Quick Answer: Most standard STD panels don’t include tests for herpes, HPV, trichomoniasis, or oral/anal infections unless you specifically request them. To get truly tested for “everything,” you need to ask for these by name.
Who This Article Is For
This is for the person who left urgent care last week with a neat little lab report that made them feel relieved, but something still feels off. It’s for the person who slept with a new partner and got “tested for peace of mind,” only to find out later that one burning question wasn’t answered. It’s for the woman whose OB-GYN only tested her for chlamydia and gonorrhea during a Pap smear, and the guy whose doctor said “you're fine” without swabbing or drawing blood at all.
If you’ve ever assumed your routine screening was complete, this article is for you. We’ll walk you through exactly what most clinics and labs test for, what they usually leave out, why it matters, and how to make sure you’re actually covered next time. It’s not about paranoia, it’s about knowledge and consent.
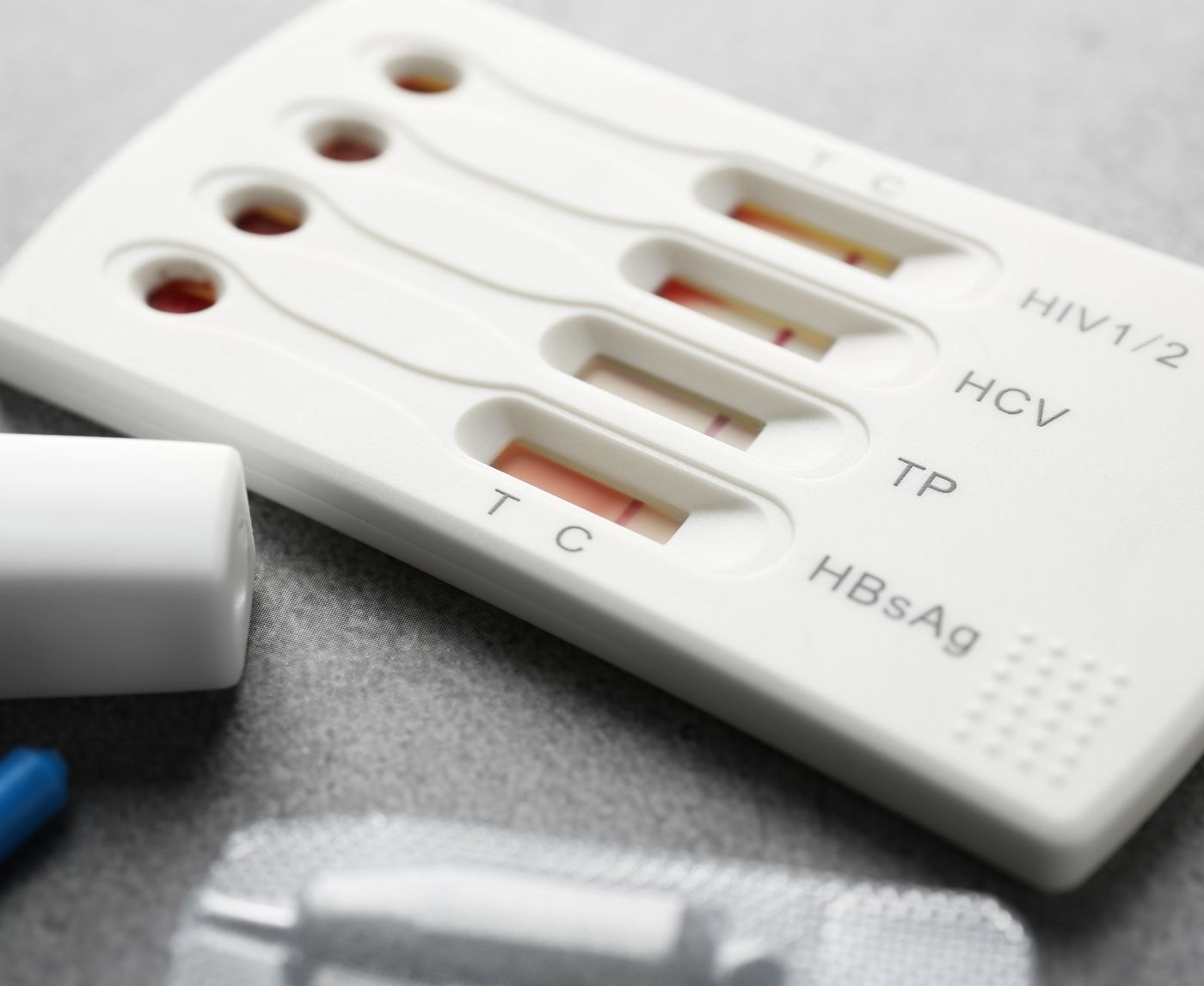
What's Actually Included in a “Standard” STD Test?
