Quick Answer: A barely visible line in a chlamydia rapid test is usually positive, but confirmatory test may still be necessary. It may be due to an early infection, low bacterial load, or end-user error. Retesting or confirmatory laboratory test is, in such cases, the best follow-up procedure.
Why This Confuses So Many People
You’re not the only one staring at a faint line like it’s a message from another dimension. The truth is, interpreting at-home STD test results can be emotionally loaded, especially when they’re not crystal clear. Many rapid chlamydia tests use a cassette format similar to a pregnancy test, one line means the test worked (the control line), and a second line means the test has detected chlamydia antigens. But what happens when that second line is barely visible?
Marcus, 24, found himself squinting at his test result in the dim light of his dorm bathroom.
“It was just a shadow, like someone had taken a pencil and lightly sketched a line,” he said. “I didn’t know if I should be panicking or not.”
That ambiguity isn’t rare, and it’s not your fault. Lighting, timing, and even humidity can affect how results appear. But the emotional toll? That’s real. You feel like your entire sex life hangs in the balance of a half-formed pink line.
Rapid tests are designed to be user-friendly, but they’re not immune to interpretation issues. You might be dealing with a low bacterial load that produces a faint signal. Or the swab didn’t collect enough material. Or maybe you peeked at the test before the full development time, then rechecked too late. It’s not just about reading the line, it’s about reading it at the right time, under the right conditions.

People are also looking for: I Took the Pills, Do I Still Need Another STD Test?
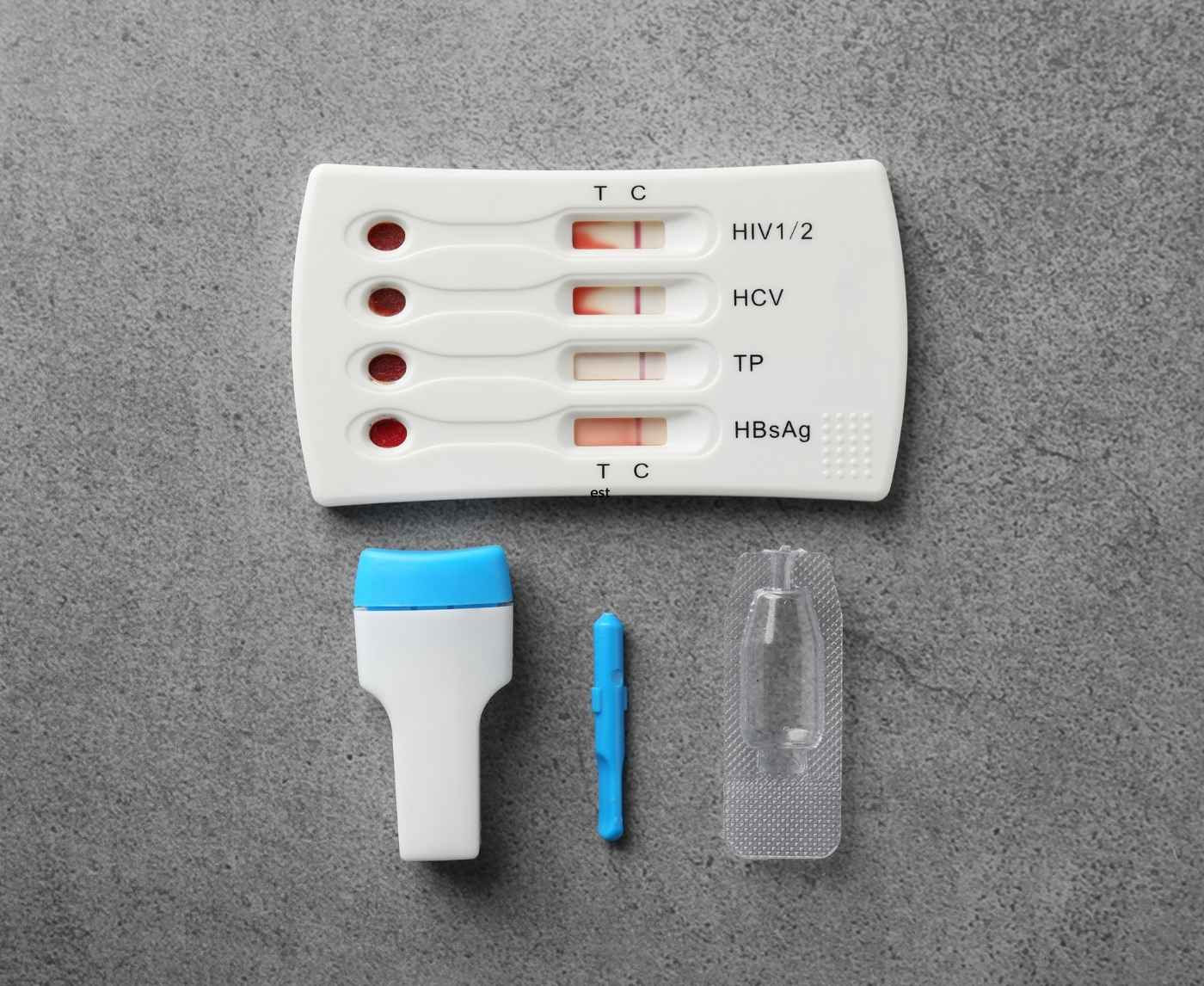
What Comes Inside a Chlamydia Rapid Test Kit?
Before you even open the foil pouch, it’s helpful to know what you’re working with. A typical at-home chlamydia test kit includes a sterile collection swab or dropper, a small buffer solution bottle, a plastic test cassette, and an instruction leaflet. Some kits include a timing card or QR code for video guidance.
Storage matters. That box under your bathroom sink? Not ideal if it’s exposed to heat or moisture. Most test kits need to be stored at room temperature, think 59–86°F (15–30°C). If the test has expired or been frozen, results may be invalid before you even begin.
| Component | Purpose | Notes |
|---|---|---|
| Swab or Dropper | Collects urine or vaginal/urethral fluid sample | Handle with clean hands; don’t touch tip |
| Buffer Solution | Extracts and stabilizes chlamydia antigen | Don’t spill or contaminate |
| Test Cassette | Shows control and result lines | Keep flat and level during use |
