Quick Answer: STD tests during pregnancy are often limited to HIV, syphilis, and sometimes chlamydia/gonorrhea. But these aren’t always retested later, so additional screening (including at-home kits) may be needed to stay safe throughout pregnancy.
Why Syphilis Is Back, and How Pregnancy Hides It
Syphilis isn’t supposed to be a 21st-century problem. But it is. And if you’re pregnant, it’s more than a historical footnote, it’s a silent risk to both you and your baby. According to the JAMA Pediatrics report, congenital syphilis cases have skyrocketed over 250% since 2017, often because of missed opportunities to diagnose or retest during pregnancy.
Here’s what makes it dangerous: syphilis can appear as nothing. No rash. No sores. No fever. Or maybe just one small bump on your vulva that gets written off as a skin tag or shaving irritation. In early pregnancy, many people assume their symptoms, like nausea, mild spotting, or fatigue, are just the usual hormonal chaos. And sometimes, they are. But sometimes, they’re not.
One mother, who posted anonymously on a parenting board, wrote: “I only got tested in the first trimester. They said it was negative. Then my partner told me he had an ‘incident’ at a bachelor party. I didn’t know I could get tested again.”
This isn’t rare. In fact, CDC guidelines only require one syphilis test during early pregnancy unless you’re in a “high-risk” group. But what counts as high risk? It varies by provider, insurance, and state. This ambiguity has left too many women, especially Black, Indigenous, and Latinx mothers, without timely care.
Here’s what the data shows: according to the Sexually Transmitted Diseases journal, nearly 30% of congenital syphilis cases happen in people who had at least one prenatal visit. The test just wasn’t repeated. Or the infection happened afterward. Or the follow-up fell through. This is not about negligence. This is about a system that assumes too much and checks too little.

People are also reading: Pain in the Testicles: Causes, Symptoms, and Prevention You Shouldn’t Ignore
The Symptoms You Might Be Googling (Or Ignoring)
So how do you tell if it's an STD, or just pregnancy being pregnancy? The truth is, you often can’t tell on your own. But some clues matter, especially if you know what to watch for.
With syphilis, the first stage might bring a small, painless sore, often internal, unnoticed, or misdiagnosed. It might show up on your cervix, vulva, anus, or even lips if oral sex was involved. Some people also notice swollen lymph nodes or a faint rash, often on the hands or feet.
With chlamydia, it’s even sneakier. Up to 70% of pregnant people won’t feel a thing. When symptoms do show up, they mimic early pregnancy problems: abnormal discharge, light bleeding, pelvic discomfort. Chlamydia can lead to premature birth or eye infections in newborns if untreated.
HIV is usually detected through early testing, but not always. Some people acquire it during pregnancy, through a cheating partner, needle exposure, or reactivation of a prior undiagnosed infection. Symptoms of early HIV might include fevers, night sweats, sore throat, or flu-like fatigue. But again, how do you tell that apart from “normal” pregnancy exhaustion?
“I thought I was just rundown from morning sickness,” said Marisol, 33, who tested positive for HIV during her second pregnancy. “But something felt off. I had sores in my mouth that weren’t going away. That’s what made me ask for more tests.”
The truth? Pregnancy masks STD symptoms. That’s why testing matters so much, even when nothing “seems wrong.” Especially then.
What Prenatal Testing Covers, and What It Leaves Out
By the time Keisha reached 34 weeks, she’d had two ultrasounds, a glucose screen, and a birth plan on file. But when she asked if she should get tested again for STDs, just in case, her OB shook their head. “We already did that back in your first appointment,” they said.
But Keisha had a new partner since then. They’d used protection inconsistently. And she’d had an unusual vaginal discharge that no one had explained. At her insistence, they reran the tests. The chlamydia came back positive.
Here’s what people don’t always realize: most providers only test once, if at all. According to CDC guidelines, all pregnant people should be tested early in pregnancy for HIV, syphilis, and hepatitis B. But that’s just the start:
Chlamydia and gonorrhea testing is recommended only for people under 25 or those deemed at risk. Herpes? Rarely tested unless there are visible lesions or a known history. HPV and trichomoniasis? Almost never included. And if you test negative once, many providers won’t retest unless something drastic changes.
