Quick Answer: The best at-home STD tests are those that are accurate like a lab test, ship discreetly, and give results quickly. Check for FDA approval, clear instructions for how to collect the sample, and help if you test positive.
Why So Many People Are Turning to At-Home STD Testing
Let’s be real, clinic testing isn’t accessible or comfortable for everyone. For some, it’s the embarrassment of facing a receptionist or explaining your sex life to a doctor you don’t trust. For others, it’s simply distance. Rural towns with no clinics. Work schedules that make weekday appointments impossible. Or trauma histories that make medical settings feel unsafe. In those gaps, at-home testing has quietly become a lifeline.
Take Jordan, 28. After hooking up with someone at a music festival, they developed a persistent sore throat and mild rash around their thighs. “I didn’t want to drive two hours just to be judged,” they said. “So I ordered a combo test kit online, took the swabs in my bathroom, and mailed it in the next day. Results came back in three days. Negative. Huge relief.”
You shouldn't have to pay for that kind of peace of mind. But not all test kits give it to you in the same way. Some come late, don't have clear instructions, or even confuse users with results that are hard to read. Some don't even check for common STDs unless you pay more or sign up. Those extra steps can seem impossible to get through if you're already anxious.
What to Look For in a Good STD Test Kit
So what separates a trustworthy kit from a frustrating one? You want a test that meets three key standards: accuracy, privacy, and usability. And you want those things without having to decode medical jargon or scroll through fine print at checkout.
Accuracy matters because a false negative can mean delayed treatment and risk to your partners. Kits using lab-based NAAT (nucleic acid amplification testing) or PCR methods offer the most reliable results for infections like chlamydia, gonorrhea, and trichomoniasis. For viral STDs like HIV or herpes, antigen or antibody tests are standard, but timing is everything. More on that in a bit.
Privacy isn't just about discreet packaging (though that helps). It's about what happens after your sample is mailed. Does the company protect your data? Can you choose not to share results with insurance? Some tests offer anonymous accounts. Others might auto-upload to health databases.
Usability means clear instructions, simple collection tools, and a results dashboard that doesn’t require a medical degree. The best kits walk you through each step like a friend would, calm, clear, and non-judgmental.