| Instructions | Guides correct steps and timing | Always read before starting, even if you’ve done it before |
Table 1: Standard components of a chlamydia home test kit. Handle all parts with clean, dry hands and follow kit-specific timing instructions.
Step-by-Step: How to Do the Test Properly
You’ve got the kit. You’re ready. Now slow down. Most mistakes happen not out of carelessness, but because we’re nervous. Maybe it’s the first time you’ve tested. Maybe someone ghosted you after a hookup and you’re spiraling. Maybe your partner just told you they tested positive and now your hands are shaking. It’s okay. This part is manageable.
Start by washing your hands and choosing a clean, dry surface to work on, ideally not right next to your toilet or in a steamy shower area. Lay out everything in front of you. If the instructions mention a buffer bottle, open it carefully and don’t touch the nozzle. Collect your sample exactly as described: insert the swab just enough to collect a proper vaginal, urethral, or urine sample, depending on the kit type. Then place it into the buffer or apply the drops according to the kit’s directions.
Place the test cassette on a flat surface and start the timer. Most tests require 10–15 minutes to develop. Do not read the result before the stated time, and don’t wait too long either, past 20–30 minutes, the lines may fade or change, leading to false interpretations.
Naya, 32, did everything right, except she forgot to set a timer.
“I came back after 40 minutes and the line was dark,” she said. “Then I Googled and realized that it might be an evaporation line. I had to retest two days later.”
The key here is timing, hygiene, and careful observation. Lighting matters. Read the result under bright, natural light if possible, not fluorescent bathroom bulbs or tinted phone flashlights.
Interpreting the Lines: Clear vs. Faint vs. Invalid
This is the moment everything hinges on. You stare at the cassette and see two lines, but that second one is barely there. Here’s what’s happening: most chlamydia rapid tests detect surface antigens from the Chlamydia trachomatis bacteria. A darker second line means more antigen is present; a faint line often means there’s less antigen, but it’s still likely present.
| Line Appearance | Likely Interpretation | What to Do Next |
|---|---|---|
| No control line, no test line | Invalid test | Retest with new kit |
| Control line only | Negative result | If tested too early, retest in 1–2 weeks |
| Control line + faint test line | Possible positive | Retest or confirm with lab test |
| Control line + clear test line | Positive result | Seek treatment and notify partners |
Table 2: Visual guide to interpreting rapid chlamydia test results. Faint lines are common and often signal a low-level infection, not a testing error.
