Quick Answer: Chlamydia is often misdiagnosed as a UTI, especially in women. If you have UTI-like symptoms but your test is negative or the infection keeps coming back, ask for an STD test, chlamydia is treatable, but only if caught.
It Starts With a Burn: How Symptoms Blur the Lines
Most people think they know what a UTI feels like: burning, frequent urination, pelvic pressure. But here’s the truth, chlamydia can feel exactly the same. In fact, for many women, the early symptoms of both infections are nearly identical. And even worse? About 70% of women with chlamydia show no symptoms at all, or symptoms so mild they’re dismissed as irritation or stress-related discomfort according to the CDC.
Because of this overlap, and because primary care providers often default to assuming urinary tract infections, thousands of women are treated with antibiotics for a problem they don’t actually have. If that antibiotic doesn’t happen to also treat chlamydia (some do, some don’t), the STD keeps thriving unnoticed.
In Delaware, a state with rising STD rates but inconsistent testing protocols, this is more than an inconvenience, it’s a public health emergency in disguise.

People are also reading: Can You Get an STD from an Animal? What the Science Says About Bestiality and Risk
Why Delaware? Unpacking the Geographic and Gender Risk
Delaware consistently ranks in the top 15 states for chlamydia infection rates per capita, with disproportionately high rates among young women aged 15–29. Yet according to state health reports, only about half of women in this age group are ever tested unless they’re pregnant or request it outright.
This is where misdiagnosis takes root. In places like Wilmington, Dover, and Newark, community health centers often treat UTI symptoms based on quick urine strips, which can’t detect STDs. Unless a provider suspects chlamydia, or unless the patient asks, it’s never tested. Even emergency rooms in Kent County have reported trends where presumptive UTI treatment goes unchecked by STD screening.
Combine that with the stigma around STDs, and many women don’t push back. They assume their pain is “just another UTI” and move on, until it gets worse.
| Symptom | Chlamydia | UTI |
|---|---|---|
| Burning with urination | Yes | Yes |
| Frequent urination | Sometimes | Yes |
| Pelvic pain or pressure | Yes | Yes |
| Vaginal discharge | Common | No |
| Blood in urine | Rare | Possible |
| Asymptomatic presentation | 70%+ of cases | Rare |
Figure 1. Symptom overlap between chlamydia and UTI causes confusion in diagnosis, especially in non-specialist settings.
“I Kept Getting Treated for the Wrong Thing” , A Case Out of Newark
Maria, 24, from Newark, DE, had been in a monogamous relationship for over a year when she started experiencing burning during urination and lower back pain. She went to urgent care and was diagnosed with a UTI. Two weeks later, the symptoms returned. Another UTI diagnosis. Then another.
“By the third time, I started Googling ‘UTI won’t go away STD?’ That’s how I found out about chlamydia. I went back and asked for an STD test, and it was positive.”
Maria’s story is echoed across community health clinics throughout Delaware. Women, particularly women of color, are dismissed, under-tested, or not offered screening unless they insist. According to a 2023 study published in the journal Sexually Transmitted Diseases, nearly 40% of women who tested positive for chlamydia had initially been treated for a UTI within the previous 6 months.
Misdiagnosis delays treatment. Delayed treatment leads to pelvic inflammatory disease (PID). PID leads to scarring, infertility, and ectopic pregnancy risk. And it all starts with a single missed test.
When a UTI Isn’t a UTI: The Problem With Pee Cup Diagnostics
Walk into any urgent care clinic with burning pee, and chances are they’ll hand you a plastic cup. The assumption? It’s a bladder infection. The problem? That cup can’t test for chlamydia.
Urine dipsticks and standard urinalysis only screen for bacteria in the urinary tract, typically E. coli or other common UTI pathogens. But chlamydia doesn’t always show up in the urine in the same way. Unless a provider orders a specific NAAT (nucleic acid amplification test) for chlamydia or gonorrhea, your sample won’t be screened for either infection, even though it uses the same cup.
So you could walk away thinking you’re “clean,” when in fact the test didn’t even check. And if the UTI test is negative but the symptoms persist, many providers simply prescribe antibiotics “just in case,” rather than ordering an STD screen.
| Test Type | Detects Chlamydia? | Use Case |
|---|---|---|
| Urine Dipstick | No | Fast UTI screening, not STD testing |
| Urinalysis (lab) | No | Checks white blood cells, bacteria, but not STDs |
| NAAT (Chlamydia Test) | Yes | Detects bacterial DNA from chlamydia; gold standard test |
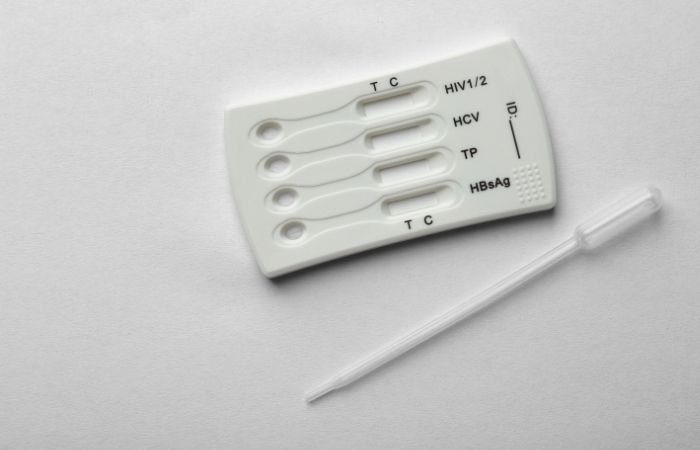
| At-Home Chlamydia Rapid Test | Yes | Screens at home; confirmatory testing may still be needed |
Figure 2. Most “urine tests” only screen for UTIs unless a chlamydia-specific test is requested.
