Quick Answer: Yes, you can get an STD without having sex. Herpes, HPV, syphilis, and even hepatitis B can spread through skin contact, shared objects, or close non-sexual exposure. Not every risk is high, but some are real, and worth understanding.
The Truth About Non-Sexual Transmission
STDs, more accurately called STIs (sexually transmitted infections), aren’t always transmitted through sex. They’re transmitted through contact. And contact comes in a lot of forms: kissing, rubbing, sharing, giving birth, even just living in close quarters with someone who has an active infection.
The idea that STDs only spread through sex is not just wrong, it’s dangerous. It leaves people vulnerable, confused, and more likely to pass infections on without ever knowing they were at risk.
Let’s walk through the non-sexual ways STDs actually spread, and where the myths end and real risks begin.

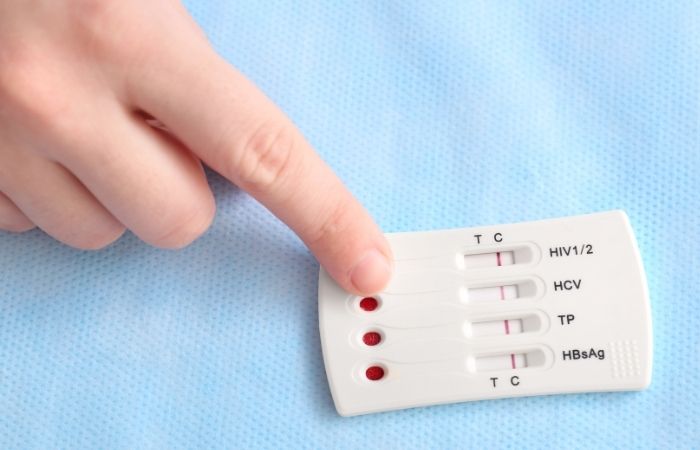
People are also reading: HIV Rapid Test vs Lab Test: What’s More Accurate and When?
STD Transmission Without Sex
This chart breaks down which STDs can spread without sex, how they’re transmitted, and what the real-world risk is.
| STD | Non-Sexual Routes | Transmission Risk |
|---|---|---|
| Herpes (HSV-1, HSV-2) | Kissing, skin contact, sharing lip balm or razors | High (during shedding or outbreaks) |
| HPV | Skin contact, shared sex toys | Moderate to high (even with no symptoms) |
| Syphilis | Skin contact, open sores, kissing (oral) | High (if sores are present) |
| HIV | Shared needles, blood-to-blood, birth | Low without blood exposure, high with it |
| Hepatitis B/C | Shared razors, needles, blood contact | Moderate to high |
| Chlamydia / Gonorrhea | Oral exposure, childbirth | Low (non-sexual), high during birth |
Table 1. Common STDs with non-sexual transmission routes and their associated risk levels.
Ways STDs Can Spread Without Sex
Sex isn’t the only route for infection. STDs are opportunists, they’re looking for access, not intimacy. Below are the most common non-sexual ways these viruses and bacteria spread, from everyday skin contact to shared items and beyond. Some are rare. Others are surprisingly easy to miss. Let’s break it down.
Skin-to-Skin Contact (No Fluids Required)
This one trips people up the most. Some of the most common STDs don’t require intercourse, ejaculation, or any fluids at all, they just need skin. Herpes (HSV-1 and HSV-2), HPV, syphilis, and molluscum contagiosum can all spread through simple skin contact, especially if there’s a sore or abrasion present.
That means dry humping, hand stuff, or even cuddling naked during an outbreak can spread the virus. You don’t need penetration. You just need proximity, and active shedding of the virus.
Herpes, in particular, is a master of this. It sheds invisibly, even when no symptoms are visible, and can infect others through contact with the mouth, genitals, buttocks, or inner thighs.
Kissing and Oral Contact
Kissing is often dismissed as innocent, but it’s actually a well-documented way to spread certain STDs, especially HSV-1 (oral herpes). If someone has an active cold sore, or even just viral shedding, kissing, licking, or sharing drinks can pass the virus on.
Gonorrhea, syphilis, and even chlamydia can also live in the throat. That means if you’re engaging in deep kissing, especially with multiple partners or someone with an untreated infection, transmission is possible, even if you're not having any other kind of sex.
Example: someone has gonorrhea of the throat but no symptoms. They kiss or perform oral sex. The bacteria spreads to their partner’s throat, genitals, or rectum, without anyone realizing a thing.
Shared Razors, Towels, and Personal Items
Most STDs don’t survive long on surfaces, but some exceptions exist. Bloodborne viruses like HIV, hepatitis B, and hepatitis C can survive outside the body for hours to days, especially in tiny amounts of blood left on razors, needles, or toothbrushes.