People are also reading: Sex, Drugs, and STDs: What They Don’t Tell You About Festival Season
Brand Showdown: How Today’s Top Kits Compare
We reviewed five leading at-home STD test providers based on accuracy, privacy, turnaround time, and support. Some offer rapid tests with results in minutes; others rely on mailed-in lab kits. Here's how they stack up:
| Brand | Test Method | Privacy Level | Turnaround Time | Accuracy | Post-Test Support |
|---|---|---|---|---|---|
| LetsGetChecked | Mail-in lab (CLIA certified) | High (discreet shipping, private portal) | 2–5 days | High (NAAT, FDA-cleared labs) | Free nurse consult if positive |
| STDcheck | Lab visit (order online) | Moderate (clinic required) | Same day to 3 days | Very High | Telehealth and treatment referrals |
| Everlywell | Mail-in lab | High | 2–5 days | High | Physician-reviewed results |
| myLAB Box | Mail-in or rapid | Very High | 1–5 days | Moderate to High (varies by test) | Telehealth follow-up |
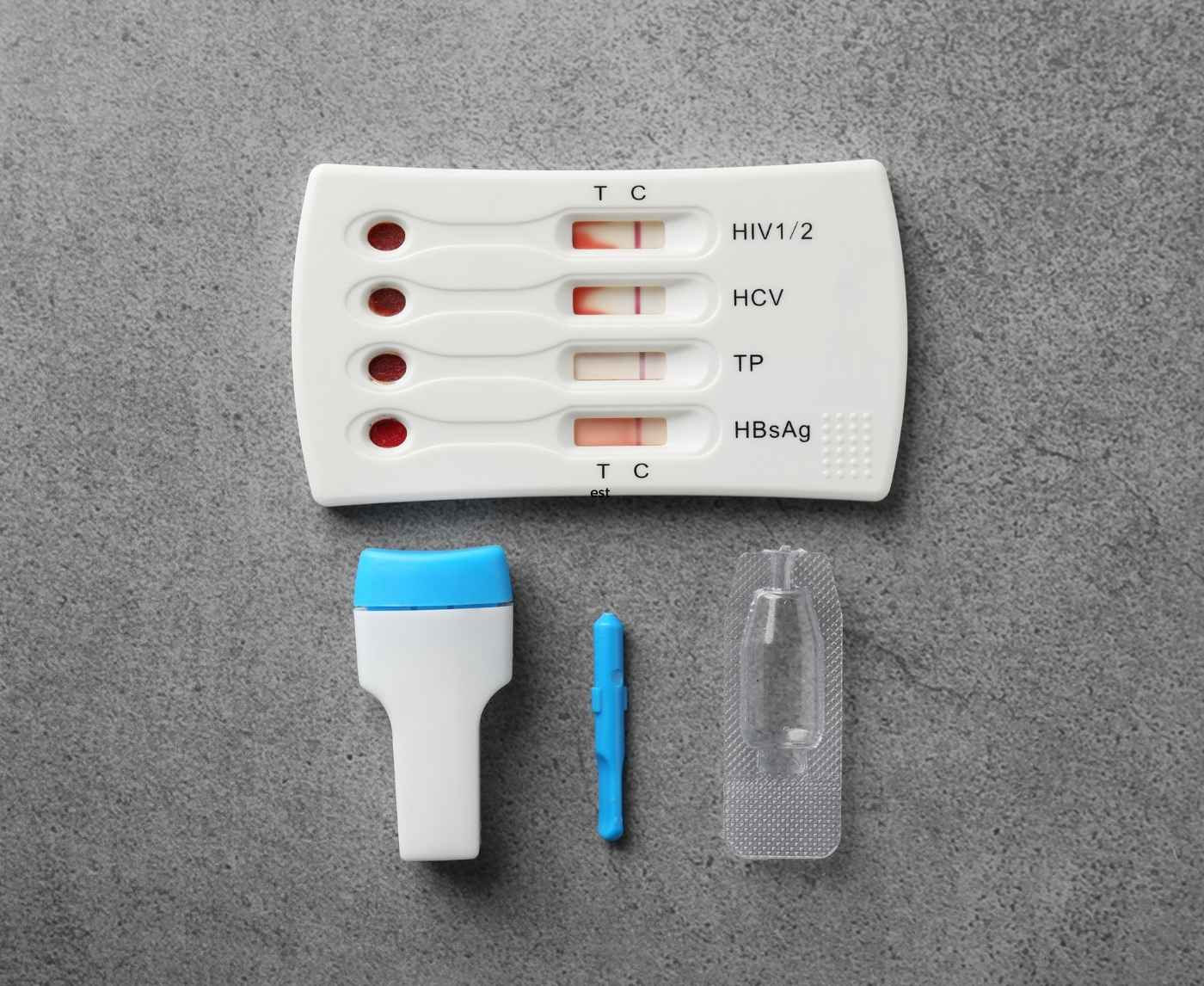
| STD Rapid Test Kits | Rapid lateral flow (home use) | Very High (no lab, no upload) | 15–20 minutes | Moderate to High (HIV, Syphilis) | None built-in; external support available |
Table 1. Comparison of leading at-home STD test kits by privacy, turnaround, and accuracy. Accuracy ratings are based on test method (NAAT > lateral flow) and third-party evaluations.
One thing to note: STD Rapid Test Kits don’t send your sample to a lab, which means no digital record exists unless you create one. This can be a huge plus for people worried about privacy or insurance tracking. But it also means you need to be confident in reading your result at home. We'll talk more about faint lines and user error in Part 2.
Meanwhile, mail-in kits like Everlywell and LetsGetChecked often feel more “clinical” but are highly accurate and include lab oversight. They’re a solid choice if you're testing multiple STDs or want a digital record for follow-up care.
Check Your STD Status in Minutes
Test at Home with Remedium7-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $129.00 $343.00
For all 7 tests
What It’s Like to Actually Use These Kits
Let’s walk through what happens once that discreet package lands on your doorstep. For some kits, like STD Rapid Test Kits, it’s just you, a lancet, and a results strip. No mailing, no app, no nurse on standby. For others, like Everlywell or myLAB Box, you’ll be collecting urine or swabs, then packaging everything for a mail drop-off. Both approaches come with trade-offs, and emotional terrain.