It’s an outdated model based on cost, not care. And it assumes that your partner is monogamous, honest, and healthy, which isn't always the case. A recent study in The Lancet found that 44% of pregnant individuals with an STD had no symptoms and did not meet “high-risk” criteria under current screening guidelines.
Worse, many people think they've been “fully tested” when in reality, their provider only screened for HIV and syphilis during the first visit. No full panel. No recheck. No disclosure. The assumption? That you’d ask if you needed more. But who knows what to ask when you’re already overwhelmed by fetal development apps, prenatal vitamins, and endless blood draws?
Check Your STD Status in Minutes
Test at Home with Remedium3-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $69.00 $147.00
For all 3 tests
Myth: “If My Doctor Didn’t Mention It, It Must Not Be Important”
One of the most dangerous myths about reproductive health is that being quiet means being safe. Your doctor may not talk about herpes, chlamydia, or the chance of getting them again while you're pregnant, but that doesn't mean you're fine. That usually just means the system didn't mark you as "at risk."
"I wish I had known I needed to ask," wrote one Reddit user after finding out she had given her newborn syphilis without knowing it. "They made me feel like I had done something wrong by asking for more tests."
But let's be honest: being pregnant doesn't change your sexual history. And it doesn't mean that your partner will be faithful. People do cheat sometimes. A past infection can come back sometimes. There are times when someone really doesn't know they're sick. This isn't about shame; it's about biology, reality, and safety.
A 2023 survey published in Sexually Transmitted Diseases found that almost 60% of OB/GYNs said they rarely offered STD testing after the first trimester unless the patient asked for it or showed clear signs of having one. It's not malice; it's stress from time, insurance billing, old rules, and, yes, implicit bias.
Women of color, trans people, and people on Medicaid are statistically more likely to not get tested or to have to wait longer for treatment. Research from the NIH has shown that structural racism in healthcare leads to differences in the outcomes of congenital syphilis.
You should get better. You should know that asking about more tests doesn't make you "paranoid" or "extra." You are taking the initiative. You are keeping yourself and your child safe. And that's never something to be ashamed of.
What At-Home Testing Offers That Clinics Might Miss
Let’s say you want to test again, but your OB says no, or your insurance doesn’t cover it. Or maybe you just feel embarrassed asking. That’s where at-home STD testing comes in, and not just as a convenience. As an equalizer.
At-home STD kits let you test on your own schedule, in your own space, for the infections most likely to affect your pregnancy. No awkward conversations. No delayed follow-up. Just answers, fast, clear, private.
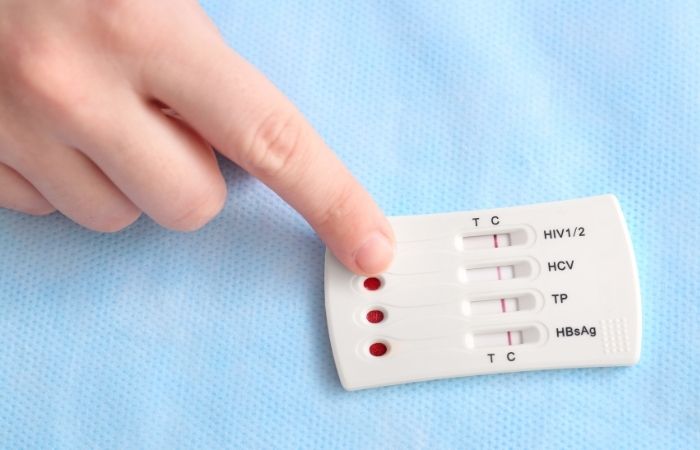
Some kits, like the Combo STD Home Test Kit, screen for multiple infections at once: syphilis, chlamydia, gonorrhea, and HIV. And yes, they’re pregnancy-safe. Blood and urine-based testing doesn't interfere with your pregnancy and can detect early infections that standard prenatal panels miss.