This diagnostic blind spot is one of the biggest reasons why chlamydia continues to be the most reported STD in the U.S., and yet still goes undiagnosed in many women until damage has already occurred.
Delaware’s Discreet Testing Gap , And How to Fix It
Many Delaware residents, especially in lower-income areas like Sussex and Kent counties, face barriers to full STD screening. These include long waits at clinics, transportation issues, and lack of awareness about at-home testing options. But what’s most dangerous is the false confidence that comes from a UTI test that never looked for STDs in the first place.
Here’s the kicker: NAAT tests can be run from the same urine sample as a UTI test, but you have to ask. And most providers won’t offer unless you bring it up.
For those in areas without easy clinic access, an at-home chlamydia rapid test offers privacy, speed, and empowerment. While confirmatory testing is still advised in some cases, many women prefer starting with a private screen before escalating to a clinic visit.
If your UTI symptoms return or don’t improve, or if your tests keep coming back “clean” but something still feels off, it’s time to test for something else.
Check Your STD Status in Minutes
Test at Home with RemediumChlamydia Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $33.99 $49.00
Symptoms That Should Trigger an STD Test (But Often Don’t)
While not all UTIs are chlamydia, and not all chlamydia causes symptoms, there are certain red flags that should prompt an immediate STD screen. Sadly, these often go overlooked, especially when providers are rushing or patients are too embarrassed to ask.
Here are some examples, based on real patterns observed in Delaware clinics and supported by national CDC guidelines:
- Frequent UTIs with no clear bacterial cause (especially in sexually active women under 30)
- Burning urination plus abnormal vaginal discharge
- Pain during sex or bleeding after (often misattributed to irritation or stress)
- Negative UTI test with persistent symptoms
- Recurrent “UTIs” that don’t respond to standard antibiotics
In all these cases, a basic urine screen won’t be enough. A full STD panel or a targeted chlamydia test is necessary.
Don’t wait and wonder. If something feels off, or if you’ve been treated for a UTI more than twice in one year, get an STD test. Your health depends on it, and it’s easier, faster, and more private than ever.
What Happens When Chlamydia Goes Untreated
When chlamydia is caught early, it’s simple: a round of antibiotics and a brief partner conversation. But when it’s misdiagnosed or missed entirely, as it often is when mistaken for a UTI, the story gets darker.
Untreated chlamydia can silently ascend from the cervix into the uterus and fallopian tubes, leading to pelvic inflammatory disease (PID). PID causes scarring and inflammation that can result in chronic pain, infertility, or ectopic pregnancy. The longer the infection sits undetected, the greater the risk. According to the CDC, up to 10–15% of untreated cases in women lead to PID.
Here’s what that progression can look like:
Step 1: Burning urination misdiagnosed as a UTI → antibiotics that don’t treat chlamydia
Step 2: Symptoms return or shift → discomfort during sex, unusual discharge, or spotting
Step 3: Internal infection spreads silently → inflammation of reproductive organs
Step 4: Diagnosis delayed until damage is done → fertility risk, chronic pelvic pain, partner reinfection
These aren't rare outliers, they're everyday stories from urgent care clinics in Wilmington, Smyrna, and beyond.
How to Talk to Providers When You're Afraid to Ask
Let’s be honest: many people, especially young women, don’t feel comfortable saying “Can I get tested for STDs?” during a rushed doctor’s visit. The stigma is still real. So here’s a script you can use without shame or fear:
“I’ve been having symptoms that seem like a UTI, but I’ve read that sometimes chlamydia can cause similar issues. Can you add a chlamydia test to my urine sample?”
That one sentence can shift the entire direction of your care. Most providers will say yes. Some may still resist, but you’re allowed to insist. And if you don’t feel safe or seen, you can always order a combo STD test kit and test privately from home.
Remember, testing is self-care, not confession. It’s not about who you’ve slept with or how often. It’s about knowing your body and getting answers when something feels off.
People are also reading: Burning When You Pee but No UTI? It Could Be Gonorrhea
Take Control Before the System Lets You Down
If you're reading this from a small Delaware town or scrolling at 2AM because something doesn't feel right, know this: you’re not being dramatic. Your pain is real. Your questions are valid. And you deserve better than rushed assumptions about what’s going on in your body.