There is no single definition of a “standard” STD test panel. Some clinics offer a “basic” screen, others call it a “complete panel,” and urgent care centers often bundle a few common infections together and call it a day. But unless you ask or read the fine print, you likely won’t know what’s being tested, and what’s not.
Here's how it typically breaks down:
| STD | Usually Included? | Test Type | Sample |
|---|---|---|---|
| Chlamydia | ✔ Yes | NAAT | Urine or swab |
| Gonorrhea | ✔ Yes | NAAT | Urine or swab |
| Syphilis | ✔ Often | Antibody (RPR) | Blood |
| HIV | ✔ Often | Antigen/Antibody combo | Blood |
| Herpes (HSV-1/2) | ✖ Rarely | Antibody or PCR (if sores) | Blood or swab |
| HPV | ✖ Rarely | Pap + HPV DNA (cervical only) | Cervical swab |
| Trichomoniasis | ✖ Rarely | NAAT or rapid antigen | Swab or urine |
Table 1: What’s usually included in a “standard” STD panel, and what’s often skipped.
This is where so many people get caught off guard. If your symptoms don't match a textbook description, or if you didn’t specifically request herpes or trichomoniasis testing, it’s very likely those were never run. And unless you're a woman getting a Pap smear, HPV may not be mentioned at all, even though it's one of the most common STIs on the planet.
People are also reading: From Oral Sex to Cancer: The Silent Danger of HPV in Men
What Gets Missed, and Why It Matters
Let’s talk about herpes for a moment. It’s arguably the most misunderstood STD in terms of testing. Many clinics, including Planned Parenthood and the CDC, do not recommend routine herpes screening for people without symptoms, because false positives are common and the emotional toll can outweigh clinical benefit. But here’s what patients hear: “You’re all clear.”
Sarah, 26, went in for a full panel before sleeping with her long-distance partner. Everything came back negative. Nine months later, after painful sores and a gutting trip to the ER, she tested positive for HSV-2. Her original doctor had never offered the test. “I wouldn’t have cared if it was routine or not,” she said. “I just wanted to know. I thought I was being responsible.”
Trichomoniasis is another stealth infection. Especially common in women, trich often causes no symptoms but can increase your risk of HIV transmission and other pelvic infections. Yet unless you request a vaginal swab or NAAT, it’s unlikely to be caught. In men, it’s rarely tested for at all.
And then there’s HPV. Unless you’re a woman between 30 and 65 getting co-testing during a cervical Pap smear, it’s likely no one tested you for it. Men aren't routinely screened, even though they can carry and transmit high-risk strains linked to cancers of the penis, anus, and throat.
The consequences of missed infections aren’t just personal, they’re communal. Every partner you sleep with inherits your testing gaps. Every negative result you share could be unintentionally misleading.
Case Study: “They Told Me I Was Clean. I Wasn’t.”
Andre, 32, had always been cautious. He got tested regularly at a local clinic, especially before starting something new. “They said it was a full panel. That’s what I paid for.” But after months of being with a partner who started having recurrent yeast infections and discomfort, she got tested on her own and came back positive for trichomoniasis. “She was devastated. I was confused. I went back to the clinic, and they admitted they never tested me for trich. They didn’t even have it in the panel.”
This isn’t rare. It’s not negligence, it’s the norm in many healthcare settings where time, insurance codes, and assumed low risk drive decision-making. Unless your provider has a reason to suspect a specific infection, they may not offer testing at all. And unless you ask, you’re trusting that “standard” means “complete.”
Andre now tells his friends to ask specifically for trich, herpes, and anything that isn’t just pee-in-a-cup. “I thought I was doing everything right. But right isn’t enough if you don’t know what to ask for.”
