Quick Answer: Once collected, your STD sample is labeled, preserved, and sent to a lab. Technicians use specialized tests, like NAATs for chlamydia/gonorrhea, ELISA for HIV, or RPR for syphilis, to detect infection. Results are reviewed for accuracy before being released to you.
The Collection: Where Testing Really Begins
The first step in any STD test is sample collection, and the type of sample depends on what’s being tested for:
- Urine: Common for chlamydia and gonorrhea. Usually requires you to avoid urinating for at least an hour before collection.
- Swab: Used for genital, throat, or rectal testing for bacterial and viral STDs. Can be self-collected or done by a clinician.
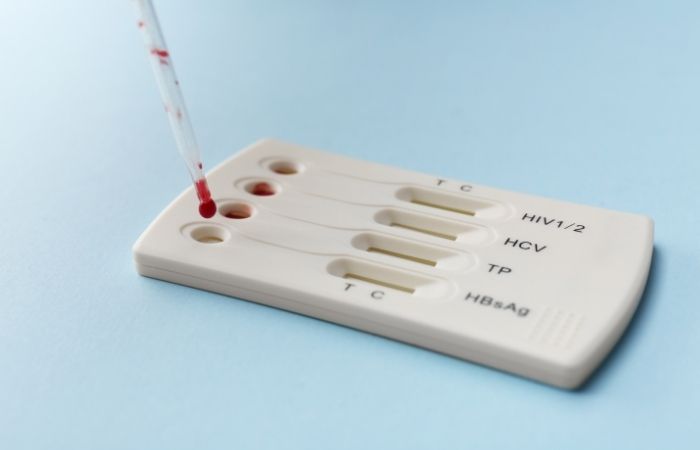
- Blood: Essential for HIV, syphilis, and certain herpes tests. May be a finger prick or a full blood draw.
Whether you collect your sample at home or in a clinic, labeling is critical. Every sample gets a unique identifier, your name might never appear on the lab’s internal forms, especially if you’re testing anonymously, but the code ensures your results match your sample exactly.

People are also reading: The Rash That Won’t Quit: When It’s Not Just an Allergy
From Your Hands to the Courier
Once collected, the sample is sealed in sterile packaging to prevent contamination. For at-home tests, you’ll place it in a pre-paid, temperature-controlled mailer that goes straight to the partner lab. Clinic samples usually head to the lab via daily courier service. Speed matters, especially for swabs and certain blood tests, because bacterial DNA or antibodies can degrade over time.
At the Lab: First Stop – Accessioning
Your sample’s first lab stop is called accessioning. Here, technicians scan the barcode or ID number, log it into the lab’s tracking system, and confirm that the correct type of test has been ordered. They also check for leaks, improper labeling, or damaged containers. If anything is off, say the tube wasn’t sealed or the swab is missing a cap, the lab may request a new sample to ensure accurate results.
Once cleared, the sample is assigned to the right department: molecular diagnostics for NAAT tests, serology for antibody-based tests, or microscopy for certain infections like Trichomonas.
DNA and RNA Testing: The Gold Standard for Many STDs
For infections like chlamydia, gonorrhea, and trichomoniasis, labs use a technique called Nucleic Acid Amplification Testing (NAAT). Here’s how it works:
- The sample, urine or swab, is treated to break open any cells and release genetic material.
- Technicians add special enzymes that replicate targeted bacterial or viral DNA/RNA millions of times.
- If the pathogen’s genetic code is present, the amplification process flags it for detection.
NAAT is highly sensitive, meaning it can detect even tiny amounts of an organism, reducing false negatives. But it’s also so sensitive that contamination during collection or processing can cause a false positive, one reason labs use strict handling protocols.
Check Your STD Status in Minutes
Test at Home with RemediumHepatitis B & Hepatitis C Test Kit
 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $49.00 $98.00
For all 2 tests
Antibody and Antigen Testing
Some infections, like HIV and syphilis, are often detected via blood tests that look for either antibodies (your immune system’s response to infection) or antigens (pieces of the pathogen itself). Common methods include:
- ELISA (Enzyme-Linked Immunosorbent Assay): Detects HIV antibodies and/or p24 antigen to catch infections early.
- RPR/VDRL (Rapid Plasma Reagin/Venereal Disease Research Laboratory): Screens for syphilis by detecting antibodies your body produces in response to infection.
