Quick Answer: COVID closures delayed STD testing worldwide, but options like at-home test kits, telehealth visits, and pharmacy-based screenings can bridge the gap until in-person services are available.
The Pandemic’s Hidden Impact on Sexual Health
When lockdowns began in early 2020, sexual health services were among the first to scale back. Routine screenings stopped. Walk-in clinics closed. Appointment wait times ballooned from days to months. According to the CDC, STD testing dropped sharply during the pandemic’s first year, while infection rates kept climbing.
This meant more people unknowingly carried and spread infections like chlamydia, gonorrhea, and syphilis. By the time testing returned to pre-pandemic levels, many were facing late-stage complications that could have been avoided.

People are also reading: Caught It From a Kiss? Debunking Hepatitis B Myths
Why Delays Matter More Than You Think
Some STDs can cause permanent damage if left untreated, even for a few months. Untreated chlamydia and gonorrhea can lead to pelvic inflammatory disease in women and infertility in all genders. Late-stage syphilis can damage the heart, brain, and nervous system. HIV can progress without treatment, weakening the immune system.
In my case, waiting eight months meant my infection had time to spread and require a longer, more intensive course of antibiotics. The takeaway? Even if clinics are closed, finding an alternative test is worth it.
Finding a Way: Testing Alternatives When Clinics Are Closed
Just because the local clinic shut its doors doesn’t mean you have to wait months for answers. During the pandemic, a few key options helped me, and thousands of others, get tested without stepping into a waiting room.
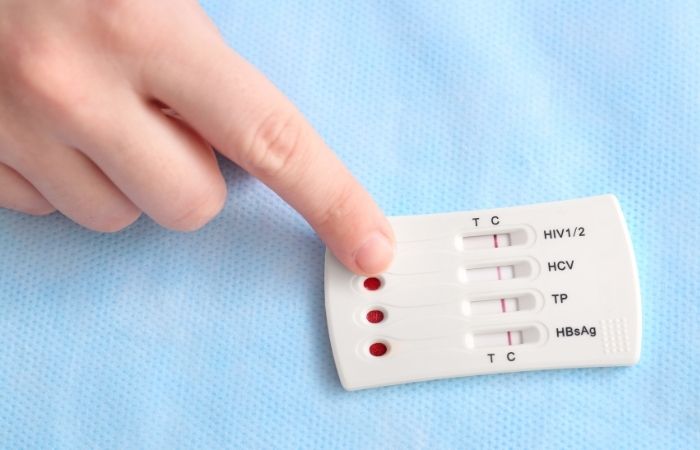
- At-Home STD Test Kits: Order online from reputable providers like STD Rapid Test Kits. Most use a simple finger-prick or urine sample, with results in minutes or days depending on the type.
- Telehealth Consultations: Video appointments are now available at many sexual health clinics. You don't have to leave your house to describe symptoms, get prescriptions, or get mailed test kits.
- Pharmacy-Based Screenings: Even when traditional clinics are closed, some pharmacies provide walk-in or appointment-based testing for common sexually transmitted diseases.
- Pop-Up Testing Events: Pay attention to announcements about community health. During COVID, many cities had mobile testing vans, and some still do.
These solutions aren’t perfect, some infections still require in-person confirmation, but they can bridge the gap until a full clinic visit is possible.
Check Your STD Status in Minutes
Test at Home with RemediumHIV Rapid Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $33.99 $49.00
What I Wish I’d Done Sooner
Looking back, I realize I could have saved months of worry by ordering a home test in week two instead of month eight. Fear and “I’ll wait it out” thinking are dangerous when it comes to sexual health. If you suspect an infection, act. You don’t need perfect circumstances, just a plan.
What Takes Place When You Wait Too Long
In addition to being stressful, STD testing has the potential to alter your health trajectory. Untreated sexually transmitted diseases (STDs) can result in long-term complications that are much more difficult to treat, even though some infections may initially only cause mild symptoms.
- Infertility in both sexes, epididymitis in men, and pelvic inflammatory disease (PID) in women can result from Chlamydia and Gonorrhea.
- Syphilis can harm the heart, brain, and nerves as it advances to secondary and tertiary stages.
- HIV: Without treatment, HIV can advance to AIDS, severely compromising immunity.
- Trichomoniasis: May increase the risk of contracting other STDs, including HIV.
Some of these complications are permanent. That’s why even during a crisis like COVID, finding a workaround for testing is critical.
People are also reading: Why That Rash Won’t Go Away, And Might Be Syphilis
Symptoms You Shouldn’t Ignore
Even if you think you can wait, certain symptoms mean you should seek testing immediately, either through an at-home kit or any urgent-care option available:
- Unusual discharge from the penis, vagina, or anus
- Burning sensation during urination
- Sores, ulcers, or bumps in the genital area
- Pelvic or lower abdominal pain
- Unexplained rash (especially on palms or soles)
- Flu-like symptoms combined with genital changes
Even mild or disappearing symptoms can indicate an infection. Some STDs, like chlamydia, may have no obvious signs at all, which is why routine testing matters even when you feel fine.
Telehealth: The Underrated Lifeline
One of the biggest shifts during COVID was the surge in telehealth appointments. For sexual health, this meant you could speak directly with a provider from your phone or laptop, discuss symptoms, and even have prescriptions sent to your pharmacy, all without leaving your home.
Many clinics expanded services to include mailing self-collection kits for chlamydia, gonorrhea, HIV, and other common infections. While not every condition can be diagnosed remotely, telehealth fills a critical gap when in-person visits are limited or impossible.
