Quick Answer: Gonorrhea, chlamydia, and herpes can infect the eye through direct contact with infected fluids during oral sex or genital touching. These infections may cause redness, discharge, swelling, or blurred vision, and require prompt medical treatment.
Why No One Talks About This (But Should)
This isn't some bizarre fluke. It’s just a topic buried under stigma and awkwardness. Most people don’t know that gonorrhea and chlamydia can cause conjunctivitis. Even fewer realize that this can happen during a completely consensual and otherwise low-risk sexual encounter, especially oral sex, where many assume there’s no “real risk.”
If you’ve ever felt confused, gross, or even ashamed wondering whether your eye infection could be related to a hookup, you’re not alone. The discomfort isn’t just physical, it’s psychological. The idea that something so intimate and playful could result in an eye infection feels absurd. But sex isn’t sterile. Fluids move. Hands move. Faces get close. STDs don’t only live where you expect them to.
In clinics, providers often overlook the eyes unless symptoms are severe or the patient knows to ask. You may be treated for pink eye without anyone testing for STDs. The result? Delay in diagnosis, more pain, and potentially permanent vision complications if it’s left untreated. That's why you're here, to get answers early, before things get worse.
Let’s Talk Fluids: How STDs Reach the Eyes
Most STDs infect the mucous membranes, soft tissues like the genitals, mouth, rectum, and yes, the eyes. During oral sex, ejaculation, or even close skin-to-skin contact, infected fluids can reach the eye through splashes, fingers, or indirect contact with secretions. In other words: someone doesn’t need to ejaculate directly into your eye for transmission to occur (though that can do it, too).
Let’s get specific: gonorrhea conjunctivitis can occur when Neisseria gonorrhoeae bacteria comes into contact with the conjunctiva, the thin layer covering the eye. The bacteria doesn’t care where it lands. If it finds a warm, moist environment, it can infect it. That includes your eye socket.
Chlamydia trachomatis can also cause eye infections, especially in babies but also in adults who touch their eyes after touching infected genitals or fluids. Herpes simplex virus, particularly HSV-1 and HSV-2, can result in ocular herpes, manifesting as sores on the eyelids or potentially leading to a more severe corneal infection.
In short: STDs aren’t confined to genital zones. If your eyes were exposed to fluids from an infected partner, even indirectly, they’re at risk. The transmission may seem rare, but in the right scenario, it's more common than you'd think.

People are also reading: Herpes or Just Razor Burn? What That Bump Might Mean
Table: Which STDs Can Infect the Eye (and How)
| STD | Can It Infect the Eye? | How It Spreads to Eyes | Common Eye Symptoms |
|---|---|---|---|
| Gonorrhea | Yes | Fluid contact during oral/genital sex or touching eyes with contaminated hands | Pus-like discharge, swelling, redness, severe pain |
| Chlamydia | Yes | Touching infected fluids then touching eye; less commonly via direct contact | Redness, mucus discharge, irritation |
| Herpes (HSV-1 & HSV-2) | Yes | Skin-to-skin or oral-genital contact; autoinoculation | Sores on eyelids, blurred vision, pain |
| Syphilis | Rarely | Advanced stages can involve eye tissues via blood | Visual disturbances, inflammation |
| HIV | Rarely | Systemic immune suppression may lead to secondary eye infections | Blurry vision, retinal damage (long term) |
Table 1: Common STDs that can infect the eyes through oral-genital contact or fluid exposure. This overview highlights which pathogens pose eye risks and what symptoms to look for early.
Order Now $119.00 $294.00 Check Your STD Status in Minutes
Test at Home with Remedium
6-in-1 STD Test Kit




For all 6 tests
When It’s Not “Just Pink Eye”
Pink eye, or conjunctivitis, is incredibly common, and often harmless. But not all eye infections are created equal. If you’ve recently had oral sex, mutual masturbation, or face-to-genital contact and you suddenly develop redness, swelling, or sticky discharge, it’s time to think beyond seasonal allergies or a dirty pillowcase. Especially if the infection shows up in just one eye and doesn't improve with standard eye drops.