- Confirmatory Tests: Western blot or TP-PA for HIV and syphilis ensure initial results are accurate.
These tests have a “window period” , the time between infection and when the body produces detectable levels of antibodies or antigens. That’s why timing matters when you test.
Quality Control: How Labs Keep Results Accurate
Before any result is released, laboratories run strict quality control measures to make sure the data is reliable. This includes:
- Running control samples alongside patient samples to check that tests are performing correctly.
- Using duplicate testing for borderline results to rule out error.
- Calibrating machines daily and documenting every step for audit purposes.
Accredited labs must follow guidelines from organizations like the Clinical Laboratory Improvement Amendments (CLIA) in the U.S., which set national quality standards for lab testing. This oversight helps ensure that your positive is truly positive, and your negative is truly negative.
Interpreting Results: More Than Just “Positive” or “Negative”
When your results are ready, they’re reviewed by a laboratory scientist or physician before being sent to you or your healthcare provider. Here’s what they might mean:
- Positive: The infection was detected, treatment or further confirmatory testing may be needed.
- Negative: No infection detected at the time of testing. Keep in mind the “window period.”
- Inconclusive/Indeterminate: The test couldn’t confirm either way, often means retesting is advised.
It’s also possible to have a “reactive” result that needs a second test for confirmation, especially for HIV and syphilis. This isn’t a final diagnosis, it’s a flag to double-check.
People are also reading: Syphilis Rash vs. Herpes vs. Eczema: What’s Really on Your Skin?
Window Periods and Retesting
One of the most misunderstood aspects of STD testing is the window period, the time between exposure and when a test can reliably detect infection. For example:
- Chlamydia & Gonorrhea (NAAT): Usually detectable within 5–7 days.
- Syphilis (RPR/VDRL): Detectable within 3–6 weeks after exposure.
- HIV (4th gen ELISA): Detectable within 2–4 weeks for most people, but up to 3 months for some.
- Herpes (PCR or culture): Detectable during an active outbreak; blood tests for antibodies can take weeks to months to show positivity.
Testing too early can lead to false negatives. If you suspect exposure but test negative early, retesting after the full window period is essential.
Case Study: “My First Test Was Negative, But…”
Jared, 29, tested negative for HIV two weeks after a potential exposure. “I felt relieved, but a friend told me to test again after the window period. At six weeks, my test came back positive.” Jared started treatment early, which helped him stay healthy and undetectable.
“If I’d stopped after that first test, I wouldn’t have known, and I might have unknowingly passed it on.”
Jared’s story shows why timing matters just as much as accuracy when it comes to STD testing.
From Lab Back to You: How Results Are Delivered
Once your test results have been confirmed, they’re sent back through the channel you used for testing. For at-home kits, this usually means a secure online portal or encrypted email. For clinic-based tests, results may be delivered in person, via phone call, or through a patient health app. Many clinics offer a “no news is good news” policy for negative results, but you should always confirm your outcome rather than assume.
Positive results often come with counseling or next-step instructions, either treatment plans, prescriptions, or referrals. Some public health departments may reach out directly in the case of certain reportable infections like syphilis, HIV, or gonorrhea to ensure treatment and contact tracing.
Check Your STD Status in Minutes
Test at Home with Remedium3-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $69.00 $147.00
For all 3 tests
Why At-Home and Clinic Results Match (Most of the Time)
FDA-approved at-home STD tests use the same laboratories and technologies as clinics. In fact, many at-home providers partner with the exact same labs your doctor would send a sample to. The main differences are in how samples are collected and shipped. As long as you follow collection instructions carefully, like not urinating before a urine sample or swabbing the correct area, your results will be just as accurate as a clinic’s.
However, in cases of a positive or inconclusive result, it’s always best to confirm with a healthcare provider, especially if treatment will require a prescription.
What to Do If You Test Positive
If your results come back positive, take a deep breath, this is information, not a life sentence. Most STDs are treatable, and many are curable. Here’s your action plan:
- Confirm: If recommended, get a confirmatory test to rule out lab error.
- Treat: Start treatment immediately if prescribed, delaying can make the infection worse.
- Notify Partners: Past and recent partners should be informed so they can get tested and treated if necessary.
- Retest: Follow your provider’s advice on retesting to make sure the infection is gone (for curable STDs) or well-controlled (for chronic ones like herpes or HIV).
Remember: early treatment can often prevent long-term complications and reduce the risk of passing the infection to others.
