Quick Answer: Yes, you can get chlamydia from oral sex, especially when giving oral to someone with a genital infection. It can infect the throat, often with no symptoms, or show up as a sore throat, mild fever, or swollen glands. Testing is the only way to know.
Why This Matters for College Students (and Anyone Hooking Up)
Let’s be real, college hookups don’t always include condoms, and oral sex often feels like the “safe” option. That’s one reason why infections like oral chlamydia are spreading quietly across campuses. Many students think they’re avoiding risk by skipping penetration, but STDs don’t need penetration to spread.
One CDC report noted that young adults aged 15–24 account for nearly two-thirds of reported chlamydia cases. And since oral sex is often left out of safer sex education, infections in the throat are frequently missed or misdiagnosed as strep, tonsillitis, or even allergies. The result? Ongoing transmission, untreated infections, and confusion when symptoms do show up.
If you're in college or casually dating, this article is for you. We’re going to unpack what oral chlamydia actually looks and feels like, how it’s different from a sore throat, and why testing matters even if you're symptom-free.
People are also reading: Chlamydia in College: How to Test, Treat, and Move On
Can You Really Get Chlamydia from Just Oral Sex?
Yes. You don’t need vaginal or anal sex to get chlamydia. Oral sex can absolutely transmit it, especially when giving oral to someone with a genital infection. In fact, chlamydia bacteria can infect the throat (pharyngeal chlamydia) when the mouth comes into contact with infected genital fluids or secretions.
Here’s how it happens: If someone with a genital chlamydia infection receives oral sex, the person giving can contract the bacteria in their throat. Similarly, if someone has oral chlamydia (yes, it can live in the throat), they can pass it on during oral sex, though this route is less common. Most transmission occurs from mouth-to-genital contact, not the other way around, but both are possible.
According to a 2020 study in the journal Sexually Transmitted Diseases, throat chlamydia infections are often asymptomatic and can go undetected without routine screening, particularly in young adults and men who have sex with men. That means someone could carry and spread the infection without ever knowing they had it.
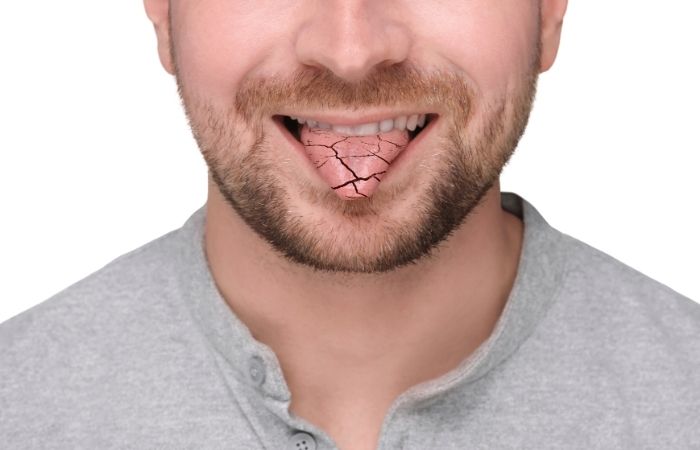
What Oral Chlamydia Feels Like (If You Have Symptoms at All)
Here’s the kicker: most people with oral chlamydia feel nothing. That’s why it’s called a “silent” infection. But when symptoms do show up, they often mimic more common illnesses like strep throat or mild respiratory infections, making them easy to brush off or misdiagnose.
Possible symptoms of oral chlamydia include:
| Possible Symptom | What It Can Feel Like |
|---|---|
| Sore throat | Persistent irritation or scratchiness, often with no other cold symptoms |
| Swollen lymph nodes | Swelling in the neck or under jaw, tender to touch |
| Red or inflamed tonsils | May appear similar to strep or tonsillitis |
| Low-grade fever | Mild elevation in temperature, especially in the evenings |
| Bad breath or taste changes | Metallic taste or unusual mouth odor without dental cause |
Figure 1. Common signs of oral chlamydia, though most people never feel symptoms at all.
Even if you feel totally fine, that doesn’t mean you’re in the clear. You can still carry and transmit the infection to partners. That’s why getting tested is crucial, especially if you’ve had unprotected oral sex and either you or your partner has other partners.
How Oral Chlamydia Spreads
Chlamydia doesn't care what you think sex is. It spreads through contact with infected genital fluids, so oral sex can also spread it. This means that you could still get infected even if there was no vaginal or anal penetration, especially if there was no barrier protection used.
Here are a few real-life hookup scenarios that illustrate how oral chlamydia transmission happens:
| Scenario | Why It's Risky |
|---|---|
| You gave oral sex to someone with a genital chlamydia infection | The bacteria can infect the tissues of your throat, this is the most common form of oral transmission |
| You received oral sex from someone with chlamydia in their throat | Less common, but possible, especially if they also kissed or touched their own genitals before oral |
| There was brief contact without ejaculation | Chlamydia can spread through pre-ejaculate and mucous membranes, orgasm isn’t required for infection |
| You used your mouth on a toy or finger that had infected fluids | If shared without cleaning, chlamydia can survive short-term on surfaces and still infect you |
Figure 2. Common ways oral chlamydia is transmitted, even in “non-penetrative” hookups.