If you’re sharing a razor with someone who has hepatitis C, and you nick yourself, you’ve just created an open door for the virus. This is rare, but it happens, especially in close-living households, dorms, or among siblings.
Towels, on the other hand, are mostly not an STD risk. They might spread fungal infections or skin bacteria, but STDs like herpes or chlamydia don’t typically survive that way. Still, if the towel is visibly soiled or was used on open sores? Play it safe.
Childbirth and Vertical Transmission
Some STDs don’t just move horizontally between adults, they also move vertically, from parent to baby. During pregnancy, labor, or breastfeeding, viruses like HIV, syphilis, herpes, chlamydia, and gonorrhea can be passed from an infected parent to a newborn.
That’s why prenatal testing matters. A person can carry an STD for years without symptoms, only to find out during a routine screen that they’ve had herpes or syphilis all along. Most of the time, treatment can prevent transmission to the baby, but only if the infection is caught early.
Fun fact: many babies born with herpes got it not because the parent knew they had it, but because no one recognized the signs, and no one tested in time.
Blood and Open Wounds
This category matters for hepatitis B, hepatitis C, and HIV. These viruses spread through blood, and while sexual contact is the most common route, it’s not the only one. Shared needles (including for tattoos or piercings), blood transfusions (in rare or unscreened cases), or even contaminated medical tools can all spread these infections.
It’s also possible, but rare, for transmission to occur if someone with an active infection bleeds onto another person’s broken skin or mucous membranes. This risk is very low in everyday settings but higher in healthcare or high-exposure environments.
STDs are called "sexually transmitted" because that’s how most people get them, not because it's the only way.
Check Your STD Status in Minutes
Test at Home with Remedium3-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $69.00 $147.00
For all 3 tests
Scenarios Where Non-Sexual Transmission Gets Overlooked
You don’t need to be sleeping around to be at risk. Plenty of people contract STDs while thinking they’re “playing it safe.” That’s because most people don’t realize how easily certain infections can travel, especially in environments where skin, saliva, or shared objects come into play.
Let’s look at some real-world scenarios where STDs can (and sometimes do) spread without sex, and why people don’t always connect the dots.
Roommates and Shared Bathrooms
Two friends share a house. One borrows the other’s razor to touch up their bikini line. Days later, they notice a red bump. It hurts. It crusts. They assume it’s an ingrown hair. But it happens again… in the same spot. Turns out, the roommate had HSV-2, and the razor wasn’t just sharp. It was contagious.
Shared razors are a common but overlooked risk for herpes, hepatitis B, and hepatitis C. These viruses can survive on the blade for hours, or longer, especially if there’s blood involved.
Parents and Kids
A toddler develops a small sore near their mouth. The pediatrician suspects impetigo, but the culture comes back positive for HSV-1. The source? Possibly a kiss on the lips from a relative with an active cold sore.
Many kids get herpes this way, no sex, no trauma, just routine affection from someone shedding the virus. It doesn’t mean abuse. It means viruses don’t care about intentions.
“Not Sex” Hookups
Two people engage in a no-penetration encounter, just oral, manual, and some heavy skin-to-skin contact. No fluids exchanged. No condom used. One of them ends up with genital warts a few weeks later. That’s how HPV spreads: through skin, not fluids.
Just because you didn’t go “all the way” doesn’t mean you didn’t share enough contact to pass an infection.
Toilet Seats, Hot Tubs, and Other Myths
Okay, let’s get this out of the way:
You’re not going to catch an STD from a toilet seat.
Viruses like herpes, chlamydia, and gonorrhea don’t survive long on cold, dry surfaces. Toilet seats are public enemies in our imagination, but they’re not real transmission risks. Same goes for hot tubs, chlorinated water kills most pathogens, and dilution makes infection nearly impossible.
But that doesn’t mean every surface is harmless. If someone with herpes sits on a shared bench at the gym with an open sore and you sit down seconds later with broken skin? Technically possible, but still rare.
Here’s the difference:
- Toilet seats = low to zero risk
- Razors, needles, or toothbrushes = real risk (if blood is involved)
- Skin-on-skin contact with active sores = very real risk
Knowing where the actual danger lies helps you stay alert without spiraling into germaphobia.
Why People Miss These Infections
Part of what makes non-sexual transmission so tricky is that it’s invisible. You don’t notice when someone else’s herpes is shedding. You don’t feel a virus jump from a shared razor. You just get a bump days later and try to remember what happened.
By then, it’s hard to connect the dots. Especially if you haven’t had sex recently, or ever. Many people who get herpes or HPV in “non-sexual” ways end up blaming themselves, wondering if they were irresponsible, dirty, or doing something wrong. But they weren’t. They just weren’t informed.