Check Your STD Status in Minutes
Test at Home with Remedium6-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $119.00 $294.00
For all 6 tests
What You Need to Ask For, By Name
Let’s make this part painfully clear: if you want full coverage, you need to ask for specific tests. Not just “an STD panel,” not just “a clean bill.” Use the actual names. And say them out loud.
This isn't about mistrusting your provider, it’s about taking ownership of your care in a system that’s often overburdened, rushed, or coded for the lowest common denominator of testing. Asking doesn’t mean you think you’re infected. It means you understand how risk works. It means you respect your partners, and yourself.
Here’s a narrative-style breakdown of what to request, and how each one is typically handled:
| Test to Request | Why It’s Skipped | How to Ask |
|---|---|---|
| Herpes (HSV-1 & HSV-2) | Not recommended without symptoms due to false positives | “Can you add herpes testing to my panel, even if I don’t have symptoms?” |
| Trichomoniasis | Not part of standard male testing; often missed in women | “Can I get tested for trichomoniasis with a vaginal swab or NAAT?” |
| HPV (High-risk strains) | Not routinely tested in men; only co-tested during cervical Pap in some women | “Am I due for HPV co-testing with my Pap smear?” (women only) |
| Syphilis | Sometimes omitted in low-risk profiles | “Please include syphilis in my blood work.” |
| HIV (4th Gen or NAAT) | Opt-in in many places; rapid tests may be 2nd gen | “Is this the 4th generation HIV test that checks for early infection?” |
Table 2: Tests you should ask for directly, what they miss and how to request them clearly.
That awkward moment at the doctor’s office when you fumble for words? It’s easier than dealing with a missed diagnosis months later. If you’re at a walk-in or using an at-home service, check exactly what the kit includes, and choose a combo test kit if you’re unsure. It’s better to slightly over-test than to walk away with a false sense of security.
Anatomy Matters: Why “Negative” Isn’t Always Accurate
One of the most common gaps in STD testing happens when people assume one sample equals full-body screening. But oral, genital, and rectal infections each require their own swabs. A negative urine test for chlamydia doesn’t rule out a throat infection from oral sex. A vaginal swab won’t detect rectal gonorrhea in someone who had anal exposure.
Here’s a scene we’ve heard again and again: someone walks into a clinic, says they want to “get tested,” gives a urine sample, and leaves thinking they’re good. But if they gave or received oral sex, or had anal play, that test missed huge potential exposure zones.
Jay, 29, identifies as a gay man and got a rapid test panel before traveling. “It was just a finger prick and pee sample,” he said. “They didn’t swab my throat or ask about anal. I thought that was weird. I asked, and the nurse said, ‘Oh, we only do that if you have symptoms.’”
That same panel missed a rectal gonorrhea infection that only showed up after his partner developed symptoms weeks later. “Now I know to be way more specific. I tell them what I’ve done, and ask to be swabbed in every area I’ve had exposure.”
STD testing isn’t one-size-fits-all. It's anatomy-aware. And if your provider doesn’t ask where you’ve had sex, you need to speak up.
The Role of Window Periods: When Timing Tricks the Test
Even when the right tests are ordered, there’s another sneaky way results can be misleading: testing too early. Every infection has a “window period”, the time between exposure and when a test can reliably detect it. Testing before that window closes can lead to false negatives. And for people who test immediately after a scare, this is a common trap.
Below is a quick-reference table that outlines when different infections show up on tests, and when retesting may be necessary.
| STD | Minimum Detection Time | Optimal Testing Window | Retesting Needed? |
|---|---|---|---|
| Chlamydia | 7 days | 14+ days | If exposed again |
| Gonorrhea | 5–7 days | 10–14 days | If symptoms persist |
| Syphilis | 3 weeks | 6–12 weeks | Yes, if tested early |
| HIV (4th Gen) | 2 weeks | 4–6 weeks | Yes, if tested <4 weeks |
| Herpes | 3–6 weeks (antibody) | 12–16 weeks | Yes, unless outbreak present |
| Trichomoniasis | 5 days | 2+ weeks | If symptoms occur or partner positive |
Table 3: Window periods and retesting needs. Early testing is not wrong, but it often needs to be followed by confirmatory testing later on.
