Quick Answer: Teen STD rates are rising even in well-informed households because shame, secrecy, and misinformation still run deep, especially around testing. “The Talk” isn’t enough without access, repetition, and safe follow-through.
Why This Guide Matters for Every Parent
Maybe you’ve had the awkward conversations. Maybe you even made it feel “not weird” to ask questions about sex, protection, or consent. That matters, hugely. But it doesn’t mean your teen is fully protected. Many parents assume that once a conversation happens, the job is done. But the reality is messier. Adolescents live in a world of peer pressure, misinformation, hookup culture, and often, emotional silence about sex and symptoms.
Parents of all backgrounds are discovering that even when they think their teen “isn’t like that,” the reality says otherwise. And it’s not about rebellion, it’s about the gap between knowledge and action. A 2023 study published in Sexually Transmitted Diseases found that even teens who understood STD risks were often too embarrassed to get tested or too misinformed to recognize symptoms.
This article is for every parent who’s ever said “But we talked about this.” It’s a no-judgment, fact-first guide to understanding what’s really going on, and what you can do that goes beyond just talking. We’ll cover what STDs look like in teens (hint: often nothing), when and how testing should happen, why even smart kids make risky decisions, and how to support your teen through diagnosis, treatment, and prevention without adding shame.

People are also reading: How Soon Will Gonorrhea Symptoms Start? A Real Timeline
The Silent Epidemic: What STDs Look Like in Teens
It’s easy to assume you'd know if your teen had an STD. But the truth is, most infections show no symptoms at all, or symptoms so subtle they get dismissed. Chlamydia, one of the most common STDs among adolescents, often presents with zero signs. When symptoms do appear, they might look like everyday irritation: mild discharge, itching, a single pimple, or a bit of burning that fades by morning.
Jared, 16, didn’t think twice when he noticed a spot on his inner thigh. He figured it was from track practice. Two weeks later, his girlfriend’s mom found out she had gonorrhea during a routine checkup. Jared had no idea he’d been exposed, he didn’t feel sick. He didn’t even know what gonorrhea was. And he wasn’t alone. Studies show over 70% of teens with chlamydia or gonorrhea report no symptoms at all, according to the CDC.
Many teens think symptoms have to be “gross” or extreme, pus, sores, unbearable pain. The reality is far more subtle, especially in the early stages. That’s what makes routine testing essential, even in teens who don’t appear sick or who have had “only oral” sex.
Why “The Talk” Isn’t Working (By Itself)
Let’s be clear: open communication is a critical protective factor. But it’s not a shield. The most common assumption parents make is that their teen either “isn’t active yet” or will tell them if something goes wrong. In reality, many teens avoid bringing up sex because they feel pressure to maintain the image of being responsible, even if they’ve already taken risks.
“We told our daughter she could always come to us,” said one mother of a 15-year-old recently diagnosed with HPV. “But I think that actually made her feel like she had to keep proving she didn’t need to.” In some families, even positive, supportive messaging can be interpreted as pressure not to mess up.
There’s also a timing problem. Many parents wait for “the right time” to bring up testing, but that time often comes after the fact. Teens rarely volunteer details about sexual activity in real time. They may also not understand what counts as a risk: fingers, oral sex, even rubbing without penetration can still spread STDs like herpes or HPV.
The chart below breaks down the most common misalignments between what parents assume and what’s actually happening:
| Parent Assumption | Teen Reality |
|---|---|
| “They’d tell me if they had sex.” | Teens often conceal activity to avoid changing how parents see them. |
| “We already talked about condoms and protection.” | Teens may use condoms inconsistently, or not at all during oral or first-time encounters. |
| “They know the risks.” | Knowing isn’t the same as applying in the moment, especially under pressure or while drinking. |
| “They’d recognize symptoms if they had them.” | Most teens don’t know what early STD symptoms look like, or that they can be asymptomatic. |
Table 1. The Gap Between Parent Assumptions and Teen Realities in STD Awareness and Risk.
The Testing Problem: Access, Shame, and False Reassurance
Even if your teen knows they should get tested, actually doing it is another story. Clinics may feel intimidating. School nurses may not be equipped to refer for testing. Teens may fear being judged by providers, or worse, having their results show up in shared family insurance portals. In many states, teens can legally access STD testing without parental consent, but they don’t always know how or where to go. And if they use a family insurance plan, explanation of benefits (EOB) letters can out them unintentionally.
That leaves many teens turning to the internet, or doing nothing. A 2022 study from the Journal of Adolescent Health found that over 40% of sexually active teens had never been tested for STDs. Among those who were tested, nearly half delayed because they were “waiting to see if symptoms developed.”