STDs aren’t just about sex. They’re about exposure. And some forms of exposure happen in everyday life, not just the bedroom.
Risk vs. Reality – Should You Worry?
This table breaks down common fears around non-sexual STD exposure, and whether they’re based on real risk or just anxiety-fueled myths.
| Scenario | STD Risk Level | Why (or Why Not)? |
|---|---|---|
| Using a public toilet seat | None | Viruses can't survive on dry, hard surfaces long enough to infect you. |
| Sharing a razor | Moderate | Risk of hepatitis B/C or herpes if there's blood or skin residue. |
| Kissing someone with a cold sore | High | HSV-1 spreads easily through saliva, even without visible sores. |
| Receiving oral sex | High | Oral gonorrhea, chlamydia, herpes, and HPV can be transmitted this way. |
| Hot tub use | Low to None | Chlorine kills most pathogens; no realistic STD transmission route. |
| Sharing towels | Very Low | Most STDs don’t survive long on fabric; risk is near-zero unless visible sores present. |
| Giving birth | High (for some STDs) | Herpes, HIV, and others can pass to baby during labor if untreated. |
Table 2. Clarifying the actual risk levels behind common non-sexual exposure fears.
Testing Even If You’re Not “At Risk”
Here’s a quiet truth: a lot of people never test for STDs because they think they don’t need to. They’re not sexually active, or they haven’t had a new partner in years, or they always use protection. But protection doesn’t cover skin contact. And “not active” doesn’t mean “never exposed.”
If you’ve ever shared razors, kissed someone with a cold sore, had oral sex, or been born to a parent with an untreated infection, you’ve been in contact with STD transmission routes.
At-home testing makes this easy. You can get peace of mind without the shame spiral. No appointments. No sideways glances. Just a few drops of blood or a simple swab and you’ll know exactly what you’re dealing with.
The Herpes 1 & 2 Rapid Test Kit is a great place to start if you’ve had unexplained bumps, oral outbreaks, or suspect past exposure. It tests both HSV-1 and HSV-2, even if you’re not showing symptoms right now.
People are also reading: Can You Have an STD and Not Know It? Here’s What to Watch For
Why “Non-Sexual” STDs Still Carry So Much Stigma
Here’s the kicker: even when someone gets an STD in a completely non-sexual way, sharing a razor, receiving oral sex, childbirth, they still feel ashamed. Why? Because we’ve been conditioned to link STDs with irresponsibility, promiscuity, or moral failure.
So when someone gets herpes from a childhood kiss or HPV from one partner’s skin contact, they don’t just feel confused, they feel dirty. People who’ve never even had intercourse have sat in clinics wondering how they could explain an STD diagnosis to a doctor, let alone a partner.
The truth is, viruses don’t care how you feel about your body count. They care about opportunity. And skin contact, saliva, blood, and childbirth? Those are all opportunities. What you did or didn’t do in bed doesn’t change the biology.
Real People, Real Transmission Stories
Niko, 24: “I had never had sex, like, at all. But I had what I thought was razor burn after the gym. It kept coming back. Finally got it swabbed and found out it was HSV-2. Turns out, I probably got it from using my roommate’s razor. I was furious, and embarrassed. But also... kind of relieved to finally know.”
Janessa, 38: “I thought I was safe because I was married and monogamous. But my partner had a cold sore years ago and gave me HSV-1 through oral sex. When I got a genital outbreak, I didn’t even know herpes could work that way.”
Mei, 19: “My mom had hepatitis B when I was born. I never got symptoms. I found out in college during a blood test and was shocked. Nobody ever explained that to me growing up.”
These are just a few examples of how STDs creep into people’s lives, not through risky choices, but through ordinary ones.
Rethinking “Exposure” in a Sex-Obsessed Culture
We live in a culture that talks about sex constantly, but still treats STDs like taboo punishments. As a result, we’ve built this myth that if you get an infection, you must’ve done something wrong. But exposure doesn’t always mean sexual activity, and “clean” doesn’t mean “immune.”
We need better language. Instead of asking, “Are you sexually active?”, what about, “Have you ever shared close contact, or had any skin-to-skin intimacy?” Instead of assuming teenagers only need sex ed about condoms, maybe we include content on skin-based viruses, oral risks, and non-sexual transmission.
That shift could help prevent the quiet spread of these infections, and the shame that keeps people from speaking up.
How to Protect Yourself (Even If You’re Not Having Sex)
You don’t need to be celibate to stay safe. And you don’t need to be sexually active to get smart about prevention. Here’s what protection looks like when we expand the definition of exposure:
- Don’t share razors, toothbrushes, or anything that might have blood/saliva on it.