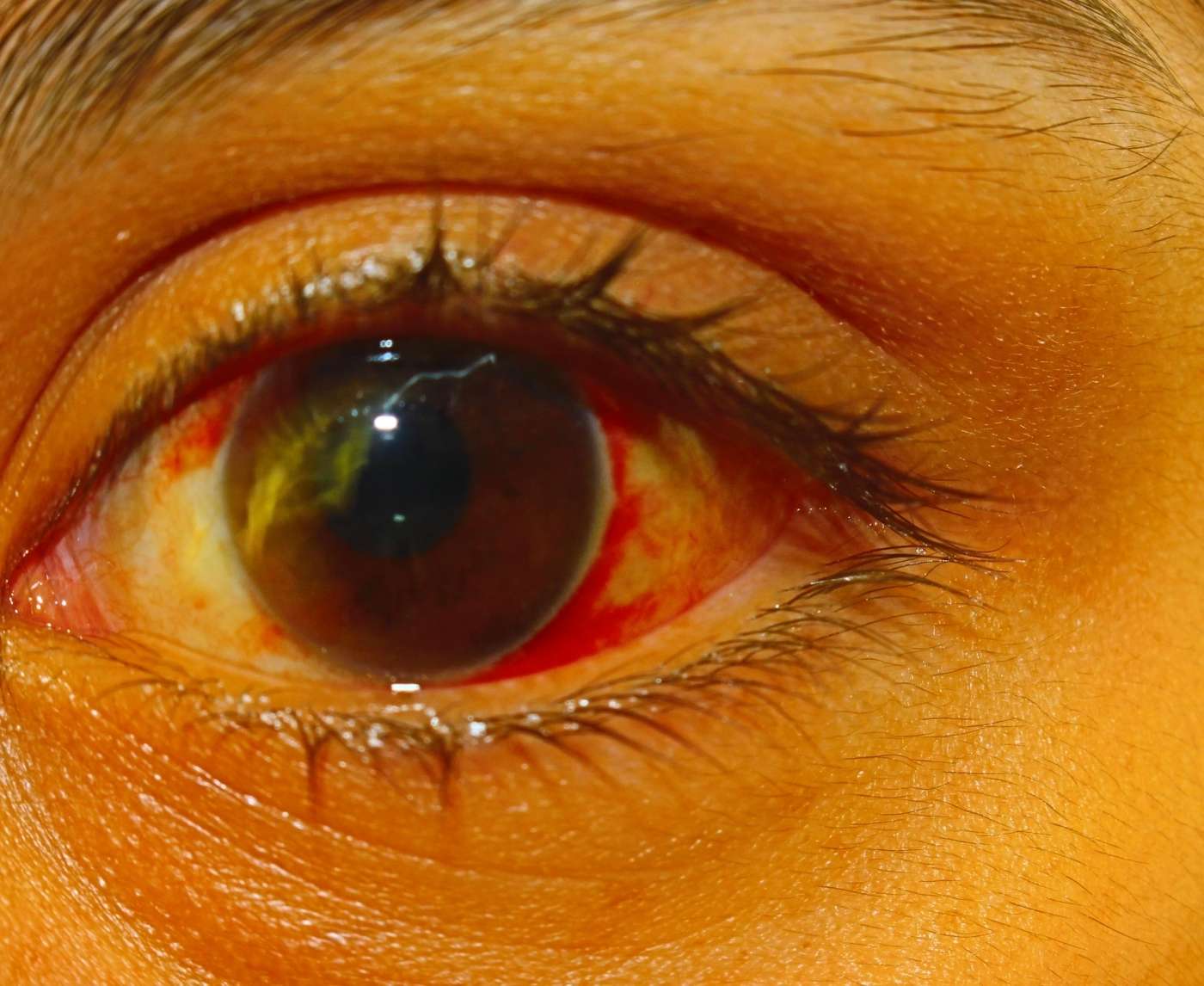
One of the most critical signs that your eye issue might be STD-related is the intensity and color of the discharge. While viral or allergic conjunctivitis usually comes with clear, watery fluid, gonorrhea causes thick, yellow-green pus that can seal the eyelid shut. It often hurts. Badly. The eye may swell to the point of closing entirely. This isn't just an itchy eye, it's a warning flag.
Timing matters, too. Many STD-related eye infections appear within 1 to 3 days after exposure. If you had oral sex over the weekend and your eye started swelling Monday morning, that’s not a coincidence, it could be incubation. Recognizing this early can mean the difference between a short course of antibiotics or weeks of worsening pain and potential vision damage.
Real Case: “I Thought I Was Allergic to His Soap”
Lena, 32, met her new partner on a dating app. Their first night together involved shower play and mutual oral, and by the next afternoon, her right eye was red, itchy, and slightly sticky. She assumed maybe some soap had splashed into her eye. But by Tuesday morning, her eyelid was swollen shut. Over-the-counter drops didn’t help, and by Thursday, she had crust so thick she needed warm compresses just to open it. She finally saw a doctor, who tested her for pink eye, but not for STDs.
