | High |
| Gonorrhea | Low | Low | Low | High |
| Trichomoniasis | Very low | Low | Moderate | Moderate |
Figure 2. Relative risk of STD transmission by trimester and delivery. Some infections (like syphilis) pass early through the placenta, while others (like herpes) become dangerous only during vaginal birth.
Delivery Decisions: When a C-Section Might Be Safer
In some cases, vaginal delivery puts the baby at much higher risk of infection. This is especially true with active genital herpes or untreated HIV. For these situations, OB-GYNs may recommend a scheduled Cesarean section to avoid contact with infected tissues during birth.
But a C-section isn’t a guaranteed shield, it’s a medical strategy, not a cure. If a parent is already shedding virus internally, or if an infection has already crossed the placenta, the delivery method may not prevent transmission. This makes early detection and treatment before labor the most effective protection, not just a surgical workaround.
Kim, 33, had never tested positive for herpes. But at 38 weeks, she noticed tingling and a slight burning sensation that she assumed was irritation. Her OB took a swab and gave her antivirals while awaiting results. The test confirmed HSV-1. She delivered via C-section two days later. Her baby stayed in the NICU for 48 hours for precautionary monitoring but remained uninfected. “I almost brushed it off,” she said. “I’m so glad I didn’t.”
Testing Isn’t Shameful, It’s Protective
There’s a brutal double standard in how people talk about STDs and pregnancy. On one hand, expecting parents are told to protect their baby at all costs. On the other, many are shamed, dismissed, or overlooked if they ask for expanded STD testing or disclose a past infection. This stigma silences conversations that could literally save a baby’s life.
Testing during pregnancy is not an accusation, it’s an act of protection. It allows time for treatment. It opens options for safe delivery. And most of all, it empowers pregnant individuals to make decisions based on facts, not assumptions. For most infections, early treatment makes an enormous difference in preventing congenital or perinatal disease.
If you’re pregnant or planning to be, and unsure what infections you’ve been tested for, ask. Ask your provider directly: “Have I been screened for herpes, trichomoniasis, and HPV?” Don’t assume they have. Many well-meaning doctors follow outdated panels or insurance constraints. Your clarity could protect your child.
STD Rapid Test Kits offers discreet, lab-grade options that can supplement or confirm clinic testing. If you’re somewhere rural or feel dismissed by providers, an at-home option might be your safest next step.
How Testing Works (And What’s Often Missed)
Most people assume that prenatal testing is a one-and-done process. You pee in a cup, get a few vials of blood drawn, and move on. But the type of test matters, and so does the window of time. Infections like chlamydia and gonorrhea require swabs or urine tests, not blood. Others, like herpes, might never show up unless there’s a specific IgG/IgM antibody test ordered, and even then, it won’t detect shedding, just past exposure.
There’s also the issue of retesting. Some infections can be picked up after the initial prenatal screen, especially if there are multiple partners or a recent exposure. For example, a pregnant person may test negative for HIV in the first trimester but convert during the third, especially in high-risk communities. Without retesting, that infection could be missed entirely until symptoms show up in the baby. By then, the damage may already be done.
Here’s a general breakdown of what’s included in standard prenatal screening, and what you might need to specifically request or supplement with at-home testing:
| Infection | Typically Included in Prenatal Panel? | Recommended Retesting? | Additional Notes |
|---|---|---|---|
| HIV | Yes | Yes – each trimester in high-risk areas | Detectable by blood test; can reduce baby risk to <1% |
| Syphilis | Yes | Sometimes | High stillbirth risk if missed; early treatment critical |
| Hepatitis B | Yes | Rarely | Vaccination and newborn immunoglobulin prevent transmission |
| Chlamydia | Sometimes | Yes – especially under 25 or multiple partners | Requires urine or cervical swab, not blood |
| Gonorrhea | Sometimes | Yes | Often tested alongside chlamydia; treatment is simple |
| Herpes (HSV-1/2) | No | Not routinely offered | Blood test can show past exposure; swabs needed during outbreak |
| Trichomoniasis | No | Rarely offered | Common in underserved areas; linked to low birth weight |
Figure 3. Prenatal STD testing gaps. Even with regular care, some infections may not be screened for without direct request or supplemental at-home kits.
People are also reading: Syphilis vs Herpes: How to Tell Them Apart Without Guessing
What Happens If Your Baby Gets an STD at Birth?
This is the part no one wants to imagine, but many new parents have faced. A newborn infected during delivery or in utero might not show symptoms right away. Some signs take days or even weeks to appear. Red eyes, breathing problems, jaundice, poor feeding, irritability, all can be mistaken for generic newborn issues. But in some cases, they’re early signs of a deeper issue.
In the worst-case scenarios, untreated infections can lead to blindness, brain swelling, liver failure, or even death. In the U.S., congenital syphilis rates have been climbing dramatically in recent years, leading to devastating outcomes that are entirely preventable with prenatal detection and treatment. Neonatal herpes remains rare but deadly when it happens, especially in first-time infections not caught before labor.
Still, there’s hope. Most infections passed from mother to baby can be treated effectively if caught early. Newborns may receive antibiotics, antivirals, or immunoglobulin therapy. Some may need NICU support. But the earlier the diagnosis, the better the outcome. That’s why testing before symptoms arise is so critical.
Check Your STD Status in Minutes
Test at Home with Remedium7-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $129.00 $343.00
For all 7 tests
How to Talk to Your Provider (Or When to Go Around Them)
Too many pregnant people assume their doctor has “already taken care of it.” But if something feels off, if you’re worried about a past partner, a recent exposure, or a symptom you’re afraid to name, you have every right to bring it up. Say the words out loud. Ask for expanded testing. If you get brushed off or told it's unnecessary, you’re allowed to seek a second opinion, or test on your own.
