Quick Answer: STD tests, especially at home, are medically valid, but no test is perfect. Timing, symptoms, and the type of infection all affect accuracy. A negative result doesn’t always mean you're in the clear.
Why This Still Happens (And Who This Is For)
If you’ve ever sat in a parked car staring at a test strip that said “negative” while your body said “something’s wrong,” this article is for you. If you’ve hesitated to trust at-home tests because a friend called them “fake” or you once got a false positive, or negative, this is for you. If you’ve ever believed that testing is only for people who sleep around, or that “you’d just know” if you had something, this is definitely for you.
We live in a world where sex is everywhere but honest conversations about testing are rare. That vacuum gets filled with myths, some rooted in shame, some in outdated science, and many in fear. This article breaks those down, one by one. Not to scare you, but to set you free. Because when you understand what’s really going on, you can act without shame or guesswork. You can protect yourself and your partners with confidence, not confusion.
“At-Home STD Tests Aren’t Real”
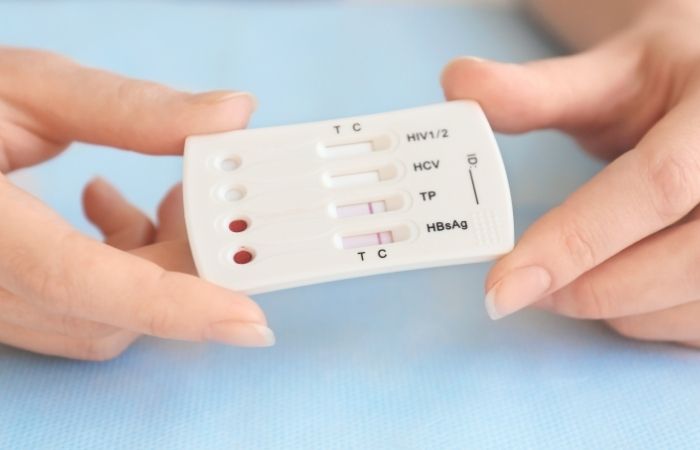
This one refuses to die. Whether it's Reddit threads questioning test strips or a friend whispering that "those online kits are fake," the stigma around home testing persists. But here’s the truth: CDC guidelines acknowledge multiple valid testing options, including self-collected swabs and mail-in kits.
This one won't die. There is still a stigma around home testing, whether it's Reddit threads that question test strips or a friend who says, "those online kits are fake." But here's the truth: the CDC says that there are many valid testing options, such as self-collected swabs and mail-in kits.
The most common at-home STD tests use a method called NAAT (nucleic acid amplification testing), the same gold standard many clinics use. Some use rapid antigen detection, which gives results in minutes. While not every test type is suited for every infection, these kits are real, lab-certified, and increasingly FDA-cleared. The real issue isn’t legitimacy, it’s timing and usage. A perfectly good test taken too early can miss an infection that’s still incubating.
At-Home vs Clinic STD Tests, What’s Really Different?
| Test Type | Where It's Done | Accuracy Range | Common for | Result Time |
|---|---|---|---|---|
| At-Home Rapid Test | Self-collected, results at home | Moderate to High | HIV, Syphilis | 10–20 minutes |
| Mail-In Lab Test (NAAT) | Self-collected, processed in lab | High (same as clinic) | Chlamydia, Gonorrhea, Trichomoniasis | 2–4 days |
| Clinic-Based NAAT or Antibody | In-person collection and processing | Very High | All STDs including Herpes, HIV | 1–5 days |
Figure 1. Comparison of testing environments. While clinic-based tests remain the most comprehensive, at-home options offer high accuracy for many infections when timed correctly.
“If I Have Symptoms, It’ll Show Up on a Test”
Here’s where things get messy. Many people assume symptoms and test results move in sync. But they don’t. That burning you feel two days after oral sex? It might not align with the testing window of the infection you're worried about. Symptoms can start before the infection is detectable. In other cases, the symptoms may be from something entirely different, like a UTI or irritation, and the STD isn’t even present. So yes, you can have symptoms and still test negative. And yes, you can test positive while feeling absolutely nothing.
