Quick Answer: You can get an STD through skin-to-skin contact, oral sex, genital rubbing, and shared sex toys, even if there's no vaginal or anal penetration. Protection still matters, and testing is essential.
Why "No Sex" Doesn’t Mean "No Risk"
Let’s start with the obvious: people define sex differently. For some, it only “counts” if there’s penetration. For others, oral sex, mutual masturbation, or even dry humping cross that line. But when it comes to STD transmission, viruses and bacteria don’t care how you label the act. What matters is contact, skin, fluids, mucous membranes, and microscopic breaks in the skin.
HPV, for example, is so contagious that even brief genital-to-genital contact without penetration can pass it along. Herpes simplex virus can spread through oral-to-genital contact or even kissing, depending on the strain. And chlamydia has been documented spreading via shared sex toys or fingers moving between partners without proper hygiene in between. So yes, “virgins” can absolutely get STDs. The body doesn’t care if you feel innocent. Microbes don’t recognize social rules.
This misconception, that you're safe if you haven't had “real” sex, causes too many people to skip testing. It’s not your fault. The sex ed most people receive either ignores this entirely or focuses exclusively on vaginal intercourse. But your risk doesn’t start and stop at penetration. It starts with closeness, moisture, and biology.
Case Study: “I Thought I Was Safe Because I Was a Virgin”
Layla, 18, had been careful her entire life. She grew up in a conservative household where virginity was sacred. She and her first boyfriend decided to “do everything but.” That meant lots of oral, some dry humping without clothes, and one shared toy they cleaned with baby wipes.
“I tested positive for chlamydia during a routine check before college. I was horrified. I hadn’t even had sex. I didn’t know what to tell my parents, or even how it was possible.”
Layla’s case isn’t rare. Shared sex toys, unwashed hands, and mouth-to-genital contact are all common ways for bacteria to transfer. If the toy was used vaginally on her boyfriend and then inside her, without proper sterilization, it’s enough. One careless moment doesn’t mean she did anything wrong. But it does mean that testing and protection matter, no matter how you define your intimacy.

People are also reading: Anal Herpes: The STD No One Talks About
How STDs Actually Spread Without Intercourse
To understand how this happens, we need to get into the biology. The surface of your genitals, mouth, and anus are made of delicate tissue that can easily absorb viruses or bacteria. Even without visible cuts or breaks, microscopic tears can let microbes in. Combine that with fluids, saliva, semen, vaginal secretions, and you’ve got a recipe for transmission.
Here’s where it gets real: even kissing can spread oral herpes. Even mutual masturbation can pass HPV or herpes if hands go from one person to another without being washed. If a sex toy isn’t sanitized, or if it’s used on both partners without a condom, it becomes a bacterial bridge. And if you're receiving or giving oral sex, you're vulnerable to gonorrhea, syphilis, chlamydia, and even HIV in rare cases.
Let’s break that down more clearly.
| Transmission Method | Possible STDs | Notes |
|---|---|---|
| Oral sex (giving or receiving) | Herpes, HPV, Gonorrhea, Syphilis, Chlamydia | Can infect throat, genitals, or anus. Often symptomless. |
| Genital-to-genital rubbing (no penetration) | HPV, Herpes, Syphilis | Skin-to-skin contact spreads viral STDs. |
| Shared sex toys | Chlamydia, Gonorrhea, HIV | Use condoms on toys and clean thoroughly between uses. |
| Kissing | Herpes (HSV-1), Mono | Cold sores = active herpes virus. |
| Hand-to-genital contact (fingering) | HPV, Herpes (rarely), Chlamydia (very rarely) | Risk increases if fingers contact fluids and switch partners. |
Table 1: Common ways STDs spread without vaginal or anal intercourse. This isn’t about paranoia, it’s about prevention.
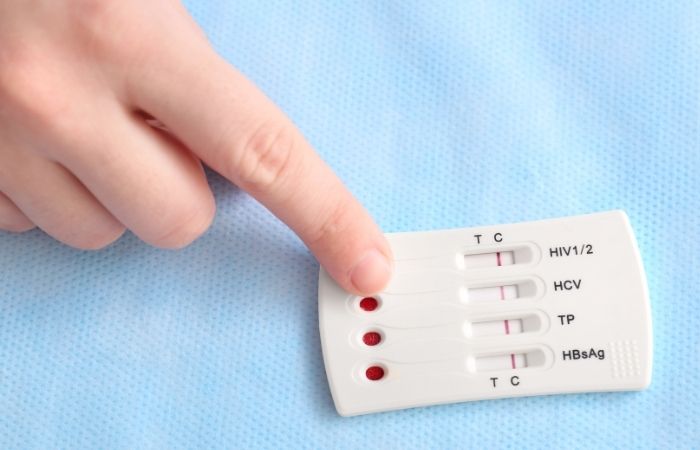
Order Now $129.00 $343.00 Check Your STD Status in Minutes
Test at Home with Remedium
7-in-1 STD Test Kit




For all 7 tests
The STD Most Likely to Be Misunderstood: HPV
If there’s one infection that truly doesn’t care about penetration, it’s Human Papillomavirus (HPV). It can live on the skin of the genitals, anus, and mouth, and most people don’t know they have it. It spreads through skin-to-skin contact and has no symptoms for many carriers. Condoms lower the risk, but they don’t eliminate it. Anything uncovered is fair game.