Timing doesn’t just affect accuracy, it affects your sense of peace. One negative test too soon can lull someone into unsafe behavior or stop a conversation that needs to happen. The emotional cost of premature testing is real. Better to test once now, again at the right interval, and be sure.
If you’re feeling unsure, STD Rapid Test Kits offers confidential, retest-ready options that fit these windows, without the clinic awkwardness.
At-Home Tests vs Clinic Panels: Not All Gaps Are Clinical
There’s a growing assumption that at-home STD tests are inherently less accurate than clinic-based ones. That’s not always true. Many at-home tests use the same labs, same sample collection methods (like urine or blood drops), and same NAAT testing protocols. The real difference often comes down to user error, timing, and what's actually included in the kit.
Let’s look at two very real but very different situations:
Mira, 24, used an at-home kit after a condom broke. The kit included tests for chlamydia, gonorrhea, HIV, and syphilis, but not herpes or trich. She assumed those were included. “It was my fault,” she says. “I didn’t check the panel closely. I just assumed ‘STD test’ meant everything.”
Tyrese, 37, went to a walk-in clinic. He was told to pee in a cup, and five days later he got a text saying he was all clear. No one took blood. No one swabbed his mouth. “It was fast and easy, which I liked,” he recalls, “but now I wonder if it was too easy.”
Both cases reflect the same issue: it’s not just about where you test. It’s about what’s being tested and how thoroughly. A negative result only means you’re negative for the things they actually checked.
Some rapid at-home kits offer broader panels than clinics do, especially combo kits that include trich and herpes options. But always read the fine print. The safest option is to choose a reputable, verified kit that clearly lists each infection covered. If you're uncertain, the Combo STD Home Test Kit covers the most commonly missed infections and includes easy-to-follow instructions for sample collection.

People are also reading: Got a Positive STD Test? Here’s What Doesn’t Happen Next
False Negatives, False Peace of Mind
One of the most painful dynamics in sexual health is false peace of mind. Someone takes a test, maybe too early, maybe for the wrong infections, maybe without the right sample, and walks away feeling clear. They share that confidence with a new partner. And that confidence becomes contagious. But it was never real.
Lex, 31, tested after a one-night stand that left them uneasy. “I did the responsible thing. I went to a pharmacy clinic the next day, got tested, and they said I was negative.” But the test was too soon for HIV, too narrow to include herpes, and didn’t address Lex’s anal exposure. “I kept seeing that guy. A month later, I tested positive for HSV-2. I felt betrayed, by the clinic, by myself. I’d done everything I thought I was supposed to.”
This is where trauma creeps in, not from the diagnosis, but from the emotional whiplash of going from “you’re fine” to “you missed something big.” It’s why transparency in testing matters. It's why we can’t treat the words “STD panel” as a guarantee. It's why we need to normalize asking for specifics without shame.
And it’s why retesting matters. One test isn't always enough, especially if it happened early after exposure, didn’t cover all potential infections, or if a partner tested positive later.
Check Your STD Status in Minutes
Test at Home with Remedium8-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $149.00 $392.00
For all 8 tests
Should You Retest? Here’s When and Why
Retesting isn't paranoia, it’s process. It's part of how medical science accounts for incubation windows, variable immune responses, and the natural evolution of detectable infection markers. And it’s how we avoid turning false negatives into false confidence.
So when should you retest?
If you tested within a week of exposure, plan to test again at the 2–4 week mark, and again at 3 months if concerned about HIV or herpes. If you tested for only a few infections and not a full panel, retesting can help fill those gaps. And if a new partner comes forward with a diagnosis, retesting is essential, regardless of your last result.
Dee, 41, had a partner disclose a past chlamydia infection. She tested negative two weeks later, but still had occasional discharge and discomfort. Her provider said it was probably nothing. Two months later, she retested with a mail-in kit that included trich, and finally got an answer. “It wasn’t chlamydia. It was trich the whole time. My provider never even mentioned that one. If I hadn’t retested, I’d still be guessing.”
If your gut says something’s off, listen to it. You know your body better than any algorithm or checklist. And testing again isn't about being dramatic, it’s about closing the loop. You can browse discreet options at STD Rapid Test Kits, especially if you need to cover less common infections like trichomoniasis or herpes.