Ty, 31, shared what it felt like to test at home after a rough breakup: “I got the kit in the mail, but I froze. The instructions looked easy, but part of me didn’t want to know. It sat on my dresser for a week before I finally swabbed and mailed it. When the results came back clear, I cried, relief, but also guilt that I waited.”
That hesitation is normal. So is confusion. Especially when you’re handling your own sample. Most kits now include QR-coded instruction videos or picture guides. Still, user error remains a top reason for inaccurate results. Swabbing too shallow, touching the sterile tip, or underfilling collection tubes can all interfere with detection, especially for chlamydia and gonorrhea.
Then there’s the mental rollercoaster of waiting. With lab kits, you’re often refreshing an app every few hours, heart in your throat. With rapid tests, the nerves compress into a tense 15-minute window. Either way, knowing when to test, and retest, is critical for getting reliable results.
Timing Isn’t Just Technical, It’s Everything
One of the most misunderstood parts of at-home STD testing is the window period. That’s the time between exposure and when a test can reliably detect infection. Testing too early can give you a false sense of security, especially for infections like syphilis or HIV, which take longer to show up in blood or swab samples.
Think of it this way: If you had unprotected sex on Saturday, testing Monday might feel urgent, but it’s not smart. Most STDs won’t be detectable yet. Testing on day 10 may catch some, but not all. Testing at day 21+ gives you better odds of accuracy. But the best plan often includes an initial test plus a follow-up.
| STD | Earliest Detectable | Recommended Testing Window | Retest Needed? |
|---|---|---|---|
| Chlamydia | 5–7 days | 14+ days after exposure | Yes, if tested too early |
| Gonorrhea | 5–7 days | 14+ days | Yes |
| Syphilis | 21 days | 6 weeks+ | Yes |
| HIV | 10 days (NAAT), 18–45 days (antibody) | 4–12 weeks | Often recommended |
| Herpes (HSV-2) | 4–6 weeks | 6–12 weeks | Sometimes |
Table 2. Common STDs and their recommended testing windows. Retesting ensures accuracy if your first test is within the early window.
This is where decision tools help. Some test providers include timeline graphics or symptom-based selectors. But many don’t. That’s why it’s so easy to misread a negative as “safe” when it might just be “too soon.”
Imagine Camila, 25, who had a new partner and tested five days later using a rapid HIV test. The result was negative. But a month later, she developed night sweats and a swollen gland. A retest through a mail-in combo kit revealed an early HIV infection. “I was furious at myself for trusting that first test,” she said. “But no one told me I tested too soon.”
That’s why we recommend pairing a rapid test with a calendar reminder to retest, especially if symptoms show up or exposure was high-risk. Some brands, like STD Rapid Test Kits, include multiple test strips in one box, which allows users to test again without waiting for shipping.
False Negatives, Faint Lines, and That “Is This a Line?” Moment
Few things are as nerve-wracking as watching a rapid test develop. A faint line appears, or doesn’t. You squint, tilt it toward the light, take a picture to text a friend, but you’re still unsure. This happens more often than you’d think.
In lateral flow tests (the kind that resemble pregnancy strips), even a faint line in the “T” area can indicate a positive result. But smudges, evaporation lines, or incorrect timing can mimic a result. Each kit is different, which makes consistency tricky. And user anxiety doesn’t help.
Ravi, 34, tested with a syphilis rapid test after a hookup left him feeling off. “There was the faintest shadow of a line. I thought I imagined it. Googled for an hour. Posted on Reddit. Eventually I just retested three days later. This time, it was clear. Positive.”
False negatives are another issue. Especially with early testing or user error during collection. That’s why follow-up is part of every major clinical protocol. It’s not about paranoia, it’s about confirmation.
Brands like myLAB Box and LetsGetChecked allow you to speak with a nurse or doctor if your results raise questions. Others, like STD Rapid Test Kits, put the responsibility on you to interpret the result, but also keep your data completely private. It’s a tradeoff, and it should be a conscious one.
If you're someone who tends to spiral, choose a kit that comes with a support pathway. If privacy is your top priority, opt for a non-digital, instant-result option you can read and discard discreetly. Either way, retesting is your safety net.

People are also reading: Which Antibiotic Kills Chlamydia the Quickest? Here’s What Experts Say
When the Test Is Positive: What Comes Next (And Who Helps)
Testing positive at home can feel like the floor drops out. Even when the kit instructions say it’s “only a preliminary result,” the emotional weight is very real. This is the moment where support matters, and where brands really diverge.
