Quick Answer: A single line on the control (C) area means negative. Two lines, no matter how faint, can indicate Hepatitis C antibodies, meaning you’ve been exposed and need confirmatory testing. No control line? The result is invalid, and you’ll need to retest.
That Tiny Line Can Feel Like a Sledgehammer
Dion, 34, took an at-home rapid Hepatitis C test after learning an old partner had recently tested positive.
“The second line was so faint I thought I imagined it,” he said. “I didn’t know if I had it, had beat it, or needed to start making calls.”
And that right there is the problem. A rapid test tells you whether you’ve ever developed antibodies to Hepatitis C (HCV), but it doesn’t confirm if the virus is still active in your body. That second line? It means you’ve likely been exposed, but your body’s response to that exposure might be ongoing, resolved, or just starting. That’s where most people get confused, and where most of the internet doesn’t explain clearly.
So let’s break it down: what that line means, when to trust it, and what comes next.
People are also reading: Discharge After Sex: What’s Normal and What Isn’t
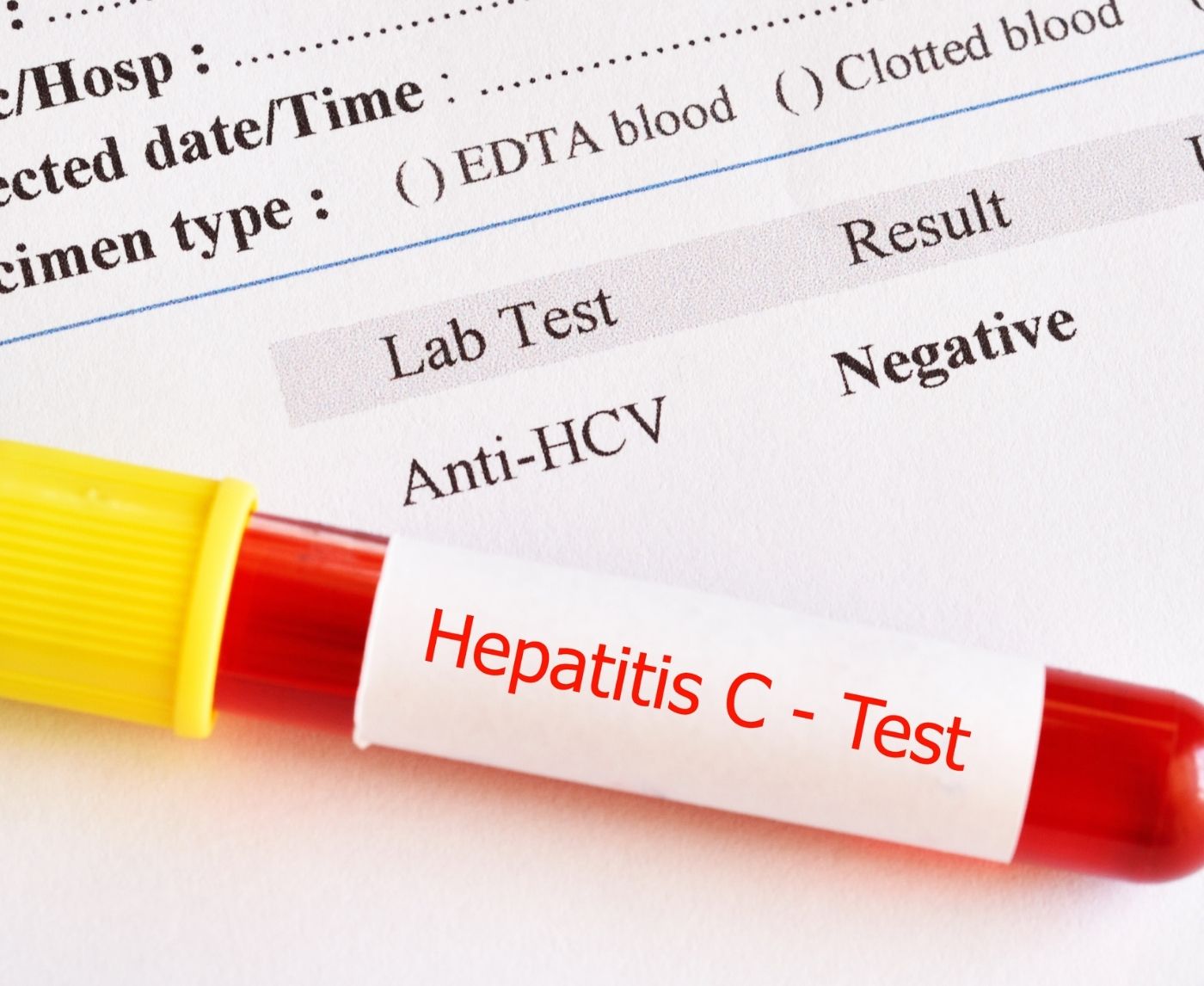
How Hepatitis C Rapid Tests Work
Rapid tests for HCV typically detect antibodies, not the virus itself. When your body encounters Hepatitis C, your immune system creates antibodies to fight it off. These antibodies can stay in your system even after the virus is gone, or while it’s actively causing damage.