Retesting is clarity. It’s care. It’s self-respect.
FAQs
1. Wait, why wouldn’t they test for herpes automatically?
Because herpes is messy, for labs and for emotions. Unless you have symptoms, many clinics skip it. That’s partly because antibody tests can’t tell when you got it, and false positives are a thing. But here’s the rub: it still matters. If you want to know, ask for it. Your peace of mind is worth more than a lab’s convenience.
2. Can I really have an STD in my throat or butt and not know it?
Absolutely. And here’s the wild part, most “standard” tests won’t catch those unless you specifically ask for oral or rectal swabs. Had unprotected oral or anal sex? Say it out loud to your provider. This isn’t the time to be polite or vague. They can't test what they don't swab.
3. I peed in a cup, doesn’t that cover everything?
Nope. Pee tests are great for chlamydia and gonorrhea in the urethra, but that’s about it. If you’ve had other kinds of sex, oral, anal, shared toys, you need swabs or bloodwork too. The “one cup to rule them all” idea? Total myth.
4. My test said I was negative. Why do I still feel off?
Testing too soon, testing for the wrong thing, or not testing the right body part, any of these can throw off your results. You might also have a non-STD issue, like BV or a yeast infection. But if something’s still bugging you, trust that instinct. Retest, ask for more, or switch providers. You’re allowed to keep pushing for answers.
5. How do I ask for a full panel without sounding “extra”?
You don’t sound extra, you sound educated. Try: “I want to be tested for herpes, trichomoniasis, syphilis, HIV, and HPV if that applies. Also, I’ve had oral and anal sex, so I’d like swabs for those areas too.” Anyone who makes you feel awkward for saying that doesn’t deserve your business or your body.
6. Can I use an at-home test instead of going to a clinic?
Yes, and for many people, it’s the better option. At-home kits let you test privately, on your timeline, without the side-eye or small talk. Just make sure the kit you choose tests for everything you need, and that it includes swabs or blood tests if needed. We’ve got discreet combo kits that cover the hard-to-catch stuff too.
7. What’s the deal with trich? No one talks about it.
Exactly, no one talks about it, which is why it gets missed. Trichomoniasis is a super common vaginal infection that often has zero symptoms. It rarely gets tested for unless you ask. And yes, guys can carry it too, even though it’s harder to detect. Silent, spreadable, and sneaky.
8. Should I really get tested again if I just did last week?
If your last test was too soon after exposure, or skipped important STDs, yes. Retesting isn’t overkill; it’s common sense. Think of it like checking the weather again before a trip. Situations change, and so does your risk profile.
9. I’m in a monogamous relationship. Do I still need to test?
If you both tested after your last partners and you’re truly exclusive, you're probably good. But if monogamy is assumed rather than discussed, or it’s a new relationship, it’s smart to test. STDs can hang out undetected for a while, especially if you didn’t get a full panel last time.
10. Is it okay to test just for peace of mind?
Hell yes. You don’t need a burning sensation or a suspicious rash to justify getting tested. Testing is care. Testing is love, for yourself and your partners. Even if it all comes back negative, you’ve taken control of your story. That matters.
You Deserve Answers, Not Assumptions
No one should walk away from STD testing with a false sense of safety. Not because they were irresponsible, but because they didn’t know what to ask for. And that’s not your fault. The system is confusing, inconsistent, and often designed around insurance codes, not real-world sex lives.
But you don’t have to stay in the dark. You can name the infections. You can ask for the right swabs. You can check the test menu before you hand over your sample. And you can retest if something still feels off.
Don’t wait and wonder, get the clarity you deserve. This at-home combo test kit checks for the most commonly missed STDs discreetly and quickly.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate.
Sources
1. CDC – STD Screening Recommendations
2. Which STI tests should I get? – CDC
3. STI Screening Recommendations – CDC
4. Know the Facts About STI Testing – CDC
5. Sexually Transmitted Infections Treatment Guidelines, 2021 – CDC
6. STI and HIV Infection Risk Assessment – CDC
7. Sexually Transmitted Diseases (STDs) – Mayo Clinic
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist who works to stop, diagnose, and treat STIs. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: Angela M., RN, MPH | Last medically reviewed: January 2026
This article is meant to give information and should not be taken as medical advice.