This delay isn’t just risky, it’s based on a fundamental misunderstanding. Many teens believe that no symptoms = no infection. Others assume they were protected because it was “just once” or because they used a condom. But condoms don’t prevent skin-to-skin STDs like herpes or HPV if lesions are outside the covered area. And “just once” is more than enough for transmission to happen.
Check Your STD Status in Minutes
Test at Home with RemediumPapillomavirus (HPV) Test

 For Women
For Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $33.99 $49.00
Why Even “Good” Teens Take Risky Chances
The myth that teens who “know better” always make safer choices is deeply flawed. Adolescents are neurologically wired to prioritize short-term rewards over long-term consequences. That’s not a character flaw, it’s neuroscience. The prefrontal cortex, which governs decision-making and impulse control, isn’t fully developed until the mid-20s. This means even the most well-informed teens can freeze in the moment, follow peer pressure, or simply forget what they were taught.
Kayla, 18, had straight As and a college scholarship lined up. She and her girlfriend decided to have sex for the first time and assumed there was no risk because they were both “girls.” Neither had been tested. Two months later, Kayla tested positive for chlamydia after developing pelvic pain. Her partner had no symptoms but was positive too. “We weren’t trying to be irresponsible,” Kayla said. “We just didn’t know we needed to test.”
Sexual education often glosses over queer relationships, same-gender risks, and oral or digital contact, all of which can transmit infections like gonorrhea, herpes, and HPV. When teens don’t see themselves represented in the risk messaging, they assume they’re exempt. And when they do take risks, they often tell no one, especially if they fear disappointing their parents.
This disconnect between education and application isn’t just about knowledge gaps. It’s about fear, shame, and the immense social stakes of being “the one with something.” That’s why testing options that preserve privacy and dignity are essential, not just in public clinics, but at home.
What Testing Actually Looks Like (And When It Should Happen)
STD testing isn’t one-size-fits-all. Some infections have longer window periods than others, meaning a test taken too early may miss the infection. Others, like herpes, may not be included in standard panels unless specifically requested. And in many cases, teens have no idea what to ask for, or if they're even asking the right questions.
The table below outlines typical window periods and optimal testing timelines for common STDs affecting teens. This is crucial when advising your teen on when to test after a hookup, new partner, or any exposure concern.
| STD | Earliest Detectable | Best Testing Time | Sample Type |
|---|---|---|---|
| Chlamydia | 7 days | 14 days | Urine or genital swab |
| Gonorrhea | 5 days | 14 days | Urine or genital/throat/rectal swab |
| Trichomoniasis | 5 days | 7–14 days | Urine or vaginal swab |
| Syphilis | 3 weeks | 6–12 weeks | Blood test |
| HIV | 10–14 days (RNA) | 28+ days (Ag/Ab) | Blood or oral fluid |
| Herpes (HSV-1/2) | 4–6 weeks | 12 weeks (if asymptomatic) | Blood or swab if sores present |
Table 2. Typical window periods and optimal testing times for common teen STDs.
If your teen is already sexually active, or even if you suspect they may be, it’s better to normalize periodic testing rather than wait for a symptom to appear. Even one sexual encounter can warrant testing depending on the activity and exposure. The more comfortable you make it to ask, test, and talk, the more likely your teen is to stay proactive.
When Privacy Matters More Than Ever
Teens often say nothing because they’re terrified of being judged, exposed, or punished. One of the most empowering things a parent can do is separate concern from control. This might mean offering to help them test privately, or stepping back and letting them test without you at all.
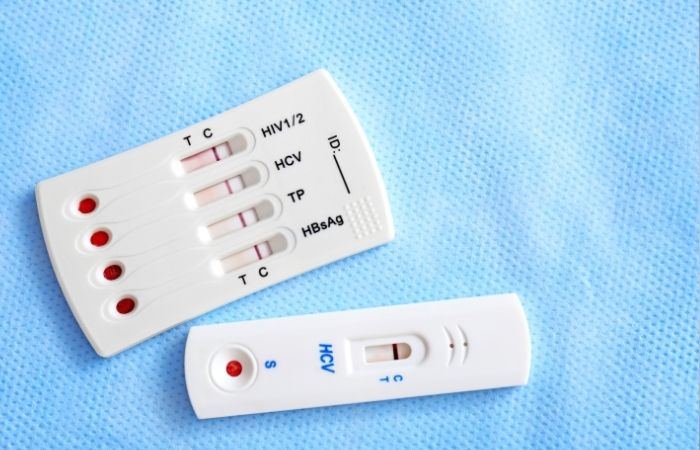
At-home testing kits have become a game changer for adolescent sexual health. Many options allow teens to collect samples themselves (urine, swabs, or finger-prick blood) and mail them off with no clinic visit required. Some offer results in 24 to 72 hours, with telehealth follow-up for treatment referrals. Others offer rapid results at home in minutes, like pregnancy tests, but for infections like HIV or syphilis.