This is especially important for people who identify as queer, trans, or nonbinary. If your encounters don’t fit the traditional heterosexual penetration mold, you still need protection and testing. HPV doesn’t care what gender you are or how you define sex. It only needs skin. And it's directly linked to cervical, anal, and throat cancers, so ignoring it because you didn’t “go all the way” puts your long-term health at risk.
And yes, you can get HPV from oral sex. That means your mouth can be a site of transmission, even if the only thing you’ve done is perform. This is why so many people are confused when they test positive. They assume that if they haven’t had penis-in-vagina sex, they’re clean. But testing positive isn’t a moral failure. It’s biology.
Why Oral Sex Isn’t “Safe” by Default
“We only did oral” sounds like a safety net, until it isn’t. The truth is that oral sex, while lower risk than penetrative sex for some STDs, still carries real risks for others. Gonorrhea can infect the throat, often without symptoms. Herpes can pass from mouth to genitals. HPV lives in the tonsils and base of the tongue. And syphilis can enter through microscopic tears during oral contact.
It gets more complicated when you factor in asymptomatic partners. Someone could have gonorrhea in their throat and not even know it. When they go down on you, the bacteria spreads, and now it’s living in your urethra, cervix, or rectum. The symptoms might be mild. A slight discharge. A sore throat. Or nothing. But the infection is active and spreading. That’s how people end up confused: “But it was just oral.”
Public health data backs this up. According to the CDC, pharyngeal gonorrhea (gonorrhea of the throat) is increasingly common in younger populations, especially among those who don’t consider oral sex to be “real sex.” So if you’ve been skipping protection during oral, you’re not alone, but it’s time to rethink your risk model.
What About Kissing, Fingering, and Toys?
We don’t talk enough about the small stuff. The moments between sex that aren’t always named. Fingering. Dry humping. Mutual masturbation. Sharing a vibrator during a makeout session. All of these can feel low-risk or harmless. And most of the time? They are. But not always.
Let’s walk through a scene. You use a toy with your partner. It’s used vaginally, then used anally, or vice versa, without a barrier and without cleaning. If one of you has chlamydia, it can spread. If it’s a herpes outbreak, even microscopic residue can transmit the virus. And if either of you has an open cut or irritated skin (think shaving or waxing), that creates a literal entry point.
Now let’s talk about hands. They move from one body to another all the time. Fluids on fingers, if not washed in between, can carry traces of HPV, chlamydia, or herpes. It’s rare, but not impossible. And in queer, lesbian, and nonbinary relationships, this may be the primary form of sex, which means risks are overlooked entirely in hetero-focused health materials.
Here’s a table summarizing how common non-intercourse activities still pose transmission risk:
| Activity | STD Risk Level | Prevention Tips |
|---|---|---|
| Kissing (with cold sores) | Moderate (for Herpes) | Avoid kissing during outbreaks |
| Fingering or mutual masturbation | Low (can be higher with fluids or cuts) | Wash hands, clip nails, consider gloves |
| Shared sex toys | Moderate to High (depending on use) | Use condoms on toys, clean between uses |
| Oral sex | Moderate (especially for HPV, Herpes) | Dental dams, condoms, avoid contact with sores |
Table 2: Relative risk and prevention for non-penetrative sexual activities.
STDs Don’t Require Ejaculation, Or Even Arousal
Another myth? That you need to “finish” or even be fully turned on for risk to exist. Not true. Some of the most contagious STDs, like Herpes and HPV, spread during the warm-up phase. Just being naked, close, and grinding skin on skin is enough.
You can be infected from a partner who didn’t ejaculate. You can get gonorrhea from someone who only gave you oral for a few seconds. If a person has an active syphilis sore, just brushing against it, even unknowingly, is a risk. It’s not about climax. It’s about contact.
