Quick Answer: STDs are rising in Connecticut’s wealthiest towns due to factors like increased travel, stigma around testing, and symptom-free infections. Discreet at-home kits offer accurate, private testing without disrupting busy schedules.
When the Symptoms Don’t Match the Stereotypes
One of the most persistent myths about sexually transmitted infections is that they only happen to “other people.” In reality, Connecticut DPH data show rising rates of syphilis, gonorrhea, and chlamydia in towns with median household incomes far above the national average. Symptoms in these cases often don’t match the textbook images found in outdated pamphlets. Sometimes it’s a single sore mistaken for razor burn, a mild sore throat after a weekend trip, or nothing at all until a routine screening, or a partner’s diagnosis, forces the issue.
Affluent professionals are uniquely prone to missing early warning signs. Tight schedules make it easy to dismiss mild discomfort as stress or travel fatigue. Dermatologists in Fairfield County have reported patients asking about “mystery rashes” they assumed were allergic reactions, only to test positive for syphilis. And because many STDs can be asymptomatic, waiting for obvious signs is a gamble with high stakes.

People are also looking for: The Breakthrough HIV Injection You Need to Know About
“I Thought It Was From the Hotel Soap”
Jenna, 41, splits her time between Hartford and New York for her consulting job. “I travel so much that my skin is always irritated from hotel products,” she said. “When I noticed a patchy rash on my torso, I chalked it up to bad lotion. It wasn’t until my partner had symptoms that I even thought to test.” Jenna used an at-home combo test kit she could mail back overnight. Her results confirmed syphilis, and her doctor told her catching it then likely prevented more serious complications.
“If it had been years ago, I probably would’ve ignored it until it was too late. The privacy of testing at home made all the difference.”
The Numbers Tell a Different Story
According to the CDC’s 2023 surveillance report, national STD rates have been climbing for nearly a decade, but the trend in Connecticut’s wealthier zip codes has been especially sharp. Between 2018 and 2023, cases of syphilis in the state nearly doubled, with Fairfield County seeing some of the largest increases. A recent study on neighborhood economic status and STI rates found that higher-income areas aren’t immune; in fact, certain behaviors, like more frequent travel, overlapping relationships, and lower perception of risk, can drive rates higher.
Another driver is the gap between exposure and testing. In Connecticut’s business districts, long work hours and the pressure to maintain a flawless image create real barriers to care. As one Stamford-based physician put it, “I’ve had patients delay testing because they didn’t want to be seen at a clinic near their office. That delay can mean weeks of unknowingly spreading an infection.”
Busting the Myths That Keep Professionals from Testing
The biggest misconception I hear is, “I’m in a committed relationship, so I don’t need to test.” While monogamy can reduce risk, it doesn’t erase it. Infections can linger for months, or years, without symptoms, and sometimes one partner’s past exposure shows up much later. Another myth? That STDs are “a young person’s problem.” Connecticut DPH data show cases among adults in their 40s, 50s, and beyond are rising steadily, especially for syphilis and herpes. Age and income don’t grant immunity from biology.
Some even believe that visible symptoms are a given. The reality is that chlamydia is often called the “silent” infection because so many never notice a change. The latest primary care screening trends show that when asymptomatic individuals are tested proactively, detection rates spike, not because more people are suddenly infected, but because hidden cases are finally uncovered.
Check Your STD Status in Minutes
Test at Home with Remedium7-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $129.00 $343.00
For all 7 tests
When Privacy Becomes a Barrier
For high-income adults in Connecticut, the desire for privacy can paradoxically make it harder to stay healthy. In smaller, affluent communities, running into a client or neighbor at a local clinic feels risky, even if that’s purely imagined. This social pressure pushes some to delay testing until symptoms are unavoidable, which is when treatment can be more complicated and outcomes more serious.
One Greenwich banker told me, “I knew something was off, but the idea of being spotted at a clinic downtown was worse than the discomfort. I waited six weeks before ordering a test online. Turns out I had gonorrhea, and my partner did too.” That delay could have been avoided with a mail-in kit from the start.
Between Flights at JFK
Picture a 36-year-old executive between flights at JFK, headphones in, toggling between emails and an online STD kit order form. His mind flicks between the client meeting he just wrapped in Los Angeles and the brief, unplanned encounter he had on the trip. He chooses a discreet home testing kit, shipped to his Connecticut apartment, because it offers him the control of testing on his own terms, no waiting room, no questions, no chance of being recognized.
Why the Rise Is Happening Now
Experts point to a convergence of factors: more travel and mobility, increased use of dating apps across all age groups, and an underestimation of risk in established social circles. The BMJ Sexual Health study on online sexual health services notes that people with higher digital literacy are more likely to adopt at-home testing, but also more likely to take sexual risks, believing they can “always test later.”