How to Build a “Plan B” for Your Sexual Health
If the pandemic taught us anything, it’s that waiting for perfect circumstances is risky. A personal backup plan ensures you’re never left without testing options again. Consider:
- Keeping an at-home test kit on hand for urgent situations
- Knowing your local telehealth providers that offer STD consultations
- Finding pharmacies that provide screening services or can order discreet tests
- Tracking community health pop-ups for free or low-cost testing
With these in place, even unexpected disruptions won’t derail your sexual health.
Check Your STD Status in Minutes
Test at Home with Remedium3-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $69.00 $147.00
For all 3 tests
Financial Help for STD Testing
Cost can be a barrier, especially if you’ve lost income during a crisis. Luckily, there are options:
- Free clinics: Many Planned Parenthood locations and local health departments offer free or sliding-scale STD testing.
- Insurance coverage: Most health insurance plans cover STD screening, sometimes even at-home kits.
- Community grants: Some nonprofits fund free test kits for people in high-risk groups.
Don’t assume you can’t afford testing, ask providers about available programs before paying full price.
Turning a Delayed Diagnosis Into Action
While my own eight-month delay was frustrating, it changed how I think about sexual health. I no longer wait for symptoms to get “bad enough” or assume clinics will always be open. Now, I test regularly, keep a kit at home, and have telehealth providers saved in my contacts.
You can do the same. Whether it’s COVID or another disruption, having tools ready means you can take control of your sexual health without losing months to uncertainty.
Why COVID Hit Sexual Health Services So Hard
When the pandemic began, health systems worldwide had to redirect resources toward COVID-19 testing, treatment, and vaccination. Non-urgent services, like routine STD screening, were deprioritized. Staff were reassigned, clinic hours were slashed, and some locations closed completely.
Even when clinics remained open, fear of exposure kept many people away. The result? A sharp drop in testing volume, coupled with an invisible rise in undetected infections. This perfect storm meant more people unknowingly carried and transmitted STDs for months, or even years, without knowing.
People are also reading: When a Sore Throat Is More Than Just Strep
How Home Testing Changed the Game
One silver lining from the pandemic was the acceleration of home-based health care. At-home STD testing went from niche to mainstream in just months. Providers improved accuracy, streamlined delivery, and expanded coverage for multiple infections in a single kit.
Now, a discreet package can arrive at your door with everything needed to collect a sample. Some kits give results within 20 minutes, while others use a mail-in process for lab-grade analysis. Providers increased coverage for multiple infections in a single kit, expedited delivery, and enhanced accuracy.
Finding Trustworthy Online Information on Sexual Health
Misinformation spreads as fast as infections during emergencies. Myths about sexually transmitted diseases and unreliable "home remedies" proliferated on social media during COVID. Taking action based on false information may result in harm or delay in care.
To keep yourself safe:
- Only trustworthy medical sources, such as the WHO, CDC, or well-known clinics, should be used.
- Advice without references or scientific support should be avoided.
- Verify information from at least two reliable sources.
The foundation of trustworthy care is trustworthy information.
Check Your STD Status in Minutes
Test at Home with Remedium7-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $129.00 $343.00
For all 7 tests
Developing a Sexual Health Routine That Is Resilient
Another pandemic, natural disaster, or local emergency could cause disruptions in healthcare. You can adjust swiftly without losing months to uncertainty if you follow a robust sexual health regimen.
Important actions consist of:
- Frequent testing: If you engage in sexual activity with several partners, get tested every three to six months, even if you feel fine.
- Vaccination: Make sure you are up to date on vaccines against HPV and hepatitis B, two preventable sexually transmitted diseases.
- Free exchange of ideas: Discuss symptoms, safer sex practices, and recent testing with partners.
- Backup points of access: Recognize which telehealth services, pharmacies, and urgent care facilities you can rely on in an emergency.
No matter what happens in the world, you can safeguard your health by being prepared.
FAQs
1. Can COVID postpone testing for sexually transmitted diseases?
Indeed. During the pandemic, many clinics closed or shortened their hours, making it more difficult to get in-person testing.
2. Can an at-home kit provide me with reliable STD results?
Yes, provided that you use a kit from a reliable supplier that has received FDA or CE clearance. Consult a healthcare professional for follow-up positives.
3. Which sexually transmitted diseases are testable at home?
The most popular at-home test options are for trichomoniasis, HIV, syphilis, gonorrhea, and chlamydia.
4. What happens if, while I wait for a test, my symptoms worsen?
Make use of urgent care or telehealth services. Additionally, some pharmacies provide same-day testing.
5. Are STD services provided by telehealth safe?
Yes, pick trustworthy providers or clinics and make sure they abide by privacy and data protection regulations.
6. How soon after the onset of symptoms should I get tested?
Delays raise the risk of complications and transmission as soon as possible.
7. Can I receive care without being tested?
In some urgent situations, doctors may treat based solely on symptoms, but testing helps determine the exact infection and the best course of action.
8. Is it safe to use mail-in STD tests?
Yes, provided that you adhere to the guidelines.
9. Will home STD testing be covered by insurance?
Check with your provider; many plans do. They are provided for free by certain public health initiatives.
10. What’s the best backup plan for sexual health?
Keep an at-home kit, know your telehealth options, and locate nearby pharmacy or mobile testing services.
Taking Charge, Regardless of the Situation
Although COVID altered our perspective on access to healthcare, your dedication to your sexual health need not be altered. Whether or not there is a pandemic, delays occur. It's important to have backup plans so you don't have to wait months for a response you urgently need.
You are entitled to treatment, clarity, and mental tranquility. The resources are available, whether via a nearby clinic, telehealth, or an at-home combo test. The sooner you take action, the sooner you make progress.
Sources
1. COVID-19 Reduced STI Testing and Increased Positivity: U.S. Retrospective Study (2021)
3. WHO – Sexually Transmitted Infections Fact Sheet
4. JAMA – Declines in STD Testing During the COVID-19 Pandemic