A real-world example: Keira, 29, noticed a cluster of painful bumps after a weekend hookup. She rushed to a clinic and tested negative for everything. The nurse suggested herpes but said it was “probably too soon to show up.” Two weeks later, a retest came back positive for HSV-2. The initial test wasn’t wrong, it was just too early. The myth here isn’t about symptoms, it’s the belief that your body and your test are on the same timeline. They’re not.

People are also reading: Not Strep, Not a Cold, This Could Be an STD
“If You Test Negative, You're Definitely Clean”
This is the most dangerous myth of all. It gives people false peace and leaves infections untreated, and unknowingly spread. A negative test doesn’t mean you don’t have anything. It means the test didn’t detect anything at that moment. That’s it. Think of it like trying to catch fish in a lake using the wrong bait at the wrong time. You could go home empty-handed and assume there are no fish. But they were there, you just didn’t have the right tool at the right time.
Here’s what most people don’t realize: each STD has a different window period, the time between exposure and when it can be reliably detected. If you test during that window, you might get a negative result even if you’re infected. Take HIV, for example. A rapid antibody test may miss it in the first two weeks after exposure. A NAAT test could catch it earlier, but not every clinic offers it. Chlamydia and gonorrhea usually show up within 7–14 days, but some tests require longer for accuracy.
And then there’s test sensitivity. Even within the right window, no test is 100% perfect. False negatives happen. They’re not common, but they’re real. And they’re more likely if the sample is collected poorly, the test is mishandled, or you’re in the very early stages of infection.
Table: Window Periods by Infection
| STD | Earliest Reliable Detection | Retest Recommended? |
|---|---|---|
| Chlamydia | 7–14 days | Yes, at 2–3 weeks if symptoms persist |
| Gonorrhea | 5–14 days | Yes, if tested before day 7 |
| HIV (Ag/Ab combo) | 18–45 days | Yes, at 6+ weeks for confirmation |
| Herpes (antibody) | 4–12 weeks | Yes, especially if symptoms occurred recently |
| Syphilis | 3–6 weeks | Yes, especially for early-stage symptoms |
Figure 2. Even the best STD tests need to be timed correctly. Retesting can be crucial after early exposure or persistent symptoms.
“At-Home Tests Are More Likely to Be Wrong”
This one stems from a mix of fear and misunderstanding. Let’s be clear: at-home test kits, especially the ones that require you to mail in your sample, often use the same lab techniques as clinics. What matters more is how the sample is collected and when the test is done.
Take Marlon, 35, who used an at-home test after a one-night stand. He followed the instructions, mailed the kit, and got a negative for chlamydia. But he had pain during urination and a milky discharge. “I figured the test was wrong,” he said. It wasn’t. He’d tested just four days after exposure, too early for many NAAT tests to catch anything. He retested on day 11. Positive.
Home tests aren’t less accurate because they’re done at home, they’re only less accurate when used improperly or too early. In fact, many studies show home tests can increase testing rates in underserved or stigmatized populations. Privacy leads to more people testing. And more testing means earlier treatment, fewer transmissions, and less shame.
When Your Test Is Negative… But Something Feels Off
Let’s talk about the in-between. The space where you’ve tested negative but symptoms linger. Maybe it’s a dull itch that won’t go away. A new bump. A weird smell. Your test says “nothing detected.” Your body says otherwise. What now?
First, breathe. False negatives happen, but they don’t mean you're broken, dirty, or reckless. They mean you need more time or another test. Use this moment to gather facts, not shame. If it’s been under 7 days since exposure, retesting is smart. If your test was rapid only, consider a lab-based one. If you used an oral swab but your exposure was genital, you might need a different sample type.
If your test was done correctly and outside the window period, and you still have symptoms, it may be time to rule out non-STD causes: yeast, bacterial vaginosis, UTI, allergic reaction, or even hormone changes can mimic STD symptoms. A sexual health provider or telehealth service can help sort this out.
But don’t gaslight your own instincts. If something feels wrong, it’s worth checking again. You’re not being paranoid. You’re being proactive.
Check Your STD Status in Minutes
Test at Home with Remedium10-in-1 STD Test Kit

 For Women
For Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $189.00 $490.00
For all 10 tests
You Deserve Clarity, Not Confusion
If your test result didn’t match what your body’s telling you, don’t wait in doubt. This FDA-approved combo test kit checks for multiple STDs at once, and gives you results you can trust, discreetly and quickly. Whether it’s your first test or your follow-up, the right timing can change everything.