For some people, like Lina, 23, a positive chlamydia result came with built-in help. “The app sent me a link to a telehealth doctor. I had meds called in within two hours. No judgment, no waiting room,” she said. That kind of seamless care pathway is only available with kits that include physician oversight, like LetsGetChecked or Everlywell.
Others, like STD Rapid Test Kits, don’t provide in-house follow-up. This means that if you test positive, you’ll need to confirm the result through a clinic or mail-in lab before beginning treatment. The upside? No digital trail. The downside? More legwork, and potentially more anxiety while you wait.
If you’re testing for HIV or syphilis, two conditions that require confirmatory testing no matter what, look for kits that flag that clearly. Some brands bury that information in fine print. Others, like myLAB Box, highlight it directly on the results page with links to next steps.
There’s no “one right way” to get support. But if you're not sure how you'd emotionally handle a positive result alone, choose a brand that includes a nurse consult or telehealth bridge. It’s not weakness, it’s care.
Cost, Insurance, and the Hidden Price of Privacy
Let’s talk money, because cost can be a dealbreaker. At-home STD test kits range widely in price depending on how many infections they test for, whether the tests are rapid or lab-analyzed, and what kind of support is included.
Some of the most comprehensive mail-in kits can cost $150 to $350. These often include tests for chlamydia, gonorrhea, syphilis, HIV, trichomoniasis, and sometimes hepatitis B/C or HPV. Single STD tests (like HIV-only) can run between $39 and $89 depending on the brand and method. Rapid test kits like those from STD Rapid Test Kits often cost less per item, sometimes under $20 per test strip, but require you to interpret results yourself.
Insurance adds another layer. Some brands accept FSA or HSA cards. A few, like Everlywell, offer receipts you can submit for reimbursement. But most do not bill insurance directly, intentionally. Using insurance means your test might show up in records, potentially impacting privacy or deductible status.
It’s a trade-off: affordability vs anonymity. And it’s okay to prioritize one over the other depending on your situation. Just know what you’re paying for. A cheaper test that gives you bad instructions, no support, or vague results can actually cost more, emotionally, physically, and financially, down the line.
Check Your STD Status in Minutes
Test at Home with Remedium6-in-1 STD Rapid Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $119.00 $294.00
For all 6 tests
Shipping, Discretion, and Who Really Sees Your Results
If you’re worried about roommates, nosy family members, or partners who might open your mail, you're not being paranoid. You're being real. Privacy starts with packaging, and not every company gets this right.
STD Rapid Test Kits arrive in plain envelopes with no health branding. So do kits from myLAB Box and LetsGetChecked. Others, like STDcheck, require a lab visit, which might mean showing ID or interacting with clinic staff. For some users, that’s a dealbreaker.
Beyond the box, consider the data. When you register a test online, do you have to give your real name? Can you use a burner email? Will your results be saved in a portal indefinitely? These questions matter. And many brands don’t offer clear answers up front.
For Jayden, 38, who was exploring sex with men for the first time, anonymity was everything. “I wasn’t ready to have anything linked to my real name. The ability to test without being tracked gave me the courage to do it in the first place.”
That’s not about shame, it’s about safety. Especially for queer, trans, or non-monogamous users who’ve experienced stigma in healthcare settings. If a brand doesn’t speak to that directly, they probably haven’t built for you.
STD Rapid Test Kits offer full control, you don’t even need an account. But that control also means responsibility. No automatic follow-up. No digital record. Just your result and what you choose to do next.
Don’t Just Test, Plan for Retesting Too
Testing once is great. But retesting is what closes the loop. Most medical guidance recommends a second test within three months after exposure, especially if the first test was within the early window period. If you’re sexually active with new or multiple partners, retesting every three to six months is considered best practice.
Some at-home kits support this. STD Rapid Test Kits offer multipacks for serial testing. myLAB Box has a quarterly subscription. LetsGetChecked sends email reminders based on your previous results. Others don’t mention retesting at all.
Marisol, 26, didn’t think she’d need to test again. But after taking antibiotics for chlamydia, she realized her partner had never tested. “He thought my negative meant he was fine. It wasn’t. I got reinfected. That’s when I started testing regularly.”