Of course, follow-up with a provider is crucial if anything comes back positive. But the power of testing, deciding when and what to test for, should belong to you. Not a billing system. Not a rushed 15-minute prenatal visit. You.
People are also reading: How High Is the Risk of Getting STDs from Sex Workers?
“I Didn’t Know He Could Give It Back to Me”, When Partners Aren’t Tested
Here’s a quiet heartbreak most people don’t talk about: reinfection. You test early in pregnancy, maybe even catch something like chlamydia or syphilis. You get treated. It’s all handled. But your partner? He never got tested. Or he said he did but never showed you the results. And you’re too tired, too trusting, or too overwhelmed to press the issue.
So what happens? You have sex again. Maybe with a condom, maybe not. And just like that, you get reinfected, sometimes without knowing it. And the clock keeps ticking. Your baby keeps growing. The infection keeps spreading.
“I didn’t know he could give it back to me,” said Alondra, who was treated for chlamydia at 10 weeks but tested positive again during labor.
“I thought once I took the pills, I was good. My OB never told me we both had to be clear.”
This is the hard truth: you can’t fully protect yourself without partner testing. And yet, many pregnant people are never told this. In some prenatal clinics, providers don’t even ask about the partner’s status unless the patient volunteers it. There’s no built-in protocol for “treat the couple.” Just “treat the pregnant person and move on.”
That’s a failure of public health, and it’s avoidable. You can request partner testing through most clinics. Or, if that’s not safe or feasible, you can encourage it privately with an at-home test. Either way, this isn’t just about your health, it’s about your baby’s first environment. Their bloodstream. Their immune system. Their future.
Yes, It’s Safe to Treat STDs During Pregnancy, Here’s What That Looks Like
If you’re worried that treatment might hurt the baby, pause. The real risk isn’t the medication. It’s the untreated infection.
Syphilis? One shot of penicillin is the gold standard and safe during pregnancy. It’s been used for over 70 years and remains the most effective way to prevent congenital syphilis.
Chlamydia? A course of azithromycin or amoxicillin, both considered safe by the World Health Organization. No, it won’t interfere with your prenatal vitamins or ultrasounds. No, it won’t “poison” the fetus.
HIV? It’s more complex, but if caught early, antiretroviral therapy (ART) reduces the risk of transmission to under 1%. You can carry to term. You can deliver safely. You can live a long, healthy life with your child. But only if you know. Only if you treat.
And if someone tells you that testing or treatment is too “risky” while pregnant, ask for a second opinion. Or a third. Or go directly to trusted resources like Planned Parenthood or the STD Rapid Test Kits knowledge base.
You’re not being dramatic. You’re being protective. That’s not overthinking, it’s parenting.
Check Your STD Status in Minutes
Test at Home with Remedium7-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $129.00 $343.00
For all 7 tests
Sex, Testing, and the Shame No One Warned You About
Let’s talk about the quiet shame. The moment someone hears “STD” in a prenatal clinic and flinches. The nurse who changes her tone. The look your partner gives you in the car. The friend who says, “Well, I didn’t have to get retested. Why did you?”
Pregnancy is supposed to be a time of joy, right? Glowing skin, gender reveals, baby showers. But for a lot of people, it’s also a time of secrets. Silent infections. Unspoken fears. And the pressure to be “perfect.”
But perfection is a myth. And infections don’t care about your character. You can get chlamydia the first time you try oral sex. You can get herpes from someone who doesn’t know they have it. You can contract syphilis during a monogamous relationship because someone wasn’t honest, or didn’t know either.
This isn’t about being “clean.” This is about being informed. And safe. And yes, still sexy, still curious, still fully deserving of pleasure, even while pregnant.
“I didn’t stop wanting intimacy just because I was pregnant,” said Ty, a queer nonbinary parent who contracted syphilis during their second trimester.
“I wish I’d known that having symptoms didn’t make me dirty. It just meant I needed care.”
STD testing doesn’t mean you did something wrong. It means you’re doing something right. For your body. For your baby. For your future.