Connecticut’s proximity to major metropolitan hubs like New York City means residents often have larger, more varied social networks. Add in the time pressure of demanding careers, and you get a perfect storm where exposure is more likely and follow-up testing is delayed. Data from the CDC state rankings reveal that while overall rates in Connecticut are lower than some states, certain counties have doubled their reported cases in under five years.

People are also reading: The Most Common Sexually Transmitted Diseases and How They Spread
This Isn’t Just Razor Burn, And Here’s Why
In clinic photos, herpes looks dramatic and unmistakable, which makes real life confusing. Many first outbreaks are subtle or look like a shaving nick that stings a little in the shower and then fades. A tender bump that shows up after a long run could be friction, but if it returns in the same spot or is paired with tingling, testing is the safest move. The same goes for a painless sore from syphilis; it can hide where you barely see it, or feel like chapped skin. When something feels “off,” assume your body is asking for clarity, not panic.
A scratchy throat after a weekend away is easy to blame on airplane air, yet oral gonorrhea and chlamydia can present as mild sore throats or nothing at all. Connecticut professionals have told me they ignored throat irritation for weeks because meetings, kids’ sports, and travel made the timing inconvenient. The truth is that a three-minute swab at home beats weeks of guessing. When symptoms are quiet or masquerading as normal life, timing your test matters more than trying to self-diagnose by sight alone.
The Sunday Shower Test
It’s 7:30 a.m. in Stamford. Steam fogs the mirror, and a faint cluster of bumps near the bikini line is playing tricks on the mind. Is it the new spin class leggings or something else? The calendar says back-to-back strategy sessions at 9 and 11. She props her phone on the sink, opens the results portal from last month’s negative screen, and orders a new kit before the coffee finishes brewing. By Wednesday, she’ll swab at home, drop the envelope at the building’s concierge, and keep her life moving. That’s not avoidance; that’s owning the timeline.
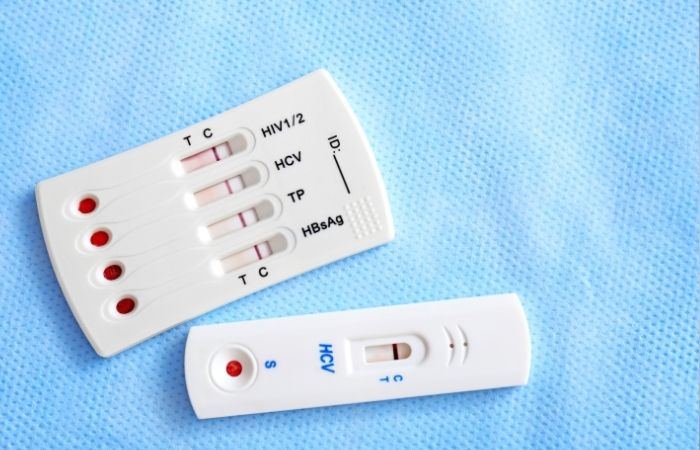
Accuracy, Windows, and What At‑Home Tests Really Catch
At-home tests aren’t a compromise; they’re a different doorway into the same lab-backed answers. Self-collected swabs and urine specimens are validated for chlamydia and gonorrhea, including throat and rectal sites when indicated. Large program evaluations have shown strong concordance with clinic-collected samples when instructions are followed carefully, which means your results are meant to be trusted, not second-guessed. Where people go wrong is the window period. If you test too early after an exposure, you can get a false sense of security; if you wait for perfect timing, you might inadvertently expose a partner. The middle ground is testing now and, if the exposure was very recent, planning a follow-up according to the infection’s window.
For chlamydia and gonorrhea, many programs recommend testing around one to two weeks after a possible exposure, with earlier testing considered if symptoms appear. For syphilis, blood tests may not turn positive immediately, so a repeat test in several weeks is common if suspicion is high. For HIV, at-home options vary; some detect antibodies that take weeks to develop, while lab-based fourth-generation tests detect both antigen and antibodies earlier. None of this is about being perfect. It’s about pairing your reality, travel, deadlines, kids’ drop-off, with a plan that closes the gap between exposure and answers.
Check Your STD Status in Minutes
Test at Home with Remedium7-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $129.00 $343.00
For all 7 tests
Myth to Retire: “If My Partner Looks Healthy, We’re Fine.”
Most STIs don’t announce themselves. Partners can carry chlamydia or gonorrhea with zero symptoms and still transmit. Someone can have herpes for years without classic blisters and still shed virus intermittently. And because syphilis lesions can be small and painless, they’re easy to miss, especially during oral sex. The point isn’t to become a detective every time you touch someone. It’s to treat testing like teeth cleaning, routine, not accusatory. Think of it as emotional hygiene that protects trust rather than threatens it.