- Ask about cold sores before kissing. They’re herpes, even if they’ve been normalized.
- Use barriers during oral sex (like condoms or dental dams), especially with new partners.
- Get tested regularly, especially before new relationships or after unexplained symptoms.
- Talk about more than “just” intercourse. Skin contact counts. Oral counts. So does close cuddling during outbreaks.
Protection isn’t just about prevention, it’s about knowing. And knowing puts you back in charge of your health.
Check Your STD Status in Minutes
Test at Home with Remedium7-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $129.00 $343.00
For all 7 tests
FAQs
1. Can you really get an STD without having sex?
You can, and people do. Herpes from a kiss. Hepatitis from a shared razor. HPV from skin-to-skin contact during a clothes-on grind. Sex isn’t the only door these viruses walk through.
2. Wait, so kissing is actually risky?
When cold sores are involved? Definitely. That’s oral herpes (HSV-1), and it doesn’t care how sweet or innocent the kiss felt. If they’ve got it, especially during an outbreak, it can spread to your mouth, or even genitals during oral.
3. I thought I was safe because it was “just oral.”
A lot of people think that. But oral sex can still transmit herpes, HPV, gonorrhea, and even syphilis. It doesn’t need to be penetrative to carry risk. And “clean” looking doesn’t mean infection-free.
4. Is it true you can catch something from a razor?
Yep, especially when blood’s involved. Herpes, hepatitis B, hepatitis C, if someone with an infection nicks themselves and you use the same blade and cut yourself after? That’s a viable transmission route.
5. So what about towels? Do I need to panic?
Relax. Most STDs can’t survive on fabric. Unless it’s visibly gross, freshly used on open sores, and you rubbed it into a wound, the risk is practically zero. Just don’t share towels regularly, especially in outbreak-prone households.
6. My baby got tested for herpes. Could it be from me?
It’s possible. HSV can be passed during delivery or even from a kiss after birth if you had a cold sore. It doesn’t mean you’re a bad parent, it means these viruses are sneaky. That’s why prenatal and pediatric testing matters.
7. I haven’t had sex in years. Why would I need an STD test?
Because some infections hang out silently. You could’ve been exposed years ago and never had symptoms. Or maybe it was oral sex, or sharing a razor, or a partner’s cold sore. You don’t need a “body count” to justify getting answers.
8. Are toilet seats really safe?
Yes. Truly. Viruses like herpes and chlamydia don’t survive long on cold, dry surfaces. It’s time we let that myth die. You’re way more likely to get an STD from someone’s lips than from a toilet seat.
9. Do condoms help if it’s not sex-sex?
They help a lot, but they’re not a forcefield. Herpes and HPV can live on areas outside of what a condom covers. So while they reduce risk, they don’t erase it, especially if there’s skin-to-skin grinding or oral contact involved.
10. How do I know if that bump was herpes or just an ingrown hair?
Good question. If it burned, blistered, crusted, came back in the same spot, or showed up after a skin-to-skin encounter, test. You can use a swab if the bump’s still there, or an at-home herpes test if it’s not.
Let’s Stop Pretending STDs Only Happen One Way
You don’t need a wild sex life to catch an infection. You don’t even need to have sex. That’s the uncomfortable truth most people aren’t told until it’s too late.
Non-sexual transmission is real. And more common than we think. From casual contact to shared razors, these viruses don’t check your relationship status, they check for opportunity. And if we only protect ourselves during intercourse, we’re leaving the back door wide open.
It’s not about fear. It’s about clarity. If you’ve had oral sex, shared a razor, kissed someone with a cold sore, or just aren’t sure what that bump was last month, get tested. Quietly, privately, on your own terms.
Get tested at home in minutes with Rapid STD Test Kits. No awkward conversations. No judgment. Just clarity, finally.
How We Sourced This Article: This article was built using up-to-date clinical research, CDC and WHO guidance, and firsthand accounts from patients and clinicians navigating real-world STD exposure. Around fifteen reputable sources shaped this article; below, we’ve highlighted some of the most relevant and reader-friendly ones.
Sources
1. WHO: Herpes Simplex Virus Overview
2. WHO — Herpes Simplex Virus Fact Sheet
4. Genital Herpes: Review of the Epidemic and Potential Use of Type-Specific Serology — PMC
5. Shedding Patterns of Genital Herpes Simplex Virus Infections — JAMA
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist who writes and consults on sexual health, stigma reduction, and accessible diagnostics. He believes knowledge should be free of shame, and testing should be as easy as brushing your teeth.
Reviewed by: E. Cruz, RN | Last medically reviewed: October 2025
This article is for educational purposes and does not substitute medical advice.