Testing isn't just a one-time fix, it’s part of sexual health maintenance. And the best kits make that part easier, not harder. Look for brands that normalize retesting, offer discreet reorders, and educate without fear.
Whether you're testing because of a specific exposure or just doing a wellness check, remember: clarity now can save you from complications later. And if your head keeps spinning with questions, peace of mind is one test away. This at-home combo test kit checks for the most common STDs discreetly and quickly.
FAQs
1. Are these at-home STD tests actually accurate?
Yes, when used at the right time and the right way. Lab-based kits like NAAT or PCR have clinical-level accuracy, often over 95% for things like chlamydia and gonorrhea. Rapid tests are solid too, especially for HIV and syphilis, but they depend more on you following instructions exactly. So no rushing it while half-dressed and late for work. Take your time. Accuracy starts with the swab.
2. What’s the deal with faint lines? Do they count?
Short answer: Yep, they count. If you see even a ghost of a line in the test area, especially with rapid kits, that’s technically a positive. It’s not a mood ring; it doesn’t have to be bold to be real. When in doubt, don’t stare at it for an hour. Just retest or follow up with a lab-based kit to confirm.
3. Can I use these tests if I feel totally fine?
Please do. Most STDs are sneaky, no symptoms at all for weeks or months. You can feel amazing and still be infectious. These tests are for peace of mind, not just panic mode. Think of them like flossing: the healthiest habits are the ones you do before there’s a problem.
4. Is my name going in some database if I test at home?
Not necessarily. Brands like STD Rapid Test Kits don’t collect your name at all. You buy it, test it, and toss it, no account, no log. Others that use labs may ask for ID to comply with health laws. So if privacy is your dealbreaker, pick a kit that leaves no digital breadcrumb trail.
5. I hooked up last weekend. Can I test now?
You can, but it might be too soon. Most STDs won’t show up accurately for 10 to 21 days. That early test might be a false negative. If it helps your anxiety, test now and again at the 3-week mark. Think of it like a two-step dance: quick check, then final confirmation.
6. What if my test says positive? Am I screwed?
Not even close. Most STDs are totally treatable, especially bacterial ones like chlamydia or gonorrhea. If it’s positive, confirm with a lab if needed, get treated, and let your recent partners know. It’s a bump in the road, not a life sentence. You’re still worthy of pleasure, love, and health.
7. How often should I be testing, really?
If you’re sexually active with new or multiple partners, every 3 to 6 months is the sweet spot. After any unprotected hookup, testing two to three weeks later (and again at 6 weeks) covers your bases. And if you’re monogamous? Once a year isn’t overkill, it’s just respect for yourself and your partner.
8. Why are some kits so cheap and others so expensive?
Usually, it comes down to what’s included. A $20 kit might test for one thing, use a rapid strip, and offer no support. A $250 kit might screen for eight infections, use lab analysis, and include a doctor consult. Both can be legit, it just depends on what you need. You're not being cheap or extra. You're shopping for answers.
9. Can I pay with FSA or HSA funds?
Yep, most of the good ones let you use pre-tax health cards. Just look for the FSA/HSA badge on the site. And no, it doesn’t mean your job will know. These accounts are usually pretty private if you're paying direct, not through insurance.
10. I’m queer. I’m trans. Will these kits still work for me?
Some do better than others. The test itself doesn’t care who you are, but the company you buy from should. Look for brands that talk openly about inclusive care, use gender-neutral instructions, and don’t assume your anatomy. If the site feels like it was built for someone else, it probably was. You deserve better.
You Deserve Answers, Not Assumptions
If you've made it this far, you're already taking charge of your sexual health. That matters. Whether you're testing because something feels off, or just want peace of mind, the right at-home STD test can offer clarity without shame. The key is knowing what you need: speed, accuracy, privacy, or maybe all three.
Stop wondering and get the answers you need. This at-home combo test kit checks for the most common STDs discreetly and quickly.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate.
Sources
1. Self‑collection of samples as an additional approach to STI testing
2. Home screening for STDs in high‑risk populations
3. Accuracy of self vs provider-collected specimens
4. Extragenital self-collection for gonorrhea/chlamydia
5. Direct‑to‑Consumer STI Testing: Benefits and Pitfalls
6. World Health Organization: STI Fact Sheet
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: Tara N. Alvarez, MPH | Last medically reviewed: September 2025
This article is for information only and should not be taken as medical advice.