The test uses a fingerstick blood sample and reacts with reagents embedded in the cassette strip. After about 15–20 minutes, you’ll see the result window display one of three outcomes:
- Negative: One clear line next to “C” (control), nothing next to “T” (test)
- Positive: Two lines, one at “C,” one at “T.” The test line can be faint or dark
- Invalid: No line next to “C.” Doesn’t matter what’s at “T”, the test didn’t run properly
If your cassette doesn’t look like this within 20 minutes, the result can’t be trusted. And if you see a line where you're not sure it’s really a line… keep reading. We’ll get into faint line syndrome next.
Faint Lines, False Hope, and Freakouts
There’s a special kind of anxiety that comes from seeing a line you didn’t expect, and not knowing what it means. A faint test line still counts as a positive result. That means your body has produced antibodies against HCV. But, and this is important, it doesn’t mean you’re currently infected.
Renee, 28, found herself in this limbo.
“I saw a ghost of a line and panicked. I thought I had Hep C and was going to die. My doctor ordered a viral RNA test, and it turned out I’d cleared the virus years ago without knowing.”
In fact, about 1 in 4 people who contract Hep C clear it naturally without treatment. The antibody stays, but the virus is gone. So if your rapid test is positive, you’ll need a follow-up PCR or RNA test to detect the actual virus in your blood.
Here’s the bottom line: faint line = antibody positive = exposure. Not necessarily active infection. Not necessarily contagious. But absolutely worth following up.
What Your Hep C Rapid Test Result Could Mean
| Test Window Result | What It Means | What to Do |
|---|---|---|
| One line at “C” only | No antibodies detected (negative) | If recent exposure, retest in 3–6 weeks |
| Two lines, “C” and faint or dark “T” | HCV antibodies detected (positive) | Get lab-confirmed PCR or RNA test |
| No line at “C” | Test is invalid (no result) | Repeat test with a new kit |
Table 1. Rapid test results explained. Even faint lines at “T” matter, don’t ignore them.
False Positives, False Negatives, and the Timing Trap
Here’s something that surprises most people: a positive Hep C antibody test doesn’t always mean you have Hep C. And a negative test doesn’t always mean you’re in the clear. Like all rapid tests, timing is everything, and that’s where the most common mistakes happen.
False positives happen when your body produces antibodies similar to those for Hep C, or when there’s a testing error. It’s rare, but it does happen, especially in people with autoimmune diseases, co-infections, or past exposure that has already cleared. That’s why a positive result must always be confirmed with a lab-based PCR test.
False negatives are more common early after exposure. If you take the test too soon, before your immune system has made enough antibodies, it might not detect the virus. This period is called the window period, and for Hep C, it’s typically around 4 to 10 weeks after exposure. Some people seroconvert faster, but many don’t.
That means if you got a needlestick injury, shared a razor, or had unprotected sex with someone at risk, and then tested the next week, you could get a false sense of security. You might still be infected, just not far enough along to trigger the test.
When to Test and Retest for Hep C
| Situation | Best Time to Test | Next Step |
|---|---|---|
| Recent exposure (< 3 weeks) | Wait 4–6 weeks for antibodies to develop | Use PCR if urgent or high-risk |
| Past exposure (1–6+ months ago) | Rapid antibody test now | If positive, confirm with PCR |
| Previously positive test | Skip antibody test | Go straight to PCR/RNA for active infection |
Table 2. Hep C test timing matters. If your exposure is recent, retesting is essential, even if you feel fine.
Common Mistakes When Using Hep C Rapid Tests
Let’s be real: even the best rapid test won’t work if it’s used wrong. And when you’re nervous, sweaty, and poking your own finger, mistakes happen. Here are the most common missteps that lead to inaccurate results, or just wasted tests:
- Testing too early. Your body needs time to create detectable antibodies. Testing within a week or two of exposure is often too soon. Unless you use a PCR test, you'll need to wait and possibly retest.
- Not adding the buffer properly. That little bottle of reagent matters. If you skip it, use too much, or spill it, the chemical reaction that detects antibodies won’t happen correctly.