However, not all slight lines constitute actual positives. Now and then, leftover dye, evaporation, or incorrect storage will produce an "illusory" line. If the test was left out for too long before or after its use, or if the buffer solution was not properly mixed, you may end up with puzzling findings. That's why numerous health professionals suggest confirming faint results with either retest in 3–5 days or a NAAT/PCR lab test, in the case of persistent symptoms or recent exposure.
When the Result Doesn’t Seem to Make Sense
You've followed every step. Waited the right amount of time. Stared down that cassette like it owed you something, and still, you can’t tell if it’s positive or just a trick of the light. That’s when the frustration kicks in. You start doubting not only the test but yourself. Did you do something wrong? Is the test expired? Was that swab even enough?
Sometimes, the test result doesn’t fall neatly into “positive” or “negative.” You may see smudges, streaks, or lines so faint they disappear when you tilt the cassette. That doesn’t mean you’re broken or paranoid. It means you’ve entered what many at-home testers call the “gray zone”, a place where anxiety thrives, but answers don’t come easy.
Erin, 28, tested after a breakup with someone she later learned had cheated.
“The test line was barely visible. I stared at it for ten minutes straight, Googling photos and message boards. I felt more lost than before I tested.”
Her story’s not rare. People want clear answers, and a vague result can make the shame and fear worse.
Here’s what to remember: rapid tests are incredibly useful, but they’re also sensitive. And sometimes, sensitivity works against clarity. That’s why even manufacturers often include a disclaimer: any second line, no matter how faint, could indicate a positive. If you see a shadow of a line and aren’t sure, the safest move is to treat it as a possible positive and confirm through one of two paths: another at-home test in a few days, or a lab-based NAAT/PCR test if accessible.
What Can Make a Test Invalid or Unclear?
Chlamydia rapid tests aren't foolproof, and they aren’t idiot-proof either, which isn’t an insult, it’s reality. People test while panicked, distracted, drunk, tired, or just overwhelmed. And even if you’re calm and focused, the test itself can betray you if the conditions aren’t right. Here’s what tends to go wrong:
Tests can be rendered invalid by expired reagents, improper storage, or even high humidity in the room. Using a swab that touches another surface, applying too little buffer liquid, or letting the test sit too long before or after use can all compromise accuracy. And sometimes, the test itself is defective, manufacturing flaws happen, especially with mass-produced kits sold online without regulation.
The result? A test with no control line, a broken cassette, or a weird smear instead of a line. If there’s no control line at all, the test result can’t be trusted. That means you need to toss it and start over.
Still unsure? Here’s a quick guide to what can go wrong and how to fix it.
| Problem | Possible Cause | What to Do |
|---|---|---|
| No control line appears | Test kit was defective, expired, or used incorrectly | Test is invalid; discard and retest with a new kit |
| Smudged or incomplete line | Too much buffer solution, improper placement, or condensation | Consider retesting; avoid steamy bathrooms and handle gently |
| Two lines, but test line is blurry or fading | Read too late, over 20–30 minutes | Result may be inaccurate; retest at proper timing |
| Single test line, no control line | Rare test malfunction or user error | Test invalid; always confirm control line is present |
Table 3: Troubleshooting chlamydia rapid test issues. Valid results require a clear control line. Anything else means you need to retest.
What to Do After a Faint Positive Line
So you’ve got a faint line. You’ve double-checked the timing. The control line is there. The test is technically “valid.” Now what? First, take a breath. A faint line isn’t the end of the world, it’s a nudge to take the next step. Chlamydia is one of the most common and treatable STDs. Left untreated, yes, it can cause complications like pelvic inflammatory disease, infertility, or chronic pain. But when caught early, it’s typically cleared with a short course of antibiotics.