And here’s a hard truth: dental dams and condoms are rarely used during oral sex. One survey of college students found that less than 10% reported using any protection during oral acts. That creates a perfect setup for invisible transmission, especially with partners you don’t know well.
Check Your STD Status in Minutes
Test at Home with RemediumChlamydia Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $33.99 $49.00
How to Get Tested for Oral Chlamydia
Oral chlamydia requires a specific kind of test: a swab of the throat. Standard STD tests, including most at-home kits, usually target genital or urine samples, so unless you specifically ask or order a test that includes a throat swab, this infection might go undetected.
There are three ways to test for oral chlamydia:
At-home test kits (with throat swab option)
Some newer kits now include pharyngeal testing options, allowing you to swab your throat and mail the sample to a lab. Always double-check that the product supports oral site testing.
Clinic-based NAAT testing
Many sexual health clinics offer nucleic acid amplification tests (NAATs), which are highly accurate for detecting chlamydia in the throat. You’ll usually need to ask for a throat swab specifically.
Combination STD test panels
Some comprehensive test panels, including those offered online, let you choose multiple collection sites (oral, genital, rectal). These are especially helpful for people with multiple partners or types of sexual contact.
If you’re worried you might have oral chlamydia, or you just want peace of mind after a hookup, testing is the only way to know. Results can take anywhere from 20 minutes (for some rapid kits) to 3 days (for lab-based mail-ins).
Whether you’re trying to stay ahead of symptoms or clear up something that just feels off, this discreet chlamydia test kit is an option many students trust for quick answers.
“We Didn’t Even Have Sex. I Still Got It.”
Devon, 20, met his partner through a dating app. They hung out a few times before anything happened. On a late night after drinks, they made out and hooked up, but never had intercourse. Just oral. A week later, Devon started feeling run-down. His throat was scratchy, and his neck felt tender. He chalked it up to a cold.
“It didn’t feel serious enough to go to a doctor. I thought maybe I yelled too much at the party. But then I saw this post on Reddit about someone getting an STD from oral, and it freaked me out.”
Devon ordered an at-home test that included an oral swab. The result? Positive for chlamydia, in his throat. The conversation that followed with his partner wasn’t easy, but it led both of them to get treated and test for other STDs, too.
This is exactly why testing matters even when the hookup seems “low risk.” Oral sex is often underestimated, but it’s a real route of transmission for several STDs, including chlamydia, gonorrhea, and even syphilis.

People are also reading: Her Pap Came Back Abnormal. What You Need to Know as a Man
What Happens If You Don’t Treat Oral Chlamydia?
Here’s the uncomfortable truth: even if oral chlamydia doesn’t cause symptoms, it can still do damage. When left untreated, the infection can linger in the throat, continue to spread to partners, and potentially trigger inflammatory responses in the body. And while rare, oral chlamydia has been associated with secondary infections, especially in people with compromised immune systems.
Unlike genital chlamydia, which is widely recognized as a cause of pelvic inflammatory disease (PID) and infertility, oral chlamydia is more likely to go undiagnosed. That makes it a hidden carrier, and a key contributor to reinfection cycles in couples who don’t get tested together.
Studies have shown that untreated pharyngeal chlamydia can persist for weeks or even months. During this time, every sexual encounter becomes a chance to unknowingly pass it on, even if you feel perfectly fine.
And here’s the kicker: standard treatment for chlamydia (a single dose of azithromycin or a 7-day course of doxycycline) works just as effectively for oral infections. But only if you know it’s there. That’s why screening is critical, especially after a new partner or risky encounter.
Can Oral Chlamydia Spread to Genitals or Back to Your Partner
Yes. Oral chlamydia can be a source of reinfection in both directions. If one partner is treated and the other isn’t (especially when one only had oral exposure), the bacteria can ping-pong back and forth. This is one of the most common causes of repeat positive tests in couples who think they’ve “cleared” the infection.
For example: if you have chlamydia in your throat and perform oral sex on your partner after they’ve been treated, they can get reinfected. Similarly, if your partner had untreated genital chlamydia and you perform oral on them, even once, you can contract it in your throat. It’s a cycle that requires both people to be tested and treated at the same time.
To stop this loop, public health agencies recommend partner notification and dual treatment, even if only one person has symptoms. And remember, not every clinic routinely tests the throat unless you ask for it. If your provider doesn’t offer that, you can order a home kit that includes oral testing.
The CDC recommends retesting for chlamydia about 3 months after treatment to make sure the infection is gone and hasn't returned due to reinfection.
Should You Retest After Treatment (or After a Scare)?
Yes, especially if you’re sexually active with new or multiple partners, or if you weren’t fully sure whether your first test included a throat swab. Here’s how retesting works:
- After treatment: Wait at least 3 weeks before retesting to confirm the infection has cleared. Some residual bacterial DNA can trigger a false positive if you test too soon, especially with NAAT methods.