- Misreading the result time window. Most rapid tests must be read within 15–20 minutes. Too soon, and the line hasn’t developed. Too late, and you may see evaporation lines or false shadows.
- Ignoring faint lines. If there’s a line at “T,” even if it’s barely visible, you need a confirmatory PCR. Don’t chalk it up to wishful thinking or lighting. A line is a line.
- Reusing lancets or test kits. Each kit is single-use only. Reusing parts, especially the lancet, increases infection risk and invalidates results.
“I Thought I Was Negative, Then I Wasn’t”
Kevin, 39, used a rapid test 10 days after he shared needles during a brief relapse.
“I tested negative and thought I was okay,” he said. “But six weeks later, I started feeling tired all the time. I retested and saw two lines.”
A PCR confirmed active Hep C. His mistake wasn’t uncommon. Testing too early can miss infections, especially if the exposure was recent. Symptoms like fatigue, nausea, or dark urine often come later, and by then, you’ve already gone weeks thinking you’re fine.
Kevin started treatment early and cleared the virus completely. But he only got there by retesting.
Check Your STD Status in Minutes
Test at Home with RemediumHepatitis C Test Kit
 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $33.99 $49.00
Take the Guesswork Out, Here’s What to Do Next
Here’s the good news: Hepatitis C is curable. And finding out early makes everything easier, treatment, recovery, and peace of mind. If your test is positive (even faintly), the next step is clear: get a PCR or RNA test to confirm whether the virus is active.
And if you tested negative but the exposure was recent, plan a follow-up test in 4 to 6 weeks. This isn’t about fear, it’s about accuracy.
Don’t let a confusing result keep you stuck in limbo. This combo STD test kit checks for multiple infections discreetly, giving you clarity without judgment.
You're not alone in this. You just need answers, and you deserve ones you can trust.
When the Test Doesn’t Work: Dealing With an Invalid Result
You did everything right, or so you thought. But now you're holding a test with no line at “C,” maybe a smudge near “T,” and no clue what just happened. That’s what’s known as an invalid result, and it means the test didn’t run correctly. Period.
It doesn’t mean you’re negative. It doesn’t mean you’re positive. It means… absolutely nothing. Something interrupted the chemical process, maybe a clogged sample pad, old buffer solution, or an error in timing, and the control line never appeared to confirm that the test functioned.
If that happens, breathe. Toss it, grab a new kit, and retest. Invalids aren’t your fault, and they’re more common than people admit. Especially if you're testing under stress, sweating over the result window, or fumbling with a tiny reagent vial at 2AM in your bathroom.
If you’re using a multi-test kit and one works while another fails, don’t assume your results cancel each other out. Treat each test on its own terms. When in doubt, repeat.
What Rapid Test Results Actually Look Like
Many people panic because their result doesn’t look like the marketing photo. But real-world test cassettes are rarely that crisp and color-perfect. Here's how to interpret what you're seeing in plain terms:
- Clear, bold lines: Easy. “C” only = negative. “C” and “T” = positive.
- Faint second line: Still positive. Even if it's barely there, it means your body has responded to Hep C.
- No control line: Test is invalid, doesn't count, no matter what else you see.
- Blurred or bleeding ink: Could mean too much blood, old kit, or defective strip. Don't trust it.
- Pink background haze: Usually fine. It’s just how the fluid runs. If lines are visible, interpret them normally.
Still unsure? Take a photo and bring it to your provider. But don’t sit in silence or assume. These results can be confusing even for seasoned clinicians. You’re allowed to ask for clarity.

People are also reading: This STD Can Still Spread Through “Protected” Sex
“The Line Was Barely There, But It Changed Everything”
Sasha, 41, had no symptoms. She tested “just to be safe” after her ex mentioned a Hep C scare.
“When the second line showed up faint, I almost threw the test away,” she said. “I thought it was defective.” But a follow-up PCR confirmed she had chronic Hepatitis C.
She started antiviral therapy and cleared the virus within months. “If I hadn’t trusted that tiny line, I’d still be walking around with it,” she said.
This is why every line matters. And why testing isn’t about shame or paranoia, it’s about catching what your body might not be telling you yet.
Your Mind Is Probably Racing, Let’s Ground It
If you’re here, staring down a result that you didn’t expect, know this: it’s okay to be overwhelmed. It’s okay to feel scared. But you’re not broken. You’re not dirty. And you’re definitely not alone.
Testing is an act of self-care, not a punishment. And a result, whatever it is, isn’t the end. It’s just information. Most people who test positive for Hepatitis C today will be cured with 8 to 12 weeks of antivirals. No stigma. No needles for life. No tragic TV plots.
