Quick Answer: Red spots on the vulva can be caused by shaving, friction, allergies, or STDs like herpes. Testing is the only way to be sure, especially if the spots come back, blister, or happen at the same time as other symptoms like tingling, discharge, or burning.
This Guide Is for Anyone Who’s Looked Down and Freaked Out
Whether it’s your first time seeing something unfamiliar, or you're someone who’s been through this before but still worries every time, this guide is built for you. You might’ve just shaved. Or maybe you had unprotected sex last weekend and now you’re spiraling because a red bump popped up. You might even be thinking back to an ex, wondering if this is karma, coincidence, or a delayed reaction.
This guide covers what causes red spots on the vaginal area, how herpes usually shows up, what non-STD causes to consider, and most importantly, what to do next. We’ll walk you through timelines, symptoms, and testing, using micro-stories and science to help you get real answers without spiraling.
Because we know the real question isn’t just “What is this spot?”, it’s “Am I going to be okay?” And the answer is yes. You are. But let’s get you the information to prove it.
Scene Check: “I Swear It Was Just a Heat Rash...Until It Wasn’t”
Jasmine, 27, brushed it off at first. She'd just gotten back from a music festival, had been wearing tight biker shorts in 90-degree heat, and had hooked up with someone she’d known for a few weeks. The tiny red dots along her inner thighs and labia felt like irritation, not infection. No pain, no itching. Just...there.
By day three, they hadn’t gone away. A few looked shinier. She Googled “red spots after sweaty weekend” and was convinced it was heat rash. But a week later, one of the spots opened up slightly, just enough to sting when she peed. That’s when she panicked. She ordered an at-home test kit. Her results came back positive for herpes simplex virus type 2.
Jasmine’s story isn’t rare. And neither is the confusion that comes before the diagnosis. The vulva is delicate, exposed, and affected by everything, from what you wear to who you sleep with to what’s in your laundry detergent. But herpes and heat rash often look similar in the early stages. Here’s how to tell them apart.
Herpes vs Heat Rash: The Visual, The Feel, and the Timeline
Spotting the difference isn’t just about what it looks like, it’s about how it feels, when it shows up, and what happens next. Let’s break that down.
| Symptom Feature | Heat Rash | Herpes |
|---|---|---|
| Appearance | Flat or slightly raised red dots; may feel prickly or itchy | Small fluid-filled blisters or clustered red sores |
| Location | Common on inner thighs, groin folds, areas with trapped sweat | Often on labia, vagina, anus, or where skin-to-skin contact occurred |
| Pain or Tingling | Mild itch or irritation, usually not painful | Tingling, burning, or stinging even before blisters appear |
| Onset Timing | Often hours after sweating or friction | 2–12 days after exposure (first outbreak); recurring episodes later |
| Duration | Resolves in 2–3 days with cooling and hygiene | Lasts 7–14 days; sores may scab and heal over time |
Figure 1. Symptom comparison between heat rash and genital herpes.
The big giveaway with herpes? It usually doesn’t go away quickly. Even if the sores are small or painless, they tend to linger or return. Heat rash, on the other hand, is quick to fade once the skin cools and air hits it. If you’ve had the same red spots for more than 3–4 days, or they’re starting to change shape, hurt, or form scabs, it’s time to test.

People are also reading: Yes, You Can Give Someone Genital Herpes With a Cold Sore
Not Just Herpes or Heat Rash: Other Possible Culprits
If you're staring at a mirror or phone camera trying to diagnose your own crotch, breathe. Let’s zoom out. Red spots don’t automatically mean STDs or skin infections. The vulvar area is affected by everything from hormones to hygiene to pressure and posture. Here's what else can cause redness that mimics STDs:
Shaving or waxing? Razor bumps and ingrown hairs can look angry and red, especially near the bikini line. New soap? You could be reacting to fragrance or pH imbalances. Wearing tight pants or synthetic underwear during a hot day? Hello, friction rash. And don’t overlook yeast infections, they don’t always cause discharge first. Sometimes it starts with irritation and redness near the skin folds.