It wasn’t until Lena brought up the timing, mentioning the hookup and the oral sex, that her doctor ordered a swab. The result: Neisseria gonorrhoeae detected. She had gonorrhea in her eye. With the right antibiotics, she healed within days. But what if she hadn't spoken up? She might’ve lost vision in that eye.
“I had no idea oral sex could do that. I felt gross, like I’d done something wrong. But I didn’t. I just didn’t know.”
Lena’s story is tragically common. Many people never get correctly diagnosed. They're misdiagnosed with allergic conjunctivitis or standard bacterial infections and don't receive the specific treatment needed for STDs. The shame and silence around eye STDs make them easier to miss, especially for women, who are often told eye issues are cosmetic or coincidental.
STD Eye Symptoms vs Regular Pink Eye
It's important to note that while pink eye can come from many sources, viral infections, allergies, even makeup, STD-related conjunctivitis has distinct markers that should raise suspicion, especially when linked to sexual contact.
| Symptom | STD-Related Eye Infection | Non-STD Pink Eye |
|---|---|---|
| Discharge | Thick, yellow-green pus, may seal eyelid | Watery or clear mucus (viral), milky discharge (bacterial) |
| Pain | Often severe, with burning or stabbing sensation | Mild to moderate irritation or itch |
| Onset | 1–3 days after sexual contact | Gradual or linked to allergy season, illness |
| Other symptoms | Swollen eyelid, blurred vision, possible genital symptoms | Itchy eyes, runny nose, cold-like symptoms (viral/allergy) |
| Response to drops | No improvement with OTC drops | Improves with antihistamines or standard eye treatments |
Table 2: Comparing signs of an STD-related eye infection with typical pink eye. When symptoms are severe, fast-moving, or linked to sexual exposure, STD testing should be considered.
Why Eye Infections From Oral Sex Are Underdiagnosed
There’s a medical blind spot here, literally and figuratively. Most urgent care centers and general clinics don’t automatically consider STDs when evaluating eye complaints. The burden often falls on the patient to say, “I had oral sex recently, and now my eye is infected.” But saying that out loud can feel mortifying.
Many people don’t even think to make the connection. The eye seems like a separate system. If your genitals feel fine, you may not suspect that something sexual could be the cause of an eye issue. That disconnect allows these infections to go untested, and untreated.
Some clinicians also lack training on extra-genital manifestations of STDs. Unless they specialize in sexual health or ophthalmology, they may misattribute the cause, prescribe the wrong antibiotics, or ignore the context entirely. That’s not your fault. But it’s also why being informed is powerful. You don’t have to diagnose yourself, but you do deserve to ask the right questions. And testing is always a good idea when symptoms don’t add up.
When to Test (And What Type of Test You’ll Need)
If you’re dealing with redness, pain, or pus in one eye and you’ve had recent oral sex, or any contact that could involve genital fluids, it’s time to consider STD testing. But not just any test. Standard eye swabs done at urgent care centers often test for common bacterial infections but don’t screen for gonorrhea, chlamydia, or herpes unless specifically requested.
Here’s the problem: the window period for detecting these infections can vary. If your symptoms began within one to three days of exposure, that’s a strong signal that testing now is appropriate. For gonorrhea and chlamydia, most NAAT (nucleic acid amplification) tests can detect the infection from a conjunctival swab or from genital, oral, or rectal samples. However, not every clinic is equipped to process ocular swabs for STDs. You may need to request extra-genital screening, or test your genitals and throat if the encounter included both.
At-home tests won’t screen your eye directly, but they can still give crucial answers. If you suspect you contracted gonorrhea or chlamydia through oral sex, testing your throat or genitals can confirm whether your partner was likely infectious. That can support your doctor's treatment decisions for your eye, even if the eye itself isn’t tested directly.
And if you’re too nervous to go in? STD Rapid Test Kits offers discreet, lab-grade tests you can use from home. It’s not a replacement for eye care, but it can be the first step toward peace of mind.
What About Herpes in the Eye?
Unlike gonorrhea and chlamydia, herpes in the eye doesn’t always cause immediate pus or swelling. It can look like irritation at first, light sensitivity, a scratchy sensation, or what feels like a stye. But HSV can cause deep corneal infections if left untreated. This includes herpes simplex keratitis, a serious condition that can lead to vision loss.
Eye herpes is most commonly caused by HSV-1, the same virus behind cold sores. But if your partner has HSV-2 (typically genital herpes) and you had face-to-genital or oral-to-genital contact, it's possible for that strain to reach your eye as well. That’s why recognizing risk and seeking early treatment matters, even if you don’t see a blister.