And if your result was negative, but the exposure was real? Good. You caught it in time. Retest later and stay alert. That’s how prevention works, not just protection, but proactive care.
STD Rapid Test Kits makes retesting easy. Whether you need confirmation or peace of mind, discreet kits are ready when you are.
Check Your STD Status in Minutes
Test at Home with Remedium10-in-1 STD Test Kit

 For Women
For Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $189.00 $490.00
For all 10 tests
FAQs
1. What does a faint line even mean? Am I positive or not?
If there’s a second line, faint, bold, ghostly, whatever, it still means your body has made antibodies to Hep C. That doesn’t confirm you’re infected right now, but it does mean your immune system once met the virus. You need a PCR or RNA test next to check if it’s still hanging around.
2. Can I trust the result if I took the test too soon?
Not really. If you tested within the first few weeks after exposure, your body might not have built enough antibodies yet. That early phase is what’s called the “window period.” Think of it as your immune system still waking up. If you're testing early, plan to do it again in 4–6 weeks to be sure.
3. So… if I test positive, does that mean I have Hep C forever?
No, and thank science for that. Some people naturally clear the virus, about 25%, and for the rest, treatment cures it in most cases. A positive antibody result is like a breadcrumb trail. It tells you there’s a history, but only a PCR test can tell you what’s going on right now.
4. Is a faint line more likely to be a mistake?
It’s easy to think so (especially when you’re squinting under bathroom lighting at 2AM), but no. A faint line still means antibodies were detected. The line’s darkness doesn’t equal severity, it’s more about how much antibody was present in your sample. Still, follow-up is key.
5. What if I don’t see any line at all?
Then the test didn’t work, period. You need to see a line at “C” for the result to be valid. No control line? Toss it and redo with a new kit. It happens more than people realize, and it’s not your fault. Maybe the buffer didn’t flow right. Maybe the kit was old. Just don’t assume that a blank test is a clean bill of health.
6. I tested negative, but I still feel off. What now?
Trust your gut, literally. If you’ve had a risk exposure and your body’s waving red flags (fatigue, weird urine, nausea), don’t rule Hep C out just yet. You could be in the window period, or the test could’ve missed something. Retest or go straight to a PCR if symptoms linger.
7. How is the rapid test different from a PCR test?
Great question. Rapid tests check for antibodies, evidence your body has responded to Hep C at some point. PCR tests look for the actual virus. Think of it like: the rapid test finds footprints, the PCR finds the person making them.
8. Can someone test positive and not have symptoms?
Yes, and that’s part of what makes Hep C so tricky. It can hang out quietly for years, slowly damaging your liver, with no major warning signs. That’s why testing matters even if you “feel fine.” Silence doesn’t equal safety.
9. What could mess up the test result?
A few things: testing too early, not using enough blood, skipping or spilling the buffer, reading the result too late, or using an expired kit. It’s not hard to get right, but under pressure, it’s easy to slip up. Just take your time and follow each step like a recipe.
10. Is it weird that I’m scared to even test?
Not strange at all. It's brave of you to even open the kit. It's normal to be afraid. But knowledge is power. You are in charge when you know your status, whether it is good or bad. No matter what happens, you're not alone. There are things you can do next, treatments, and help. You can do this.
Don't Allow Uncertainty to Win, Receive the Clarirty You Deserve
Hepatitis C tests at the pharmacy or your physician's office provide you with something strong: the facts. But the facts come with strings attached sometimes: blurry lines, questionable windows, and surprise results. Don't be shamed into silence or avoidance.
If you’ve tested positive, you're not alone. You're not doomed. And you're not untreatable. Hepatitis C is curable, and you took the hardest step already, getting tested.
If you're unsure about your result, the answer isn't to sit in fear. It's to follow up, confirm, and move forward. Testing doesn't mean you're broken. It means you're informed. And being informed is how people heal.
Need a next step? This discreet at-home combo test kit makes it easy to check for Hep C and other common STDs, all from home, without shame.
How We Sourced This Article: We combined current guidelines from global health organizations with clinical literature, firsthand case studies, and trusted test kit manufacturer data. Our aim is to help you read your Hep C results with clarity and confidence. Below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
1. CDC
2. PMC
3. NCBI
4. StatPearls
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI and viral hepatitis testing. His trauma-informed clinical work combines scientific clarity with a stigma-free approach to testing and treatment.
Reviewed by: Kendall Vance, NP | Last medically reviewed: October 2025
This article is for informational purposes only and is not a substitute for professional medical advice or diagnosis.