Still, even doctors sometimes misdiagnose herpes as “just irritation” on first glance. That’s why testing matters. Not just to catch STDs, but to rule them out confidently so you’re not stuck in Google purgatory.
Check Your STD Status in Minutes
Test at Home with RemediumGenital & Oral Herpes Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $75.00 $98.00
For all 2 tests
How Long Should You Wait Before Testing?
Here’s where things get tricky, and where most people make one of two mistakes: testing too soon or waiting too long because they’re scared. With herpes, timing is everything. If you test too early, especially after your first exposure, the virus might not be detectable yet.But if you wait too long, especially after you start to see symptoms, you could put off treatment and spread it without meaning to.
Let’s say you had sex with someone new five days ago, and now you see a red spot. You’re anxious and want answers now. Totally fair. But here’s the truth: if it’s herpes, the first outbreak usually shows up between 2 and 12 days after exposure, and testing accuracy improves the longer you wait after symptoms appear.
If you have visible sores or blisters now, a swab test from a clinician or urgent care is the fastest way to confirm herpes. If you're using an at-home blood test, it's best to wait at least 3–4 weeks after exposure so antibodies can develop. Herpes antibody tests won’t detect new infections right away. And if you already have herpes type 1 from childhood (cold sores), blood tests may be inconclusive unless it’s HSV-2.
Here’s a visual breakdown of testing timelines and accuracy across the most likely causes:
| Cause | Best Time to Test | Testing Method | Notes |
|---|---|---|---|
| Herpes (HSV-1/HSV-2) | 3–12 days (swab), 4+ weeks (blood test) | Swab of active sore or blood antibody test | Swab needed if symptoms are present; antibodies take time to show up |
| Yeast Infection | During symptoms | Swab or self-assessment + OTC response | Often causes redness, itching, cottage-cheese discharge |
| Heat Rash | No test needed | Resolves on its own | If it disappears in 48–72 hours, no further steps needed |
| Chlamydia / Gonorrhea | 7–14 days post-exposure | Urine or swab NAAT test | Rarely causes red spots but may coexist with herpes |
Figure 2. When to test for common causes of vulvar redness and irritation.