- After a negative result but ongoing risk: If you tested early (less than 7 days post-exposure), it’s smart to retest around day 14 for better accuracy. That’s when most tests will reliably detect an active infection in the throat.
- If symptoms persist: A sore throat that doesn’t improve, or that recurs after treatment, may signal incomplete clearance or a new exposure. Retesting helps you get clarity, and peace of mind.
If you’re not sure whether your last test covered oral exposure, or if you just want full-body reassurance, a combo test kit is your best bet. It checks for multiple STDs, quickly and discreetly.
Check Your STD Status in Minutes
Test at Home with Remedium3-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $69.00 $147.00
For all 3 tests
You Deserve Real Answers, Not Guesswork
Too many people brush off symptoms, skip testing, or assume oral sex is risk-free. But knowledge is power, and knowing whether you have an oral STD lets you protect yourself and your partners with confidence. You shouldn’t have to wait in line at a clinic or feel judged by a stranger just to get answers.
FAQs
1. Can you actually get chlamydia from oral sex?
Yes, and it’s way more common than people think. If your mouth touches someone’s genitals and they have chlamydia, the bacteria can infect your throat. Doesn’t matter if it was “just for a second” or if there was no ejaculation. Chlamydia doesn’t wait for a climax, it just needs skin and fluid contact.
2. What does oral chlamydia feel like?
Honestly? For most people, it feels like nothing. That’s what makes it sneaky. But when symptoms do show up, they can feel like a scratchy throat that won’t quit, swollen glands, maybe a low-grade fever. Imagine strep’s quieter, less dramatic cousin, but just as real.
3. Can I have it and not know?
Absolutely. Oral chlamydia is usually silent. You could carry it in your throat for weeks or months and have no clue, meanwhile, it’s still contagious. That’s why it spreads so easily, especially in hookup-heavy spaces like college campuses.
4. Will a regular STD test catch oral chlamydia?
Not unless it’s designed to. Most standard STD tests check urine or genital swabs. If you don’t specifically test your throat, either at a clinic or with a kit that supports oral swabs, it won’t show up. So if you’re worried about a hookup that involved oral, make sure you’re testing the right place.
5. Is kissing enough to give someone oral chlamydia?
It’s extremely unlikely. Chlamydia usually needs sexual fluids to spread, genital to mouth or mouth to genitals. Kissing someone who has it in their throat isn’t a big risk unless there’s open sores or fluid transfer. Still, good hygiene and avoiding deep kisses right after oral can’t hurt.
6. Do I need to get tested if I feel fine?
If you’ve had unprotected oral sex and you're wondering, yes, get tested. Not because you should panic, but because peace of mind is better than playing symptom roulette. The best time to test is around 7–14 days after exposure. If you’re testing sooner, you might need a follow-up to be sure.
7. What happens if I don’t treat it?
It can linger. Even if you’re symptom-free, you can still pass it to partners. In rare cases, untreated infections can mess with your immune system or contribute to reinfection cycles in couples. Translation? You’ll keep swapping it back and forth unless both of you test and treat.
8. Can oral sex give me chlamydia even with a condom?
Condoms help, definitely use them, but they’re not perfect. Most people don’t use them during oral sex, and even when they do, bacteria can still be present in areas that aren’t covered. So yes, you can still get chlamydia from oral, even with protection. Lower risk, not zero risk.
9. Can I get reinfected after treatment?
Yes, and it happens more than people realize. If your partner wasn’t treated at the same time, or if they had it in their throat and didn’t know, you can get it all over again. That’s why retesting after treatment (usually at the 3-month mark) is strongly recommended by the CDC.
10. Is oral chlamydia treated the same way?
Yep. The same antibiotics used for genital infections work on throat infections. Just make sure your provider knows where your exposure was, so you’re not only getting treated but getting tested in the right places too. And please, finish the whole prescription, even if you feel fine halfway through.
You Know Your Body, Now Get the Clarity You Deserve
Whether it’s a dry tickle in your throat or just a sinking gut feeling that something isn’t right, your instincts matter. And so does your peace of mind. Oral sex isn’t risk-free, but with the right tools and knowledge, you can stay ahead of the guesswork.
Don’t keep wondering. This at-home combo STD test kit lets you check for multiple infections, including chlamydia, quickly, discreetly, and without judgment.
How We Sourced This Article: We combined current guidance from leading medical organizations with peer-reviewed research and lived-experience reporting to make this guide practical, compassionate, and accurate. In total, around fifteen references informed the writing; below, we’ve highlighted six of the most relevant and reader-friendly sources.
Sources
1. WHO – Sexually Transmitted Infections
2. Planned Parenthood – What is Chlamydia?
4. STI Risk and Oral Sex – CDC
About the Author
Dr. F. David, MD is a board-certified infectious disease doctor who specializes in preventing, diagnosing, and treating STIs. He combines clinical accuracy with a straightforward, sex-positive approach and wants to make it easier for people in both cities and rural areas to read his work.
Reviewed by: A. Menon, MPH | Last medically reviewed: January 2026
This article is for informational purposes and does not replace medical advice.