When people skip testing, it isn’t ignorance; it’s often hope. Hope that a tickle in the throat is allergies. Hope that a bump is an ingrown hair. Hope that last night never happened. Hope is human, but it’s not a medical plan. A plan is deciding, right now, how you’ll get tested in ways that fit your life. A plan is choosing privacy without choosing silence. A plan is scheduling follow-up if you tested very early or if a partner develops symptoms later.
Sex‑Positive, Zero‑Shame Scripts That Actually Work
Good conversations don’t need perfect words. They need posture: curious, calm, and collaborative. Try telling a partner, “I’m keeping testing regular because I care about us, not because I don’t trust you.” Or, “Travel and timing make clinic visits hard for me, so I’m using an at‑home kit to stay on top of things.” Notice how those sentences move away from blame and toward shared safety. If you’re newly dating, you can say, “I like you, and my norm is testing before we stop using barriers. What’s your norm?” Healthy adults respect boundaries; unhealthy dynamics pressure you to drop them.
One client from Darien told me, “I felt dramatic bringing up testing before a weekend away. Then he said, ‘I do the same thing before big trips, it keeps life simple.’ We both ordered at-home kits, screen-shared when the results came in, and had a lot more fun after that.” Clean talk is sexy talk when you’re both on the same team. It gives intimacy a wider runway instead of a panic brake.
People are also reading: The Risks of Untreated Chlamydia in Men: Epididymitis and Beyond
Treatment Is Not a Moral Verdict
Antibiotics for chlamydia and gonorrhea work well when taken as prescribed, and follow‑up testing ensures the infection is gone. Syphilis requires specific antibiotics and time-sensitive follow-up, and your clinician will guide you through staging and contact notification. If you test positive for herpes, antiviral medication can reduce outbreaks and lower the chance of passing it on, and many people find that simply naming it out loud dissolves the fear that gave it power. None of this defines your character, your relationship, or your future. It defines a moment of care you’re choosing to take.
One West Hartford couple told me they treated a dual positive like a team project. “We blocked off a Saturday, made a list, and handled testing, pharmacy, and partner conversations in one go,” said Marcus.
“By dinner, the worst part was over, and the relief was real.”
Their story isn’t unusual; it’s what happens when people swap secrecy for structure and let treatment be the bridge back to normal life.
FAQs
1. Is it possible to get chlamydia from kissing?
No. You can't get chlamydia from kissing someone you don't know. It mostly spreads through genital contact during vaginal, anal, or oral sex.
2. Are STD tests you do at home as accurate as those done in a clinic?
Yes, but only if they are collected and handled correctly. Most of them use the same certified labs as clinics and meet the same standards for clinical accuracy.
3. How long should I wait to take a test after having sex without protection?
It depends on the type of infection. You can find chlamydia and gonorrhea in about one to two weeks, but you may need to wait a few weeks for syphilis and HIV to show up.
4. Is it possible to have an STD without showing any signs?
Of course. Chlamydia and herpes are two infections that can be passed on even when they don't show any symptoms for months or years.
5. Will my insurance company find out if I order a kit to use at home?
There is no insurance billing if you pay out of pocket. Your privacy is protected by private payment and discreet shipping.
6. How do I tell my partner that I tested positive?
Be direct and clear. Tell them what the diagnosis is, what the treatment plan is, and that you care about their health too.
7. Do STDs go away on their own?
No. Antibiotics can help some infections, but viral infections like herpes stay in the body and need to be managed all the time.
8. What if my partner doesn't want to get tested?
First, take care of your own health. If safety boundaries aren't followed, use barriers all the time and think about the relationship again.
9. Can you find STDs on the same day?
Some infections can be tested quickly, but most at-home kits need to be sent to a lab for processing, which can take 1 to 5 days.
10. Is it safe to take an at-home test while on the road?
Yes, as long as you can safely get the kit and send the sample back quickly. Think about the lab's schedule to get results faster.
You Deserve Answers, Not Assumptions
Whether you live in downtown Stamford or a quiet corner of Litchfield County, your time and privacy matter, but so does your health. Rising rates in Connecticut’s wealthiest areas aren’t a sign of carelessness, they’re proof that anyone can be affected. The smartest move is to treat testing as part of your normal health rhythm, without waiting for symptoms or stigma to push you there.
Sources
1. Connecticut DPH: STD Statistics in Connecticut
2. CDC Sexually Transmitted Infections Surveillance, 2023
3. Neighborhood Economics, Insurance & STI Risk
4. Primary Care Screening for STIs: Trends in Testing