If you’re still unsure what to do, here’s a rule of thumb: if the spot is changing, hurting, or not fading in 3–4 days, test. If it's lingering beyond a week or has returned more than once in the same place? Almost certainly time to check for herpes.
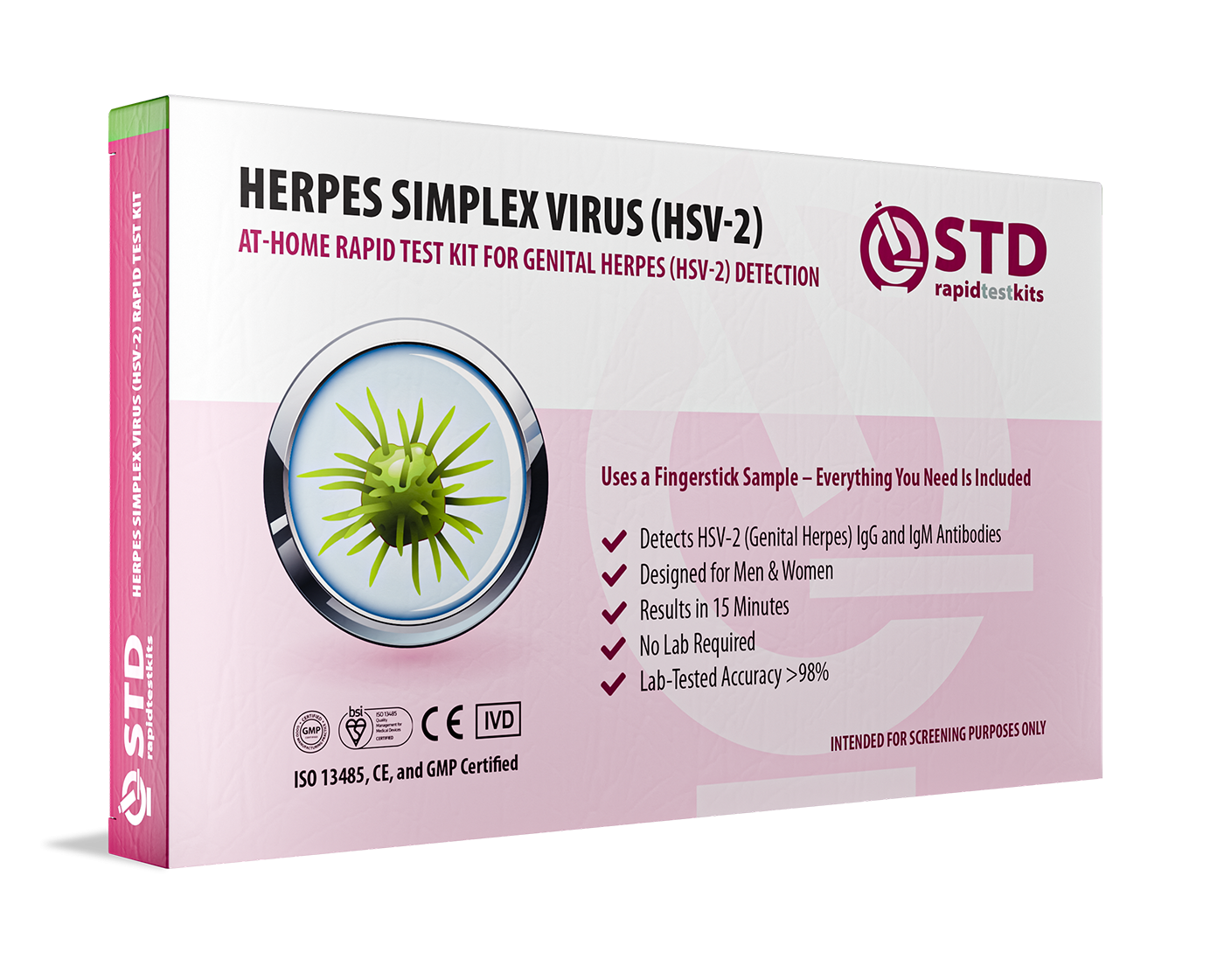
Testing at Home: Peace of Mind in a Box
It’s late. You’re in bed, half-scrolling, half-worrying, and definitely not going to sleep anytime soon. You don’t want to go to urgent care. You don’t want to tell your new partner. And you’re not ready to walk into Planned Parenthood with a photo of your vulva.
That’s where at-home testing comes in. You can discreetly order a combo STD test kit that screens for the most common infections, including herpes, chlamydia, and gonorrhea. Some kits use finger-prick blood, others use swabs or urine. Many arrive in plain packaging and include everything you need to test privately.
If your red spot turns out to be nothing, great. Relief. If it turns out to be herpes, also great. Because now you know. Now you can treat it, manage it, and talk to partners responsibly.
Whether it’s a bump or a question mark, you deserve to know. This at-home combo test kit can help.
When It’s Time to See a Doctor (And What to Expect)
If you're not ready to test at home, or if your symptoms are severe, burning pain, trouble peeing, swelling, or a fever, it’s time to visit a provider. Genital herpes is usually diagnosed via swab during an active outbreak. Many clinics offer same-day results, or at least faster than you’ll get scrolling TikTok for photos of “herpes day 2 vs razor burn.”
Don’t be surprised if your doctor doesn’t do bloodwork unless you request it. Many clinics only test visible lesions, and not all providers will suggest an HSV blood test right away. That’s why it’s helpful to go in with questions prepared. Ask: “Can you swab this now?” and “Can we test for both HSV-1 and HSV-2?” Knowledge is power. And asking questions doesn’t make you dramatic, it makes you smart.
Herpes is common. More common than you think. In fact, according to the CDC, about 1 in 6 people aged 14 to 49 in the U.S. have genital herpes. That means you probably know someone who has it. You just don’t know they do, because most people never show symptoms, or never talk about them if they do.