“If My Partner Is Negative, I Must Be Too”
This is one of the most misleading and relationship-damaging beliefs people carry. It’s comforting to think that if your partner tests negative, you're both in the clear. But that’s not how transmission, or testing, works. Infections don’t always pass back and forth immediately. And not every test detects infections at the same stage for every person.
Consider Emily and Tayvon. They’d been exclusive for six months when Emily developed symptoms, burning, discharge, and low pelvic pain. She tested positive for chlamydia. Tayvon was furious and defensive. “I tested last month. Negative.” But Tayvon hadn’t tested since a partner before Emily. And his result came from a rapid-only screen that didn’t include chlamydia. Once retested using a full panel, Tayvon was also positive. The myth, that one person’s negative result proves both are fine, keeps people from taking responsibility for their own health and supporting their partners through testing without blame.
Testing isn't a loyalty test. It’s a medical check-in. And even the best relationships deserve reality-based care. Get tested together. Get retested if either of you has new symptoms. Choose curiosity over blame. Because being “clean” isn’t a moral status, it’s a temporary testing snapshot. And it can change with one encounter, one missed infection, or one outdated assumption.
“If I Already Had That STD Once, I’m Immune”
This one leads to some of the most quietly damaging cases of reinfection. Some people believe that after treatment for chlamydia or gonorrhea, they’re now immune, like chickenpox. The reality? Reinfection is common. In fact, the CDC recommends retesting three months after treatment for several STDs because reinfection rates are so high, especially if a partner wasn’t treated at the same time.
Let’s break it down with a short scene: Adrian, 24, tested positive for chlamydia in January. He took the full round of antibiotics and felt better within days. No follow-up. No partner testing. By April, he was back at the clinic, same symptoms. He was frustrated. “But I already had this.” Yes. And now you have it again.
STDs don’t build immunity. If your partner didn’t get treated, you can ping-pong infections back and forth. If you start a new relationship, you could pick something up again, regardless of what you’ve been treated for in the past. That’s why retesting is not paranoia, it’s protection.
So When Should You Retest? Let’s Get Real
The urge to test right away is normal. We want answers fast. But the most accurate answers often come with time, and the willingness to retest if things still feel off. Here’s how to think about it:
If you tested less than 7 days after a risky encounter and got a negative result, consider it a preliminary screen. Plan to test again around day 14, and once more if symptoms persist beyond that. If you were treated for an STD, wait at least 3 weeks before retesting to avoid false positives from lingering DNA fragments. For HIV or syphilis, longer windows may apply, 6 weeks or more for reliable detection.
And here’s a critical piece: retesting isn’t about mistrusting the first result, it’s about understanding how biology works. Infections incubate. Tests require thresholds. Sometimes your body is ready before the test is. Sometimes it’s the other way around.
People are also reading: Tinder, Testing, and Telling the Truth: Dating With an STD in 2025
Retesting Scenarios That Make Sense
| Scenario | When to Retest | Why It Matters |
|---|---|---|
| Tested within 5 days of exposure | Retest at 14–21 days | Early testing can miss active infection |
| Symptoms persist after negative test | Retest in 7–10 days | Rule out false negative or unrelated condition |
| Partner tested positive | Retest immediately, again in 2–3 weeks | You may be in the window period or have a new exposure |
| Treated for an STD | Retest at 3 months | Check for reinfection, especially if partner untreated |
| One-night stand or condom break | Initial test at 10 days, follow-up at 4–6 weeks | Covers incubation + window period overlap |
Figure 3. Retesting isn't redundant, it's smart. Especially when symptoms linger or exposure risk is high.
Let’s Talk About Shame (And Why It’s Not Helping)
Most of these myths don’t come from nowhere. They come from stigma, both external and internal. We've been taught that sex is dangerous, testing means guilt, and STDs are something that happen to “those” people. The problem is, that shame doesn’t protect anyone. It only pushes testing later, hides symptoms longer, and makes false security feel like safety.