Avoiding Sample Rejection: Small Steps That Save Big Time
Nothing slows your results like a rejected sample, and it happens more often than you’d think. For urine tests, aim for the first-catch stream and try not to urinate for at least an hour beforehand. For swabs, avoid douching, strong soaps, or applying ointments to lesions right before collection; residue can interfere with detection. For finger-prick blood, warm your hands, hydrate, and let the lancet do the work without milking the finger, which can dilute the sample.
Label everything exactly as instructed and seal it in the provided packaging. Mail or courier it the same day if possible; heat and time can degrade certain targets. If a lab flags an issue, leaky tube, missing cap, wrong medium, don’t panic. Recollecting correctly is better than trusting a compromised result.

People are also reading: Why Monogamy Isn’t a Foolproof Shield Against STDs
False Positives, False Negatives, and “Indeterminate”, Decoded
Tests speak a precise language. A false positive is a rare “detected” when the infection isn’t present, often prevented by confirmatory testing. A false negative is more common early on if you test inside the window period or collect the sample incorrectly. An indeterminate (or “equivocal/reactive”) result means the signal wasn’t strong enough to call; the next step is a different, usually more specific, confirmatory test.
If your result is positive, assume it’s real until a clinician says otherwise, then follow through with treatment and partner notification as advised. If negative but suspicion is high, retest after the full window period. The goal isn’t perfection in one shot, it’s certainty over time, with confirmatory checks when needed.
Cost, Insurance, and Privacy: What to Expect
Clinic testing may be covered by insurance, but check how explanations of benefits (EOBs) are handled if you share a plan and want privacy. Many public health clinics offer low- or no-cost testing. At-home kits provide transparent pricing and discreet shipping; you pay upfront, and your sample goes to certified labs using the same methods as clinics. Positive results for certain infections are reportable to public health, not to shame you, but to connect you with care and protect your community.
If you prefer to stay fully in control, cash-pay and at-home options reduce paper trails while keeping clinical quality. Explore options and pricing through STD Rapid Test Kits, and choose the path that fits your budget, timeline, and privacy needs.
Check Your STD Status in Minutes
Test at Home with Remedium7-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $129.00 $343.00
For all 7 tests
FAQs
1. How long does STD testing take from sample to results?
Most lab tests return results within 2–5 business days, but some rapid tests can give answers in 20 minutes.
2. Do at-home STD tests use the same labs as clinics?
Yes, FDA-approved home kits typically send samples to the same certified labs used by doctors and clinics.
3. Can I eat or drink before giving an STD blood sample?
Yes, STD blood tests do not usually require fasting unless combined with other blood work.
4. What is the most accurate type of STD test?
NAAT (nucleic acid amplification tests) are the gold standard for many bacterial STDs; PCR is highly accurate for viral infections.
5. Can I test for all STDs with one sample?
Some combo tests check for multiple infections from a single urine, swab, or blood draw, but not all STDs can be detected from one type of sample.
6. What happens if my sample is damaged in transit?
The lab will contact you or your provider to request a new sample to ensure accuracy.
7. Why do some results need confirmatory testing?
Borderline or reactive results, especially for HIV and syphilis, are confirmed with a second, different test to rule out false positives.
8. Can I test for STDs the day after unprotected sex?
It’s too early for most tests to detect infection; wait until after the window period for accurate results.
9. Are my STD test results confidential?
Yes, both at-home and clinic-based tests are protected by privacy laws, though some infections must be reported to public health agencies.
10. Can I get treated without going back to the clinic?
Many telehealth services can prescribe treatment after a positive result, and some at-home test providers include treatment options.
Testing Is About Empowerment
From the moment you collect your sample, whether in your bedroom, bathroom, or a clinic, to the moment results arrive, the STD testing process is designed to give you clarity. Every step exists to make sure your results are accurate, confidential, and actionable. Understanding this journey turns testing from something intimidating into something empowering.
If you’re ready to check your status, you can start today with a discreet, FDA-approved Combo STD Home Test Kit, and know exactly what’s happening every step of the way.
Sources
1. CDC , Getting Tested for HIV (Types of Tests & Windows)
2. CDC , Chlamydial Infections: STI Treatment Guidelines (NAAT specimen types)
3. MedlinePlus , HIV Viral Load Test (NAAT/PCR overview)