Herpes cannot be diagnosed through a typical bacterial swab. It requires a specific viral culture or PCR test. Many doctors skip this unless you request it. If your symptoms are mild but persist or worsen, or you’ve ever had a history of cold sores or herpes outbreaks, flag that during your appointment. Treatment usually involves antiviral medication, not antibiotics, so the wrong treatment can let it fester.
Why Testing Matters, Even If You Think It’s Just Irritation
Imagine this: someone hooks up on a Friday night. By Sunday morning, their eye is swollen and red. They think, “I just rubbed it wrong.” They wait. By Tuesday, it’s worse. By Wednesday, they finally get an eye drop prescription. But it doesn’t work. On Thursday, the eye starts leaking yellow-green pus. The infection spreads. What started as a mild irritation has now become a full-blown case of gonococcal conjunctivitis, possibly threatening their vision.
This timeline happens often. The delay isn’t just due to ignorance, it’s due to shame, confusion, and false reassurance. People don’t want to seem dramatic. They downplay their exposure, or they believe myths like “oral sex doesn’t count.” But gonorrhea doesn’t care what kind of sex it was. If the bacteria gets to your eye, it behaves the same way, fast, aggressive, and damaging.
If you’re wondering whether to test, the answer is probably yes. Especially if you notice worsening discharge, blurred vision, eye crusting, or if over-the-counter treatments aren’t helping. And if you’ve already tested recently but symptoms persist? You may need to retest, or test a different site.
Retesting Windows and Hidden Risks
Retesting is often necessary for STD-related eye infections, especially if your first test was taken too early or came back negative but symptoms continue. This is because bacterial load increases with time, and tests are more accurate a few days into the infection. Testing immediately after exposure, particularly in the first 24 hours, may yield false negatives.
If you test on Day 1 and get a negative result, but your eye symptoms worsen by Day 3 or 4, retesting is smart. The same goes if your partner tests positive after the fact. In that case, you may be infected even if your initial test was clear.
In treatment cases, most clinics recommend retesting two to three weeks after finishing antibiotics, especially if symptoms are slow to resolve. For herpes, you may not test positive until an outbreak is active or viral load is high enough. This is why tracking your symptoms and acting early is so important. Testing doesn’t just tell you what’s wrong, it can rule out what’s not, and help your provider choose the right medication.

People are also reading: Yes, You Can Get an STD Without Sex, Here's What to Know
At-Home vs Clinic Testing: What’s the Right Fit?
Let’s say you’re in a small town. The closest urgent care is 40 minutes away, and it’s closed on weekends. Your eye hurts. You feel embarrassed. You’re worried someone will judge you, or worse, not believe you. In these moments, at-home STD test kits can bridge the gap.
While they won’t swab your eye, they can still give you key answers. If your genital or throat swabs come back positive for gonorrhea or chlamydia, your doctor is more likely to treat your eye infection with the right antibiotics. It’s proof. It’s leverage. And it’s private. You test on your terms and bring the results to a provider who can help.
Clinic testing remains the gold standard for eye-specific swabbing. But not everyone has access to clinics, and not every clinic asks the right questions. At-home testing gives you a head start. For many people, that’s the difference between getting treated, or getting ignored.
So You Tested Positive, Now What?
Let’s take the fear out of this: testing positive for an STD doesn’t mean you’re dirty, reckless, or doomed. It means you have information, and information is power. Most STD-related eye infections, especially gonorrhea and chlamydia, are highly treatable with the right antibiotics. But time matters. The longer you wait, the more intense the symptoms can become, and in rare cases, the damage to your vision could be permanent.
The first step is confirming the diagnosis. If you used an at-home test and it came back positive for gonorrhea or chlamydia, bring that result to your provider. Request ocular-specific treatment, often this means oral antibiotics and, in some cases, direct eye drops or ointments. For herpes-related eye infections, antiviral pills like acyclovir or valacyclovir are typically prescribed.
Don’t forget your partner. If they were the source of exposure, they’ll need to get tested and treated as well. This isn’t about blame, it’s about stopping the cycle. Many people carry infections without symptoms and don’t realize they’re spreading them. The eye infection might be your first sign that something deeper is going on in the relationship or body. Facing it head-on is brave. It's also smart.
Check Your STD Status in Minutes
Test at Home with Remedium7-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $129.00 $343.00
For all 7 tests
Your Privacy, Your Power
One of the biggest barriers to getting tested for eye-related STDs is shame. But here’s the thing: eye infections caused by sexual activity aren’t dirty, they’re clinical. They’re preventable, treatable, and manageable. And no one else has to know unless you want them to.
