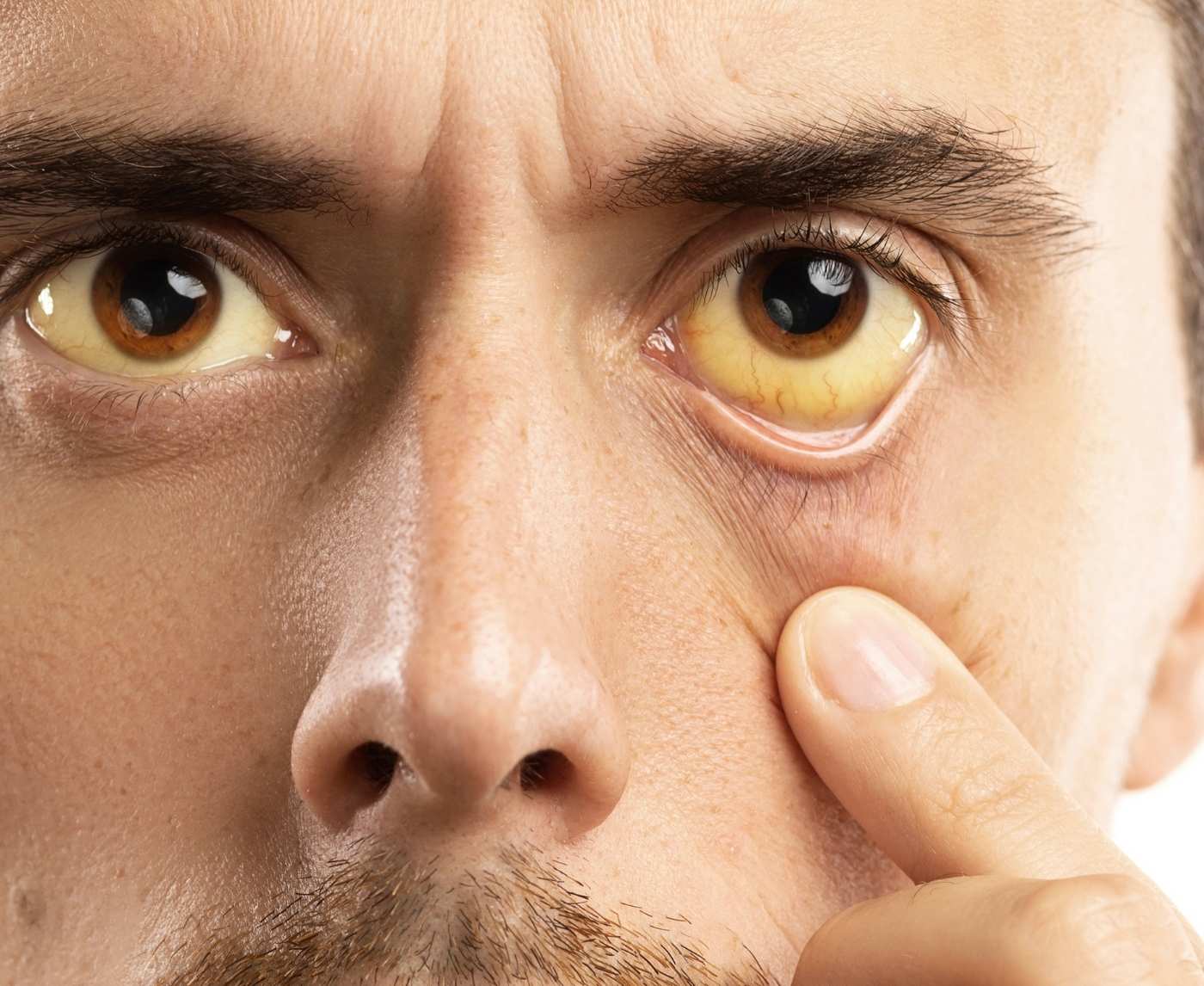
Quick Answer: Yes, you can get an STD in your eye. Infections like herpes simplex virus (HSV-1 or HSV-2), chlamydia, gonorrhea, and syphilis can infect the eye through direct or indirect contact with infected fluids. Symptoms may mimic pink eye but often involve more pain, sensitivity, or recurring issues.
This Wasn’t Just Pink Eye, It Was Herpes
Ty, 28, thought he’d been careful. He hadn’t had genital sex in months. But he’d recently hooked up with a friend, some kissing, some oral, nothing “high risk” in his mind. A week later, his eye started burning. “I thought maybe I rubbed my eye after touching something dirty,” he told me. “But then the vision in that eye got cloudy, and it just kept getting worse.”
The herpes simplex virus type 1 (HSV-1) that causes cold sores also causes ocular herpes, but it doesn't stay in the mouth. It can spread through skin-to-skin contact, saliva, or even a dirty finger. The virus can cause herpes keratitis when it gets into the eye. This can lead to ulcers on the cornea. This isn't just annoying; if you don't get it treated, it could make you blind for good.