And the worst part? Many STDs are asymptomatic for weeks or months. You might feel fine. Your partner might look totally clean. But that doesn’t mean there’s no risk. This is why testing is key, and why delaying testing just because you didn’t “go all the way” can be dangerous.
Testing Still Matters, Even If You’re a Virgin
This is the part no one told you in health class: being a virgin doesn’t protect you from exposure. Testing isn’t a punishment or a confession of wrongdoing. It’s a basic part of health maintenance, like brushing your teeth or checking your blood pressure. If you’ve had oral sex, shared toys, or touched someone intimately, you qualify for an STI screening.
At-home test kits make this easier than ever. You don’t have to go to a clinic or explain yourself to a nurse. You can swab or pee in a cup in your own bathroom and send it off. Or you can use a rapid test and get results within minutes. No judgment. No awkward questions.
And if something comes back positive? That’s not a verdict on your choices or identity. It’s information. And with information, you can treat, prevent, and move forward.
This at-home combo test kit screens for the most common STDs discreetly and quickly, ideal for those moments when you’re not sure if your experience “counts.”
Case Study: “I Didn't Even Think I Needed to Test”
Marcus, 22, had been dating his partner for a few months. They agreed to keep things “PG-13” until they felt ready for sex. They fooled around, oral, some naked cuddling, touching, using fingers. When his partner tested positive for gonorrhea, Marcus was stunned. “But we didn’t have sex. Not even once.” He felt betrayed by his own body.
“I felt stupid for not knowing better. I thought I was being safe because we avoided ‘real’ sex. But no one ever explained the rest of it. No one said oral could give you an STD.”
Marcus tested positive in his throat. He’d received oral and given it too. One careless encounter was enough. It wasn’t about recklessness, it was about ignorance. And he’s not alone. Too many people think abstinence from penetration is protection. But protection means knowledge, boundaries, and testing. Not avoidance.
People are also reading: Oral Sex Isn’t Risk-Free: 6 STDs You Can Get From Going Down on Someone
“But I Didn’t Feel Anything”, The Asymptomatic Trap
More than half of all STDs can show up with zero symptoms, especially in the early weeks. That includes chlamydia, gonorrhea, syphilis, and even early-stage HIV. You might feel perfectly fine and still be carrying something contagious. This is why non-penetrative exposures can still lead to surprise diagnoses weeks or months later.
Take oral chlamydia. It often doesn’t show up as anything more than a mild sore throat, if that. You might brush it off as allergies or a cold. But it’s there, and if you give oral sex to someone else, you could pass it along. This silent cycle is how infections move through communities. Not because people are careless, but because they don’t know they’re infectious in the first place.
That’s why regular testing matters. If you’ve engaged in any intimate contact, especially oral, shared toys, or skin-on-skin, you deserve answers. Testing after 14 days post-exposure can catch most bacterial STDs. For viral ones like herpes or HIV, timelines vary a bit more. But timing shouldn’t delay your peace of mind. You can always test now and retest later if needed.
Check Your STD Status in Minutes
Test at Home with Remedium10-in-1 STD Test Kit

 For Women
For Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $189.00 $490.00
For all 10 tests
Timing Still Matters, Even Without Sex
Testing too early can lead to false reassurance. The STD might be in your system but not detectable yet. This period, called the window period, varies by infection. And yes, it still applies even if you didn’t have intercourse. A quick reference can help you decide when to test.
| STD | Can Spread Without Sex? | Minimum Test Window | Best Time to Test |
|---|---|---|---|
| Chlamydia | Yes (oral, toys, fluids) | 7 days | 14+ days |
| Gonorrhea | Yes (oral, fluids, shared toys) | 7 days | 14+ days |
| Herpes (HSV-1/2) | Yes (kissing, rubbing) | 4–12 days (after symptoms) | Wait for outbreak or 12 weeks for antibodies |
| HPV | Yes (skin-to-skin) | Not routinely tested without symptoms | Annual cervical or anal screening if applicable |
| Syphilis | Yes (skin, sores, oral) | 3 weeks | 6–12 weeks |
Table 3: Window periods for common STDs that spread without penetrative sex.
If you’re feeling unsure when to test, don’t freeze. Test once at the two-week mark for bacterial infections. Then test again after 6–12 weeks if you’re worried about viruses like herpes or syphilis. This staggered testing strategy gives you accurate results without the waiting anxiety.
It’s Not About Shame, It’s About Truth
If there’s one thing to take away from all of this, it’s that STD risk isn’t a morality scorecard. You can be a virgin. You can be queer. You can be cautious. And still end up exposed. That doesn’t make you reckless. It makes you human.