These kits remove two major barriers: fear of being seen and fear of being judged. Teens don’t have to ask permission, make an excuse, or walk into a waiting room. And as a parent, encouraging this kind of discreet, self-led testing can build lifelong sexual health habits based on autonomy, not fear.
If you want to make this an option in your home, introduce it casually. Keep kits in a bathroom cabinet. Let your teen know they’re available. Say something like: “You never have to tell me if you use one. I just want you to have choices.” The message is clear: their health matters more than your comfort.
People are also reading: How Soon Will Gonorrhea Symptoms Start? A Real Timeline
The Emotional Fallout No One Prepares You For
Getting an STD diagnosis can be devastating for a teen, not just physically, but emotionally. It may be their first major encounter with shame, fear of being “damaged,” or terror about having to tell a partner. Some may spiral into silence or depression. Others may act like it’s no big deal but secretly carry the weight alone.
One 16-year-old shared anonymously: “I was so scared to tell anyone. I felt dirty, even though I know it’s common. I thought if my mom found out, she’d never look at me the same.” This kind of emotional burden is what often keeps teens from testing in the first place.
As a parent, your role here is not to correct, shame, or even advise right away. It’s to listen. To breathe. To thank them for trusting you. And then to help them get care. This isn’t about what went wrong, it’s about what comes next.
In most cases, STDs are treatable. Some, like chlamydia and gonorrhea, can be cleared with a single dose of antibiotics. Others, like herpes or HPV, may be chronic but manageable, and increasingly common. The goal is not to scare them into abstinence, but to help them understand how to protect themselves and others moving forward.
Normalizing treatment, follow-up testing, and partner notification as acts of maturity, not shame, is one of the most powerful shifts you can make in your home.
Turning Panic Into Power: What Teens Actually Need
When a teen confides in you, or when you suspect they’re at risk, the gut reaction is often panic. But what they need in that moment isn’t more fear. They need a plan. And they need to feel like they’re not broken, not dirty, not “bad.” They need to know that this doesn’t define them. It just means they’re human. Learning how to test, treat, and move forward is part of growing up, especially in a world where hookup culture, misinformation, and early sexual experimentation are the norm.
This is where testing becomes a tool of empowerment, not punishment. It tells your teen: you deserve answers. You deserve peace of mind. You deserve a healthy body and the confidence to take care of it. Whether it’s their first encounter or they’re already navigating relationships, offering options for safe, confidential testing is a concrete way to shift from fear to action.
This at-home combo test kit checks for the most common STDs teens are likely to encounter, discreetly, quickly, and without clinic lines. Results are available in minutes, and teens can test from their own bathroom, no awkward explanations needed. For many, that’s the difference between getting tested and doing nothing.
If your teen isn’t ready to talk but you suspect something’s going on, you can still open the door. Leave a kit in a shared space. Send them a link with a simple message: “No judgment. Just in case.” Make testing feel like care, not confrontation.
How to Normalize STD Testing in Your Home
You brush your teeth. You wear a seatbelt. You go to the dentist once a year. STD testing should be no different. But teens don’t grow up thinking that way, unless someone shows them how. Here’s what that could look like in real life:
A mother of two keeps test kits in the linen closet next to the Tylenol. “If you ever need it,” she told her kids, “it’s there. No questions asked.” A father puts a post-it on the fridge with a QR code to an at-home testing site. A stepmom casually brings up that she got tested after her last relationship ended and says, “It’s just basic self-care, like getting your eyes checked.”
These aren’t big speeches. They’re small signals that say: this is normal. You’re not in trouble. We want you safe.
Some families create a routine: test once a year, just like a physical. Others make it partner-based: new partner, new test. However you do it, the goal is consistency. That builds trust. That breaks shame. That’s how you create a household where sexual health is just part of health.
And if your teen tests positive? Treat it the same way you’d treat strep throat or a broken toe. No lecture. Just next steps. That one reaction can shape how they view their body, their worth, and their ability to bounce back.
Check Your STD Status in Minutes
Test at Home with Remedium3-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $69.00 $147.00
For all 3 tests
What If They Don’t Want to Talk About It?
Sometimes you know something’s off, but your teen shuts down. They dodge questions. They change the subject. They roll their eyes. That doesn’t mean you’ve failed. It just means they’re still learning how to hold space for vulnerability, and that takes time.
If your teen isn’t ready to talk, try changing the question. Instead of “Have you had sex?” try “Have you ever felt unsure if something was safe?” Instead of “Are you being careful?” ask “Do you feel like you have the right info?” Instead of “Do you need to get tested?” offer “Would you want to do it privately, without having to tell me?”
Language matters. Timing matters. But what matters most is that they know the door is always open, and that nothing they say will make you love them less. That’s the foundation where real prevention lives. Not in fear, but in trust.