At-home STD tests offer a layer of protection and control that clinic visits don’t always provide. Discreet packaging. No one staring. No awkward conversations in waiting rooms. Just a sample, a few clicks, and an answer. Whether it’s to confirm a suspicion or start a conversation with your doctor, these kits put the timeline in your hands. And when your health is on the line, that kind of control matters.
This at-home combo test kit can help you screen for the most common infections connected to eye symptoms, including gonorrhea, chlamydia, and herpes.
FAQs
1. Can oral sex seriously give you gonorrhea in the eye?
Yep, and it’s not a myth. If someone with an untreated gonorrhea infection gives or receives oral sex and fluids end up near your face, or you touch down there and then rub your eye, it’s enough. The bacteria just needs a mucous membrane. Your eye has one. Boom. Infection.
2. How fast would symptoms show up if that happened?
Fast. We’re talking 1 to 3 days after exposure in many cases. You might wake up thinking it’s allergies, but by day two or three, your eye’s swollen, crusted over, and leaking goo. If it feels like pink eye, but on steroids, it’s time to test.
3. What’s the discharge like with an STD in the eye?
This isn’t your average watery drip. Gonorrhea in the eye usually means yellow-green pus that can literally glue your eyelids shut. If it hurts to blink and you're peeling crust off your lashes every morning? That’s not seasonal allergies.
4. But can’t pink eye just look like that too?
Not really, not to this extreme. Viral pink eye might give you clear tears and a little itch. Bacterial pink eye could have some gunk, sure. But gonorrhea-level discharge is next-level, and it usually comes with pain, swelling, and a red eye that gets worse fast, not better.
5. What if my doctor doesn’t offer an STD test?
Advocate for yourself. Say the words: “I had oral sex recently, and now I have these symptoms. Can you test for gonorrhea and chlamydia?” Many clinics don’t automatically test the eye for STDs unless you ask. Or if you're not comfortable asking yet, use an at-home test to check your throat or genitals first. It's still helpful.
6. Can I test myself at home for an STD in the eye?
Not directly, but indirectly, yes. If you swab your throat or genitals and it comes back positive for something like gonorrhea, that tells your provider your eye issue could be related. Then they can treat it properly. It’s not perfect, but it’s a solid strategy when you're dealing with stigma or no access.
7. Does herpes really spread to your eye from oral sex?
It can. HSV-1 (the cold sore virus) and HSV-2 (typically genital herpes) can both cause eye infections. If your partner has an active outbreak and things get close, mouth to face, mouth to genitals, fluids flying, it can end up in your eye. Herpes there might start mild but can get serious if untreated.
8. Will over-the-counter drops fix this?
Probably not. Regular eye drops might soothe it for a minute, but they won’t kill bacteria like gonorrhea or knock out herpes. If symptoms are strong and not improving in a day or two, or if they’re getting worse, stop guessing and get tested.
9. Is this something I have to tell my partner?
It’s a tough convo, yeah, but yes. If you test positive, they might have the infection too, even with no symptoms. Sharing helps them get treated and helps prevent you both from ping-ponging it back and forth. The good news? More people understand than you think, and some might even thank you.
10. Will I go blind if I wait too long?
In most cases, no. But the risk is real. Gonorrhea in the eye, left untreated, can damage your cornea. Herpes can do long-term damage too. Vision loss isn’t common, but it’s possible. That’s why fast treatment is everything. Don’t wait for it to get scary.
You Deserve Answers, Not Assumptions
If your eye hurts and your instincts are sounding the alarm after a hookup, trust them. You’re not imagining it. You’re not being dramatic. And you’re definitely not alone. STD-related eye infections are underdiagnosed, misunderstood, and often ignored, until someone like you speaks up and demands clarity.
Don’t wait and wonder, get the clarity you deserve. This home test kit checks for the most common STDs quickly and without drawing attention to itself.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate.
Sources
1. CDC: Gonorrhea – Detailed Fact Sheet
2. Gonococcal Infections Among Adolescents and Adults (CDC)
3. Clinical Overview of Pink Eye (Conjunctivitis) (CDC)
4. Gonorrhea - Symptoms and Causes (Mayo Clinic)
5. Sexually transmitted diseases (STDs) - Symptoms and Causes (Mayo Clinic)
6. Chlamydia - Symptoms and Causes (Mayo Clinic)
7. Five-year review of ocular Neisseria gonorrhoeae infections (PMC)
8. Gonococcal conjunctivitis: A case report (PMC)
9. Sexually Transmitted Infections Treatment Guidelines, 2021 (CDC)
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: Dr. Meena Rai, MPH | Last medically reviewed: December 2025
This article is for informational purposes and does not replace medical advice.