STD Rapid Test Kits offers discreet options for Combo STD test kits that can screen for multiple infections at once. You collect the sample privately at home. If you get a positive result, you can follow up with a provider for confirmation and treatment. If negative, you gain peace of mind. Either way, you’re reclaiming agency.
Your baby deserves to come into this world protected, not because you were perfect, but because you were informed. Testing is never a failure. It’s love in action.
FAQs
1. Can babies actually get STDs from their moms?
Yes , and it happens more often than people think. A baby can be exposed during pregnancy, during vaginal delivery, or even from skin-to-skin contact after birth. This includes infections like herpes, HIV, syphilis, and others. You don’t have to be “sick” or showing symptoms for it to happen , that’s what makes this so scary and so important to talk about.
2. But what if I’ve never had symptoms? Doesn’t that mean I’m fine?
Not always. Some STDs , especially herpes and trichomoniasis , can live in your body for years without flaring up. You could be shedding virus without knowing it. One mom described it as “the infection I didn’t even know I had until my baby got eye drops in the NICU.” Silence doesn’t equal safety, especially when it comes to birth.
3. What’s the riskiest infection to pass to a newborn?
It depends, but congenital syphilis is rising fast in the U.S. and can lead to devastating outcomes like stillbirth or neurological damage. Neonatal herpes can also be deadly, especially if it’s a new infection during pregnancy. The good news? Early testing and treatment stop almost all of this before it starts.
4. Will a C-section protect my baby if I test positive?
It might , but only in certain cases. If you have active genital herpes lesions close to your due date, a scheduled C-section is usually recommended. But it’s not a catch-all fix. If an infection like syphilis already crossed the placenta, the delivery method won’t change much. Timing and treatment matter more than surgery alone.
5. Why didn’t my provider test me for everything?
Sadly, “everything” isn’t routine. Most OBs screen for HIV, syphilis, and hepatitis B. Some might include chlamydia and gonorrhea. But herpes? Not unless you ask. Trichomoniasis? Almost never. This isn’t your fault. The system assumes too much and informs too little. That’s why it’s smart to double-check or test from home if you’re unsure.
6. How would I know if my baby got something during birth?
Some signs show up fast, others take time. Think red or swollen eyes, skin rashes, fever, feeding issues, or breathing trouble. One parent said, “I thought she just had colic. Then she stopped eating.” If your gut says something’s wrong , especially in the first month , get checked. Even a mild symptom can be a clue.
7. Is it still safe to breastfeed if I have an STD?
In most cases, yes. But there are exceptions. If you have herpes lesions on your breast, you’ll need to avoid nursing on that side. If you’re living with HIV, U.S. guidelines typically recommend formula to avoid risk, even if you're on meds. When in doubt, ask a provider who actually knows your diagnosis and won’t shame you for asking.
8. Should I test more than once during pregnancy?
If you’re at higher risk , new partners, untreated infections, or community outbreaks , then yes, retesting is a good idea, especially in the third trimester. Think of it as checking your blind spots. One test in the first trimester doesn’t catch a new exposure in week 30. Your baby deserves the clearest picture, and so do you.
9. What if I already had sex again after my first test?
You’re not alone , and yes, you can get exposed again. If you’ve had a new partner, or your partner has, since your initial test, consider retesting. STDs don’t freeze in place just because you’re pregnant. And honestly, there’s no shame in staying informed , only power.
10. Can I really trust an at-home test while pregnant?
If it’s FDA-approved and follows proper collection steps, absolutely. STD Rapid Test Kits are used by people who want answers privately, quickly, and without feeling judged. It’s not a replacement for a doctor, but it’s a solid step , especially if your clinic access is limited or you’ve been brushed off.
You Deserve Answers, Not Assumptions
No one talks about how lonely it feels to second-guess your body while growing a human. To worry that a past hookup or a forgotten test could ripple into someone else’s life. But shame doesn’t prevent transmission. Information does.
If you’re reading this because you’re scared, unsure, or just trying to be thorough, good. That instinct is protective. Whether you’re 5 weeks along or 2 months postpartum, it’s never too late to get tested or retested. And it’s never wrong to want clarity before something becomes a crisis.
Don’t wait and wonder, get the clarity you deserve. This at-home combo test kit checks for the most common STDs discreetly and quickly.
How We Sourced This Article: We used the most up-to-date advice from top medical groups, peer-reviewed research, and reports from people who have lived through the issues to make this guide useful, kind, and correct.
Sources
1. CDC: STD Treatment During Pregnancy
3. Congenital syphilis - Mother-to-child transmission of syphilis (WHO)
4. CDC Reports Latest National Data on Syphilis in Newborns and STIs
5. Preventing Perinatal Transmission of HIV During Pregnancy and Childbirth (NIH)
6. About STIs and Pregnancy (CDC)
7. Screening and Testing for HIV, Viral Hepatitis, STD & Pregnancy (CDC)
8. Pregnant Women: STI Treatment Guidelines (CDC)
9. Chlamydial Infections - STI Treatment Guidelines (CDC)
10. Sexually Transmitted Infections, Pregnancy, and Breastfeeding (U.S. Office on Women’s Health)
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: Janelle Ortiz, RN, MPH | Last medically reviewed: December 2025
This article is for informational purposes and does not replace medical advice.