The best thing you can do now is confirm. That means either taking a second test in 3–5 days (especially if your exposure was recent and you tested early) or getting a lab-based NAAT test if you want clinical certainty. Many people start with a rapid test because of anxiety or privacy, then follow up with a lab test if results are positive or unclear.
Jorge, 35, took a rapid test after a partner told him they’d tested positive. His result showed a faint line.
“I was freaking out, but I didn’t want to go to a clinic right away. I took another test three days later, and the line was darker. That’s when I called a telehealth service and started treatment.”
This layered approach, rapid first, confirmatory second, is common, especially when you’re navigating fear, stigma, or scheduling barriers. And remember: no one ever regretted confirming a positive. What people do regret is ignoring early warnings because the line looked “too faint to be real.”
Check Your STD Status in Minutes
Test at Home with Remedium3-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $69.00 $147.00
For all 3 tests
Disposing of the Test and Protecting Your Privacy
Once you’re done testing, you’re not totally done. That used cassette is still sitting there, staring at you. If you live with roommates, family, or a partner you haven’t told yet, even tossing it can feel loaded with risk. The good news is that test cassettes don’t contain biohazardous material once they’re dry, and you can usually wrap them in tissue or a plastic bag and throw them out with household trash.
Don’t flush anything down the toilet, not the swab, not the wrapper, and definitely not the cassette. If your kit includes a disposal bag, use it. If not, wrap it up tight and toss it where others won’t go snooping. Some people keep the used test in a drawer for a few days, just in case they want to show it to a provider or compare with a future retest, but that’s your call. The cassette won’t stay stable forever, and most manufacturers advise against interpreting results after the 30-minute mark.
As for digital privacy: don’t upload your test photo to Reddit or a group chat unless you’re absolutely sure about consent and anonymity. If you want a second opinion, some telehealth services allow photo uploads for professional interpretation. Choose that over social media speculation every time.
Your Next Step, And Why It’s Worth Taking
Getting a faint line isn’t failure, it’s a starting point. It’s your body saying, “Hey, something might be up.” You’re not dirty. You’re not reckless. You’re someone taking charge of their health, and that deserves credit, not shame. Whether you choose to retest at home or schedule a lab test, you’re doing exactly what smart, informed, sexually active people do: checking in.
If you're stuck in the spiral of Googling, know this, peace of mind is closer than you think. A clear result is just one solid test away. And if it’s positive? That’s not a sentence. That’s a solvable situation.
Need help deciding which test to take next or where to order another kit? STD Rapid Test Kits offers discreet, fast-delivery options including the Chlamydia Rapid Test Kit and combination kits that check for multiple infections at once. Your results, your privacy, your move.

People are also reading: What Happens If You Ignore Trichomoniasis?
Retesting: When, Why, and How to Do It Right
If your test result left you confused, or confirmed a faint positive, you’re probably wondering when it’s safe (or smart) to retest. Here’s the deal: timing matters just as much the second time around. Retesting too early can give you another faint, unclear, or even false-negative result. Retesting too late delays treatment and risks further spread.
Chlamydia typically becomes detectable by rapid antigen tests around 7 to 14 days after exposure. NAAT (nucleic acid amplification) tests, like the ones used in labs and mail-in services, can sometimes detect infection as early as 5 days, but accuracy still improves the longer you wait. If your first test was taken within a week of potential exposure and showed a faint line, the best plan is to wait 3 to 5 more days before retesting at home. If you can access a NAAT test at a clinic or via mail-in, go for it, that method offers higher sensitivity, especially for low-level infections.
Don’t make the mistake of assuming a clearer line means a “worse” infection or that a disappearing faint line means you’re cured. Rapid tests are not viral load monitors. They don’t measure severity, they detect presence. Think of them like a smoke detector: even a faint beep is telling you something’s burning.
Still unsure whether you’re ready to retest? Ask yourself: Have symptoms changed or intensified? Has it been at least 7 days since potential exposure or since your last test? Have you had sex again since your last test, especially unprotected? If the answer to any of these is yes, a second test is a good idea.
When You Should Consider a Clinic or Lab-Based Test
Rapid tests give fast answers, but sometimes, fast isn’t enough. If your result is confusing, your symptoms are getting worse, or you simply want the most accurate read possible, it’s worth going the clinical route. Lab-based NAAT tests for chlamydia are considered the gold standard for a reason: they can detect even trace levels of bacterial DNA and are far less prone to visual interpretation errors than cassette tests.