If you’ve ever delayed testing because you didn’t want to be “that person”, you’re not alone. If you’ve ever ignored symptoms out of fear of judgment or rejection, millions of people have been there. And if you’ve ever gotten a result that didn’t match your symptoms and wondered if you were just making it up, you're absolutely not.
What you’re doing now, reading, learning, maybe preparing to retest, is health care. It’s strength. It’s a form of love: for yourself and for whoever you share your body with. Don’t let shame tell you otherwise.
FAQs
1. Can I really test negative and still have an STD?
Yes, and it's more common than people think. A test is a snapshot, it only shows what’s detectable at that moment. If you test too early, or if the infection hasn’t built up enough to register, it can slip under the radar. Doesn’t mean you’re fine. Doesn’t mean you're doomed either. It just means you might need a follow-up.
2. How soon is too soon to get tested after sex?
If you test within 48 hours, you’re probably wasting your time and money. Most STDs won’t show up that fast. Chlamydia and gonorrhea usually need about a week. HIV takes longer. One-night stand last weekend? Wait 10–14 days. Still nervous? Test now, then again later. That’s how pros do it.
3. Are those at-home kits actually legit?
Totally. Most mail-in tests use the exact same lab tech as clinics, just without the awkward gown and cold exam table. The trick? Following directions like your health depends on it (because it does). Timing and proper sample collection matter more than whether you’re wearing pants when you do it.
4. Why does my body feel off if my test says I’m fine?
Could be timing. Could be the wrong type of test. Could be a yeast infection pretending to be something worse. Your body isn’t lying, it’s just that not all tests are designed to detect every problem. If you feel off, trust yourself. Retest. Or talk to a provider who gets it.
5. My partner tested negative. Doesn’t that mean I’m good too?
Not necessarily. You’re two different bodies on two different timelines. They could be in the window period. They could’ve gotten tested for one thing and not another. Or they might have a dormant infection they don’t even know about. Get tested for you, not based on someone else’s results.
6. Can I catch the same STD more than once?
Sadly, yes. This isn’t chickenpox. Chlamydia, gonorrhea, even syphilis, they don’t hand out immunity cards. You can clear it with treatment and still get reinfected by a partner who didn’t get treated. That’s why doctors recommend retesting at three months, just in case it ping-pongs back your way.
7. Does oral sex really spread STDs?
Yep. Big time. Gonorrhea loves throats. Syphilis loves mouths. Herpes? Everywhere. Just because it's not penetrative doesn’t mean it’s risk-free. Protection helps, but testing is what keeps the mystery out of your mouth (and your partner’s).
8. Is it enough to test once a year?
Maybe, if you’ve had no new partners, no weird symptoms, and you’re in a monogamous situation where everyone’s been tested. But if anything’s changed? Test more. Think of it like dental cleanings, you wouldn’t skip those just because your teeth didn’t hurt.
9. I got a negative result... then a positive one later. What gives?
Welcome to the window period. It’s that annoying time after exposure when the infection is there, but tests aren’t ready to pick it up. The first test wasn't “wrong”, it was just early. That’s why retesting is part of the game. No shame in doing it twice.
10. Are rapid tests a waste of time?
Not at all. They’re fast, private, and useful, especially for things like HIV and syphilis. But they can miss early infections. Think of them like a first date: you get some important info, but you might need a follow-up to be sure. If something feels off, double-check with a lab test later.
You’re Not Broken, You’re Paying Attention
If you've made it this far, know this: your doubts are valid, your body deserves clarity, and your confusion doesn’t mean failure. In a world full of myths and misinformation, you’re doing the hard, brave thing, seeking answers. Whether you're dealing with a false negative, persistent symptoms, or post-treatment paranoia, you are not alone, and you're not doomed.
Your next test could bring peace of mind. Or a plan. Either way, you win.
Order your confidential combo STD test kit today and take back control, on your terms, in your time.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted five of the most relevant and reader-friendly sources.
Sources
1. Planned Parenthood: Why and When to Get Tested
2. CDC: STD Screening Recommendations
4. Serological Tests for Syphilis – PMC
5. Frequency and Characteristics of Biological False-Positive Syphilis Tests – PMC
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: C. Martinez, RN, MPH | Last medically reviewed: September 2025
This article is for informational purposes and does not replace medical advice.