Even if you think they’re not ready, give them tools anyway. A link. A kit. A note. A reassurance: “If you ever need help, I’ve got you.”
FAQs
1. Can you really get an STD from oral sex?
Yes, absolutely, and that surprises a lot of people. Infections like herpes, gonorrhea, and even syphilis can pass through oral sex. A sore throat that won’t go away after a hookup? It might not be strep. Many teens think “just oral” means no risk, but if there’s skin-to-skin contact or fluid exchange, there’s a risk.
2. My teen swears they’ve only had sex once, should they still get tested?
One time is all it takes. That’s not fear talk, it’s just biology. STDs don’t care about your intentions or track record. Even if it was a one-time thing and protection was used, testing is still a smart move, especially if it brings peace of mind. There’s no minimum number of partners for an STD to show up.
3. Is it true that most teens with STDs don’t even know it?
Sadly, yes. Most common STDs, like chlamydia or trichomoniasis, don’t throw up obvious red flags. No pain, no sores, no dramatic symptoms. That’s how they spread so easily. A teen can feel totally fine and still be positive. Testing is how you find out, guessing won’t cut it.
4. Can my teen get tested without telling me?
Legally, in most places, yes. But the real issue isn’t legality, it’s logistics. Teens can go to clinics on their own, but what scares them is being judged, seen by someone they know, or having test info show up in your insurance mail. That’s why at-home test kits are game-changers. No lines. No eyes. Just answers.
5. How soon should they test after a hookup?
It depends on what they were exposed to. Some STDs can be detected in as little as 5–7 days. Others take weeks. The sweet spot for most infections? Around 14 days. But retesting later, at 6 weeks or so, can catch anything that didn’t show up early. Testing once and calling it done too soon is a common trap.
6. Are those at-home STD kits even accurate?
The short answer: yes, if it’s a good one. Many at-home tests use the same lab technology as clinics (we’re talking about things like NAAT, which is highly accurate). Some are rapid, others are mail-in. Follow the directions, and the results are solid. Just make sure you’re using a kit from a reputable source, not something sketchy off a random site.
7. What do I do if my teen tests positive?
Breathe first. Then thank them for telling you. Seriously. That kind of honesty is rare, and brave. Next? Get them care, some infections need antibiotics, others need monitoring. Remind them they’re not “gross” or “ruined.” They’re just a person who got something common and treatable. You wouldn’t shame them for strep throat, so don’t do it here.
8. Should teens test even if they have no symptoms?
Yes, yes, and yes again. No symptoms means nothing in STD world. Especially for teens, who often don’t know what to look for, or assume irritation or discharge is “just hormones.” If they’re sexually active in any way, oral, digital, vaginal, whatever, regular testing is part of taking care of themselves.
9. Which STDs should a teen be tested for?
Start with the big five: chlamydia, gonorrhea, syphilis, HIV, and trichomoniasis. If there are symptoms like sores, test for herpes too. And remember, HPV might not be on standard panels, it’s often caught during Pap tests. A combo test kit usually covers the key bacterial STDs and is a great starting point.
10. What if my teen lies about being sexually active?
Welcome to parenting a human. It’s not about catching them in a lie, it’s about keeping the door open. If you suspect something, skip the interrogation. Say, “If you ever need to test, there’s a kit in the bathroom. No questions asked.” That one move can do more than a thousand lectures.
You Deserve Answers, Not Assumptions
You’ve done the hard part, you’ve had the conversations. You’ve opened the door. Now it’s time to go a step further. The truth is, even in the most communicative homes, silence still wins when shame is stronger than support. Testing, prevention, and care can’t just be abstract ideas, they have to be concrete, available, and judgment-free.
Your teen doesn’t need another lecture. They need a plan. They need a private path to answers. And they need to know that if the result is positive, they’re not alone, they’re not ruined, and they’re not in trouble. They’re just human. And being human means having tools, options, and love, no matter what the test says.
Don’t wait and wonder, get the clarity you deserve. This at-home combo test kit checks for the most common STDs discreetly and quickly.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted six of the most relevant and reader-friendly sources.
Sources
1. Planned Parenthood: STDs, HIV, and Safer Sex
2. NHS: STIs Overview and Testing
3. Sexually Transmitted Infections Surveillance, 2024 | CDC
4. STI Testing and Youth Risk | CDC Healthy Youth
5. Sexually Transmitted Infections among Young Americans | CDC NPIN
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist who works to stop, find, and treat STIs. He combines clinical accuracy with a straightforward, sex-positive attitude and is dedicated to making his work available to more people, both in cities and in rural areas.
Reviewed by: S. Langford, NP | Last medically reviewed: December 2025