FAQs
1. Wait… so can I really get tested for STDs while I’m pregnant?
Yes. 100% yes. And you should, especially if it hasn’t been done since your first trimester. Blood, urine, and swab tests are safe for you and your baby. It’s one of the few things in pregnancy that’s quick, painless, and actually gives you clarity instead of more questions.
2. But didn’t my OB already test me for everything?
Probably not everything. Most prenatal panels check for HIV and syphilis early on. Sometimes they’ll include chlamydia or gonorrhea, especially if you're under 25. But herpes? HPV? Trich? Unless you’ve got visible symptoms or you explicitly asked, nope. It’s not automatic, and most doctors won’t mention it unless you bring it up.
3. I’m in a monogamous relationship. Do I really need to get tested again?
Listen, monogamy doesn’t always mean safety, especially if there’s been any infidelity, past infections, or you’re not 100% sure about your partner’s history. No shame, no assumptions. You can love someone deeply and still protect your body. A quick retest now can prevent long-term heartbreak later.
4. What if I don’t have any symptoms?
Most people don’t. That’s the trap. Chlamydia? Quiet. Syphilis? Might just look like a bug bite or nothing at all. HIV? Could feel like a cold or flu. Don’t wait for fireworks, STDs during pregnancy are often invisible. Test anyway.
5. Okay but… will the treatment hurt my baby?
Nope. The real risk is not treating. Medications like penicillin, azithromycin, and certain antivirals are totally safe during pregnancy. You’ll likely get a shot or a short round of pills, and that’s it. One uncomfortable moment now could spare your baby from lifelong complications.
6. My doctor brushed it off when I asked about retesting. What should I do?
Ask again. Push back. Or go around them. Your doctor works for you, not the other way around. If you’re not being heard, get a second opinion, or use an at-home test to take matters into your own hands. Testing yourself isn’t being dramatic. It’s being responsible.
7. Can I give my baby an STD without knowing I have one?
Sadly, yes. That’s why testing is so important. Some infections, especially syphilis and HIV, can cross the placenta. Others, like chlamydia and gonorrhea, are passed during delivery. The earlier you find out, the easier it is to prevent transmission. Knowledge = power (and prevention).
8. What if I tested negative before but I’ve had sex since then?
Then it's time for another test. Your status can change anytime there’s new sexual contact, especially if protection wasn’t used consistently. A negative test in the first trimester doesn’t mean you’re still negative in the third. Life happens. Just retest.
9. I’m embarrassed to talk to my partner about testing. Help?
Totally normal. Try this: “Hey, my doc said I should get retested just to be safe, wanna do it together?” Or blame it on me (seriously): “I read this article that said partners should test too.” Keep it low-drama, high-care. If they push back hard? That’s a red flag, not a reflection of you.
10. Is it too late to do anything if I’m close to my due date?
Not at all. In fact, some treatments, especially for syphilis, can still protect your baby even if started late in pregnancy. It’s never too late to check, to treat, or to give your baby the safest start possible.
Don't Hesitate. Get Tested.
You don’t need anyone’s permission to get tested again. You don’t need to explain why you want peace of mind. You don’t need to wait for symptoms or scare tactics or someone else to finally take your concerns seriously.
What you do need, what you already deserve, is clarity. Whether your doctor offered it or not. Whether your partner’s been supportive or silent. Whether your pregnancy has felt like a celebration or a minefield of what-ifs.
Testing isn’t shameful. It’s survival. And it’s love, real love, for yourself, for your baby, for your future.
This at-home combo test kit checks for the most common STDs discreetly and quickly. Whether you're retesting mid-pregnancy, double-checking after an exposure, or just trying to feel safe again, it’s one small step for long-term peace of mind.
Sources
1. CDC – Screening & Testing for HIV, Hepatitis, STDs in Pregnancy
2. CDC – Pregnant Women & Syphilis Trends (NCHS Data Brief)
3. CDC – About STIs and Pregnancy
4. Johns Hopkins – Why Syphilis Is Spiking in the U.S.
5. PubMed – Congenital Syphilis Incidence Trends (Narrative Review)