You don’t have to wait weeks for a clinic appointment. You don’t need to beg for tests. You can order an STD test online, test from home in total privacy, and get clear results in minutes.
Whether it’s a stubborn burn or just a hunch, peace of mind is one test away.
Chlamydia Isn’t Just a “Teen Problem” , And UTI Misdiagnosis Doesn’t Discriminate
While chlamydia is most common among women aged 15–24, it doesn’t magically stop after college. Many Delaware women in their 30s and 40s experience recurrent UTI symptoms that never seem to clear, only to learn later that they’ve had an asymptomatic STD for years.
Providers may be more likely to screen younger women for STDs, but they often overlook the risk in older, partnered, or married patients. That’s part of the systemic failure. Anyone who is sexually active is at risk. And anyone with symptoms deserves real answers, not assumptions.
Especially if your UTI tests keep coming back negative, it’s time to rule out other causes. Chlamydia is common, curable, and best caught early. Don’t let a delay turn into a deeper issue.
FAQs
1. Can chlamydia really feel like a UTI?
Yep, and that’s the trap. The burning, the pressure, the constant need to pee? Chlamydia can hit all those notes. That’s why so many people walk out of urgent care with a UTI diagnosis when it’s actually an STD. The only way to tell for sure? Ask for a test that actually checks.
2. I had a UTI test, and it was negative... so why does it still burn when I pee?
Because not all burning is bladder-related. A negative UTI test that leaves you feeling the same (or worse) should be a giant neon sign to test for chlamydia or gonorrhea. Some infections don’t play by the rules, and they don’t show up unless you’re testing for the right thing.
3. How do I even ask my doctor for an STD test without it being awkward?
Try this: “Can you check for STDs too, just in case?” That’s it. No apology, no shame. If you're being seen for pee pain, weird discharge, or a UTI that won’t quit, this is totally normal to ask. If it still feels weird, remember: you can test yourself at home. Privacy wins.
4. Is it possible I’ve had chlamydia for months and didn’t know?
Unfortunately, yes. Chlamydia can simmer silently for weeks or even years. You could feel completely fine, or just “off” enough to ignore. That’s why it's often called the “silent” infection. If you’re in doubt, especially with a partner change or recurring symptoms, it's better to test and know.
5. Do all antibiotics for UTIs work on chlamydia?
Not even close. Some do double duty, but many don’t. If your doc prescribed nitrofurantoin (Macrobid) or something similar, it likely won't touch chlamydia. And if you did have it, the infection could still be quietly doing damage.
6. What if I’m in a committed relationship, could I still have chlamydia?
Look, relationships are complicated. STDs don’t just show up because someone cheated. Sometimes infections stick around from before the relationship started. Or someone didn’t know they had it. It's about biology, not blame. Test, talk, and move forward with clarity.
7. Can I just use an at-home test instead of going to a clinic?
100%. If you'd rather skip the awkward waiting room vibes or want privacy, at-home chlamydia test kits are a legit, FDA-approved option. They’re fast, discreet, and surprisingly easy to use.
8. How fast can chlamydia mess with my fertility?
Scary fast. Left untreated, chlamydia can lead to PID in a matter of weeks or months, and that’s what causes long-term damage. The good news? Early detection = no damage. That’s why testing at the first hint of weirdness matters so much.
9. What if I already took antibiotics and now I feel better, do I still need to test?
Maybe. If you took antibiotics that treat chlamydia and your symptoms went away, that’s great, but you should still test to confirm it’s really gone. And if your partner didn’t get treated too, you could get reinfected. Always better to test than guess.
10. How often should I be testing for STDs, really?
Think of it like dental cleanings, but for your sexual health. Once a year if you’re monogamous. Every 3–6 months if you have new partners, symptoms, or you just like peace of mind. And every time something feels “off.” Your gut is usually right.
You Deserve Answers, Not Assumptions
If you’ve been treated for a UTI but something still feels off, or if you’ve never been offered an STD test despite recurring symptoms, it’s time to take your health into your own hands. Delaware women are being overlooked, misdiagnosed, and delayed access to real care. That ends with awareness, and action.
Chlamydia is common. Testing is simple. And you don’t need permission to take the next step.
Don’t wait and wonder, get the clarity you deserve. This at-home combo test kit checks for the most common STDs discreetly and quickly.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted some of the most relevant and reader-friendly sources.
Sources
1. Planned Parenthood – What Is Chlamydia?
3. NHS – Chlamydia Overview and Symptoms
5. In ERs, UTIs and STIs in women misdiagnosed nearly half the time — ScienceDaily
6. Potential delayed and/or missed STI diagnoses due to misclassification as UTIs — 2023 Study
About the Author
Dr. F. David, MD is a board-certified infectious disease doctor who specializes in preventing, diagnosing, and treating STIs. He is dedicated to making his work available to more people, whether they live in cities or off the grid. He combines clinical accuracy with a straightforward, sex-positive approach.
Reviewed by: Elise Tran, FNP-BC | Last medically reviewed: December 2025