Some situations almost always warrant a lab follow-up:
- Your test shows a faint line and you're experiencing symptoms like unusual discharge, pelvic pain, testicular ache, or burning urination.
- You've had multiple recent partners and aren't sure who you might have contracted it from.
- You're pregnant or immunocompromised and need fast, reliable treatment planning.
- You're about to start treatment and want a confirmed diagnosis first (some clinics require it).
In-person clinics offer confidentiality protections, and many have express services for STI testing. If privacy or stigma is a barrier, look into telehealth platforms that offer mail-in testing with lab-grade analysis and optional doctor consults. You can usually collect your sample at home and send it off the same day, getting results in 1–3 business days.
Lab-based confirmation doesn’t mean your first test “wasn’t real.” It just means you’re being smart and covering your bases. You’d double-check a weird bank transaction. Why not double-check your health?
What to Say (and Not Say) to a Partner After a Faint Positive
This is the part no test instruction sheet prepares you for. The moment you realize that this isn’t just about you anymore. If you’ve tested positive, or even had a faint result that you’re treating seriously, it’s time to think about disclosure.
Lena, 29, had been seeing someone casually for a few months. When her faint line showed up, she froze.
“We weren’t exclusive, but I still felt like I owed him honesty. I didn’t want him to hear it from someone else or get sick.”
She sent a short text with a screenshot of the test and a message:
“I got a faint positive on a chlamydia test. I’m retesting tomorrow, but wanted to give you a heads-up in case you want to test too.”
His reply? “Thanks for telling me. I’ll get checked this week.” That was it.
You don’t need to offer a confession. Just a heads-up. Chlamydia doesn’t make you dirty, and it doesn’t require a full sexual history breakdown. You can say:
- “I just got a faint positive on a test and I’m getting it confirmed.”
- “There’s a chance I might have chlamydia, and I thought you should know.”
- “You might want to get tested too, better to catch it early.”
If you’re not ready to reach out directly, there are also anonymous partner notification tools supported by public health departments. You can send a message through those systems without revealing your name, but still give your partner the information they need to act.
Check Your STD Status in Minutes
Test at Home with Remedium10-in-1 STD Test Kit

 For Women
For Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $189.00 $490.00
For all 10 tests
The Emotional Fallout: You're Not Overreacting
It’s just a line on a plastic stick, but it can feel like a verdict. For many people, a faint positive taps into deep-seated fears: Am I gross? Will anyone want to be with me again? Am I going to get sick, lose my fertility, be judged forever?
Breathe. You’re not overreacting. You’re not alone. And you’re not broken.
Millions of people test positive for chlamydia each year. Many never have symptoms. Most clear the infection easily with treatment. What you’re experiencing, the spiral of shame, panic, second-guessing, is not weakness. It’s what happens when we grow up in a world that treats STDs as proof of failure instead of the medical events they are.
If you need support beyond the test, that’s okay. Some people talk to a therapist. Some confide in a trusted friend. Others write it all down and process solo. Whatever you do, don’t let that faint line become a wedge between you and your own body. You took the test. You sought truth. That makes you brave, not dirty.
You deserve answers, not assumptions. And if that means testing again, seeing a provider, or just having one less thing to worry about, that’s reason enough.
You’re the One in Control Now
Maybe you’re still staring at the test in the trash. Maybe you’ve already ordered a second kit. Maybe you're texting a partner, waiting for a reply, heart thudding. Wherever you are in this moment, remember: the test doesn’t define you. The result doesn’t diminish you. What matters is that you chose knowledge over fear, action over silence.
If you’re ready to take the next step, retest, confirm, or check for other STDs, there are tools made exactly for this. You can order a discreet chlamydia test kit right now, or choose a combo kit that screens for multiple infections in one go. Everything ships privately. No one has to know but you.
Your body is not a mystery. Your health is not a guessing game. And even a faint line is better than staying in the dark.