STDs don’t discriminate. They don’t wait for “real” sex to show up. And they don’t mean you’re dirty or broken. They mean you’re alive, you’re intimate, and you’re part of a world where closeness has consequences. That’s not shameful. That’s science.
Testing is the opposite of guilt. It’s care. It’s clarity. It’s power. Whether you’ve shared a toy, a kiss, or just a question, you deserve to know what’s going on in your body. And if you’re negative? Great, that’s peace of mind. If you’re positive? Great, now you can treat it, protect others, and move forward.
FAQs
1. I haven’t had “real” sex. Do I really need to worry about STDs?
Yes. “Real” sex is a social label, your body doesn't care what you call it. If there was skin-to-skin contact, oral sex, or shared toys, you’ve opened a door. Doesn’t mean you have an infection. Just means testing is the smart move. Think of it like brushing your teeth, not because they’re dirty, but because you care.
2. Can oral sex give you something serious?
Totally. You can get gonorrhea in your throat, chlamydia in your mouth, and herpes almost anywhere. And most people who have these orally? Don’t feel a thing. That’s what makes it sneaky, and why it spreads so easily through “just oral.”
3. How about kissing? That can’t give me an STD… right?
If someone has an active cold sore (hello, oral herpes), that kiss is more than sweet, it’s infectious. Most people get HSV-1 this way. And once you’ve got it, you’ve got it for life. Still kissable. Still lovable. But yeah, kissing can definitely be more than innocent if there’s a sore in the picture.
4. I share toys with my partner. Do I need to clean them every time?
Yes, like your toothbrush, but more personal. Toys can carry chlamydia, gonorrhea, even traces of HIV if there’s blood. Use a condom over them if you're switching between partners or body parts, and clean them with soap and water (or a toy-safe disinfectant). Shared pleasure shouldn't come with shared bacteria.
5. I don’t have any symptoms. Should I still get tested?
If you’ve had contact, yes. Most STDs don’t throw a parade. No itching, burning, or discharge doesn’t mean all’s clear. Silent doesn’t mean absent. That’s how people end up saying “I had no idea until I got tested.” You deserve better than surprise results.
6. How long should I wait before testing if I think I was exposed?
For chlamydia and gonorrhea, test after 7–14 days. For syphilis or herpes, 3–12 weeks is more reliable. If it’s only been a few days, testing now can give you a baseline, then follow up. Peace of mind comes in stages.
7. Does being a “virgin” actually protect me?
Nope. Virginity is a cultural concept, not a medical shield. If you’ve had oral sex, been touched, touched someone else, or used toys, your body’s had contact. Virgin or not, exposure is exposure. You can be smart, safe, and still get something, and that’s not a failure.
8. Are rapid STD tests legit if I didn’t have “real sex”?
Yes, 100%. A rapid STD test doesn't care how you were exposed. It detects infections, period. If a bacteria is present, the test picks it up. It’s like asking if a thermometer only works after a certain kind of fever. It works when you need answers.
9. Can I get herpes without knowing the other person had it?
Yes, and it’s actually pretty common. Many people carry herpes (HSV-1 or HSV-2) without ever having symptoms. It can still spread during skin contact, even when there are no visible sores. That’s why it’s often called “the silent guest.”
10. If I get an STD this way, does it mean I was irresponsible?
Absolutely not. You were being human. Exploring. Connecting. Being intimate doesn’t mean being reckless, and getting an STD doesn’t mean you did anything wrong. It just means it’s time to get treated and move on. No judgment here. Just facts, solutions, and a hell of a lot of compassion.
You Deserve Answers, Not Assumptions
If you’ve ever walked away from a hookup wondering, “Wait, did that count?” then you already know how confusing the rules around STD risk can be. But here’s the truth: if there was close contact, moisture, or shared touch, there’s a possibility. That doesn’t mean panic. It means checking in with your body and giving yourself the gift of clarity.
You don’t need to explain your choices. You don’t need to have had “real” sex. You just need information. And an at-home STD test kit can help you get it, fast, private, and judgment-free.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate.
Sources
1. Planned Parenthood – STDs, Testing, and Prevention
2. About Sexually Transmitted Infections (STIs) | STI – CDC
3. About STI Risk and Oral Sex | STI – CDC
4. How to Prevent STIs | STI – CDC
5. About Genital HPV Infection | STI – CDC
6. Non‑sexual HPV transmission and role of vaccination for a cancer‑free future
7. STDs: Factsheet for the Public | NICHD
8. Sexually Transmitted Infections: Symptoms, Diagnosis & Treatment | Urology Health
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: Nia Carson, RN, MPH | Last medically reviewed: October 2025
This article is only for informational purposes and should not be taken as medical advice.