If your doctor says it looks like herpes but doesn’t test you, ask again. If they tell you it’s “probably nothing” but your gut says otherwise, test anyway. This is your body. You’re the one who has to live in it. Not them.
What If the Spot Disappears Before You Test?
Here’s the most frustrating part: many people finally decide to get tested, and the spot is gone. No redness. No bump. No sign it ever existed. And suddenly they feel silly, anxious, or unsure about what to do next.
If this is you, you’re not alone. Herpes lesions, especially early or mild ones, can heal quickly, sometimes in under a week. And a visual swab test only works if the lesion is active. Once it scabs over or vanishes, a swab can’t pick up the virus anymore.
That’s where herpes blood testing comes in. These tests detect antibodies your body creates in response to HSV-1 or HSV-2. But they don’t show up right away. Most experts suggest waiting 4–6 weeks post-exposure for accurate results. The test might still miss a very recent infection, but it’s a good next step if a spot has healed or you’re unsure about your history.
We know that waiting sucks. That the in-between time feels like torture. But knowing when and how to retest gives you power. It replaces spiraling with a plan.

People are also reading: Why HIV Rates Are Higher in Black Gay Men, And How to Protect Yourself
Tested Positive for Herpes? You’re Still the Same Person
Let’s say the test comes back positive for HSV-2. You see that tiny text, and your stomach drops. Your brain might fill in the worst-case scenarios: Will anyone want me? Did I ruin my life? Is this forever?
Pause. Breathe. It’s okay to be scared. But here’s the truth: a positive test doesn’t change who you are. It just gives you a piece of information you didn’t have before. It means you can take care of yourself more precisely, protect your partners more intentionally, and navigate sex with honesty and confidence.
Plenty of people have herpes. They date. They have sex. They fall in love. They have kids. They thrive. Herpes is not a punishment, and it’s not a dealbreaker. It’s an infection, one that’s manageable with meds, boundaries, and good communication.
Here’s what happens next:
You’ll talk with a provider about suppressive or episodic antiviral treatment. Most people use meds like valacyclovir to reduce outbreaks and transmission risk. You’ll figure out your patterns, how your body reacts to stress, sex, friction, or illness. And eventually, it will become part of your routine, not your identity.
If you're not ready to talk to a doctor yet, that’s okay too. Start with a discreet test. Then decide what to do next, one step at a time.
Check Your STD Status in Minutes
Test at Home with RemediumGenital Herpes Test Kit
 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $45.99 $49.00
Partner Talk: How to Share Without Shame
Maybe the red spot is gone. Maybe you’ve tested and now you’re waiting for results. But there’s another thing hanging over you: your partner. Or partners. Do you tell them? When? How?
This part can feel worse than the symptom itself. But it doesn’t have to be a confession. Think of it as care. A heads-up. A way to make sure you both stay informed, safe, and empowered. If you're in a newer relationship, you can keep it simple: “Hey, I noticed something weird going on down there and I’m getting tested. Just wanted to let you know in case you want to do the same.”
If you’ve tested positive, try: “I just found out I have HSV-2. I didn’t know until now, and I want you to have the info too. I’m learning more and looking into treatment, but I care about being upfront.”
You don’t have to say it perfectly. Just say it honestly. Anyone worth your time will respect you more for telling the truth. And if they freak out or shame you? That’s about them, not you.
Need support? Resources like ASHA and Reddit’s r/Herpes community are full of people navigating the same thing with humor, grace, and honesty.
Privacy, Testing, and Getting the Answers Without the Drama
Let’s be real: walking into a clinic and asking someone to look at your vulva is not on anyone’s vision board. Even with the best providers, it can feel invasive, exposing, and sometimes even humiliating. That's why STD tests you can do at home are so important, especially for people who have anxiety, trauma, or just everyday shame.
When you order from STD Rapid Test Kits, you’re not just buying a test. You’re buying privacy. Your kit arrives in discreet packaging. Your name isn’t blasted across the box. You do everything in the comfort of your own space. And you get results that help you move forward.