FAQs
1. Can a faint line on a chlamydia rapid test mean a false positive?
Yes, it can, but it all depends on when and how the test was used. If you tested at the right time and followed the directions carefully, a faint line could be a true positive. But signals can be wrong if they are exposed to moisture, expired kits, or read outside of the suggested time frame. If you're not sure, do another test or get confirmation from a lab-based NAAT test.
2. Is a faint positive on a chlamydia test still contagious?
Absolutely. Even if the result seems faint, it likely means chlamydia is present in your body. That means you can still pass it to a partner. Avoid sexual contact until you’ve confirmed the result and completed treatment. A faint line isn’t a maybe when it comes to transmission risk, it’s a reason to act.
3. When do I receive a faint positive after exposure?
Faint positives may appear as early as 5 to 7 days after exposure, and even sooner in speedy antigen tests. After 10 to 14 days, it is more reliable, though. You may test too early and see the infection when it is in its beginning phase, and that may make the line appear faint. You should re-test in a few days, though.
4. Is a thin line evidence that I am mildly infected?
Nope. Line intensity has nothing to do with severity. It just indicates the level of detectable antigen present. There are persons with weak positives who keep getting harsh symptoms, and persons with dark-stained lines who feel great. Always interpret the faint line as the indicator, never the severity level.
5. Is it possible to ignore a thin line if I am asymptomatic?
No, your symptoms do not closely indicate if you have chlamydia. About 70% of chlamydia infections do not present stark symptoms. Untreated chlamydia may result in long-term health problems such as infertility or pelvic inflammatory disease even when you do not have symptoms. Even if you "feel fine," do not ignore a borderline result.
6. What if I received a weak line but negative partner?
Your result may differ because of timing, test, or sampling differences. If your positive line is real, assume that you're positive and follow up for confirmation. Ask your partner to retest after the due window period. Different bodies, different timing.
7. May I re-test with the same kit if I am in doubt?
No. You may not use another kit once you have used it, even if you think the sample was too small. You do have to use a brand-new kit for each test. Using the same parts more than once maximizes false readings and contamination.
8. How do you properly store a rapid test in order to avoid errors?
Keep your kit at room temperature (59°–86°F or 15°–30°C), in dark, dry place, away from moisture and heat. Never keep it in a hot car or steamy bathroom. Always read and examine the expiration date prior to use.
9. Must I test for all other STDs if I have a wispy line for chlamydia?
Yes. Co-infections do occur. When you test positive for chlamydia in the background, it is possible your body is just trying to let you know that you have a bigger problem. When you've slept with more than one person or had unsafe sex, you might wish to think about getting a combo STD kit that will test for gonorrhea, trichomoniasis, syphilis, and other STDs.
10. Must I believe in at-home tests completely?
When properly used, reliable home chlamydia test kits prove highly reliable. Otherwise, it is best if you follow timing guidelines, use recently purchased kits, and do not misread test results. For greatest assurance, use rapid test and in addition, clinical verification.
You Deserve Clarity, Not Confusion
You’ve made it through the fear, the waiting, and the blur of test lines. Whether you’re holding a faint result in your hand or just preparing for what could happen, remember this: you’re taking care of yourself. That’s the opposite of shame, it’s power.
Don’t let one blurry pink line leave you in limbo. Retest, confirm, and move forward with clarity. If you need the next test, we’ve got you. STD Rapid Test Kits offers reliable, discreet shipping and tests you can trust, whether you’re checking a suspicion or retesting after a faint line.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted six of the most relevant and reader-friendly sources.
Sources
1. Planned Parenthood – Chlamydia Overview
2. Atlas Medical: Chlamydia Rapid Test Device Instructions (even faint lines count as positive)
3. Understanding False Positives & False Negatives in STI Tests | Verywell Health
4. Testing for STIs at Home | ASHA Sexual Health
5. Screening for STIs at Home or in the Clinic? | PMC
About the Author
Dr. F. David, MD is a board-certified infectious disease specialist focused on STI prevention, diagnosis, and treatment. He blends clinical precision with a no-nonsense, sex-positive approach and is committed to expanding access for readers in both urban and off-grid settings.
Reviewed by: Dr. M. Cheng, MPH | Last medically reviewed: October 2025
This article is for informational purposes and does not replace medical advice.