Are you not sure which test to take? We suggest the Combo STD Home Test Kit if you have a mystery spot because it tests for more than one infection at once. If your symptoms are similar to those of herpes, you might want to get a herpes-specific test and follow up if necessary.
Your health deserves clarity, not confusion. Your body deserves care, not guesswork.
FAQs
1. Is every red bump down there a sign of herpes?
Nope. Not even close. Your vulva deals with a lot, shaving, sweat, friction, hormones, underwear seams. All of it can cause red spots. But if the bump blisters, burns, or keeps coming back in the same place? That’s when you might want to rule out herpes with a test.
2. How can I tell if it's just irritation or something serious?
If it fades fast, like in a day or two, and doesn’t hurt or change, it’s probably nothing serious. Razor burn, friction rash, mild allergic reactions can all cause redness. But if it lingers, stings when you pee, or morphs into a sore? That's your sign to test, not guess.
3. Can herpes really show up without any pain at all?
Totally. Some people have no idea they have herpes until it pops on a test. Others just notice “a weird red dot” that doesn’t itch or hurt but won’t go away. Pain isn’t required. That’s why herpes slips under the radar so often, and why testing matters.
4. Do I need to wait weeks to test for herpes?
Depends on the test. If you’ve got a visible sore now, you can get it swabbed right away. But if you're doing a blood test for herpes antibodies, you’ll need to wait at least 4–6 weeks after exposure for it to be accurate. Otherwise, the test might miss it.
5. What’s the point of at-home testing if I’m not sure what this is?
At-home kits are for anyone who wants answers without drama. If you’re staring at a bump, unsure what it means, a combo STD test kit can give you clarity on herpes, chlamydia, gonorrhea, and more, all from your bathroom, no exam table required.
6. Can I give someone herpes even if I don’t have symptoms?
Yes, and this is what makes herpes sneaky. It can shed and spread even when you feel totally fine. That’s why people who don’t even know they have it still pass it to partners. It’s not about blame, it’s about being informed.
7. If I test positive, is this my life now?
In some ways, yeah, but not in the “everything’s ruined” way you’re imagining. People with herpes date, have amazing sex, get married, have kids, and live full lives. You’ll learn your triggers, manage outbreaks, and go on being exactly who you were before, just a little more equipped.
8. How do I even tell someone I might have herpes?
Like this: “Hey, I noticed something going on, and I’m getting tested just to be safe. Wanted to be upfront in case it matters for you too.” That’s it. You don’t need a script, just honesty and calm. And if someone bails because of that? Good. They weren’t built for real-life intimacy anyway.
9. What if I got a negative result but I’m still not convinced?
Then test again. It could’ve been too soon, or the test type might not have matched your situation. Follow your gut. Your peace of mind is worth a second round, and your body’s still talking, even if the test didn’t catch it yet.
10. Does herpes mean I have to give up sex?
Not even close. It just means learning how to protect partners and manage your health. Most people with herpes continue to have sex, it just comes with more awareness, better conversations, and sometimes a little planning. Your sex life isn’t over. It’s just evolving.
You Deserve Answers, Not Assumptions
If you’ve made it this far, you’re probably not just curious, you’re concerned. And that’s okay. Having a red spot down there doesn’t mean something is wrong with you. It means your body is telling you something. The best way to respond? Don’t guess. Don’t panic. Test.
Don’t wait and wonder, get the clarity you deserve. This at-home combo test kit checks for the most common STDs discreetly and quickly. Your body deserves better than a Google spiral.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate.
Sources
1. Planned Parenthood – Herpes Overview
2. American Sexual Health Association – Herpes Support
3. Reddit – Herpes Peer Support Community
7. Genital Herpes – Symptoms & Causes – Mayo Clinic
8. What Does Herpes Look Like? – Verywell Health
9. Genital Skin Problems – DermNet NZ
10. Genital Rash: Causes & How to Identify – Verywell Health
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: A. Liyah Santiago, MPH | Last medically reviewed: October 2025
This article is for informational purposes and does not replace medical advice.