Ty's story isn't unusual. A study published in the Journal of Ophthalmology in 2022 found that ocular HSV affects about 1.5 million people around the world each year. Many of these people first think they have seasonal allergies or bacterial conjunctivitis. Most cases can be avoided if people know what to look for and are aware of the problem.
The Symptoms That Send People Googling at 2AM
Here’s the part that makes this so confusing: ocular STDs look like a dozen other things. Pink, itchy eyes? Could be viral conjunctivitis. Crusty lashes? Maybe bacterial. Light sensitivity and blurry vision? Could even be dry eye or a scratched cornea. That’s why people delay care. That’s why they Google phrases like “burning eye after oral sex” or “STD that looks like pink eye.”
What differentiates an eye-related STD is usually how aggressive or persistent the symptoms are. Herpes eye infections, for instance, often recur. One day it’s fine, the next it’s on fire. Syphilis can attack the optic nerve and cause a dull, persistent ache behind the eye. Gonorrhea and chlamydia? Those are less common but more dangerous, gonorrhea in particular can rapidly eat through eye tissue if untreated.
The problem is that most urgent care clinics don’t think to test for STDs when a patient presents with eye irritation. In fact, unless you bring it up, or unless your provider knows to look for it, it might never get flagged. That’s what happened to Liana, 24, a queer artist who caught chlamydial conjunctivitis from a partner she only kissed and received oral from. “I got passed between three doctors before someone asked if I’d had recent oral sex,” she told me. “It took weeks to get the right antibiotics.”
This delay is common. According to a 2023 clinical review in Sexually Transmitted Diseases, ocular STDs are frequently missed due to low provider suspicion, especially in women, queer people, and people with nontraditional sexual exposure.

People are also reading: Are Schools Teaching Enough About STD Prevention
How Do STDs Even Get Into the Eye?
Let’s get this myth out of the way: you do not need to have penetrative sex to get an STD in your eye. You don’t even need genital contact. All it takes is a small viral or bacterial load transferred from one mucous membrane (like the mouth, penis, vulva, or anus) to another, and the eye’s surface counts.
This can happen through:
- Kissing someone with an active cold sore, then rubbing your eye - Receiving oral sex from someone shedding HSV or with undiagnosed chlamydia - Touching your partner’s fluids and then absentmindedly rubbing your eye - Using shared makeup or towels that haven’t been cleaned properly
The scary part is that it often takes only one exposure. Your eye doesn’t have the same defense systems your genital or oral tissues do. Once the pathogen enters, it can multiply quickly.
And for those wondering, yes, this applies to HSV-2 (the “genital” herpes virus), too. While it’s more commonly associated with genitals, HSV-2 can absolutely infect other mucous surfaces, including the eye. A case report in the British Journal of Ophthalmology found ocular HSV-2 in a patient who had no genital symptoms but had recently had oral-genital contact.
Check Your STD Status in Minutes
Test at Home with Remedium7-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $129.00 $343.00
For all 7 tests
When the Diagnosis Comes With Shame
For Marcy, 32, the hardest part wasn’t the blurry vision. It was the silence. “I didn’t tell anyone for months,” she said. “I kept thinking, who gets an STD in their eye? It felt dirty, like I’d done something wrong.” Marcy’s story echoes what public health experts already know: when infections show up in “unexpected” places, they carry even more shame. And that shame delays care.
We don’t talk enough about the emotional weight of STD stigma, especially when symptoms don’t fit the usual scripts. Most people assume herpes or chlamydia only live below the belt. When a red, weeping eye turns out to be sexually transmitted, people blame themselves. They fear being judged by their doctor, or worse, dismissed entirely.
In one 2020 study published in BMJ Open, researchers found that fear of stigma was one of the top three reasons people delayed STD testing, especially in cases involving non-genital symptoms. That delay can turn a minor, treatable eye infection into something far more serious.
And it gets worse for certain populations. Queer, trans, and nonbinary individuals often face additional layers of judgment, or worse, ignorance, from providers unfamiliar with their sexual health realities. "I had to argue with a clinic nurse to even consider that my eye infection might be linked to sex," said Devon, 26, who identifies as nonbinary. "She kept saying it was allergies."
This is why we write pieces like this. Because shame kills clarity. Because providers miss things when the symptoms don’t follow “normal” rules. And because too many people are suffering in silence, afraid that their infection says something bad about who they are. It doesn’t.
Can You Really Get an STD From a Kiss?
Yes. And it happens more often than people think. Herpes simplex virus, both HSV-1 and HSV-2, can live in the mouth, lips, and throat, even when there are no visible sores. When someone with oral herpes kisses you, gives you oral sex, or even shares saliva via a drink or cigarette, there’s a small chance of viral shedding.
Now combine that with one simple, unconscious motion: rubbing your eye. Touching your mouth and then touching your eye is enough. A recent CDC bulletin on HSV-1 transmission emphasized just how common asymptomatic shedding is, meaning people pass herpes even when they don’t have active outbreaks. That’s why the myth of “you’ll know if someone has herpes” is so dangerous.
But herpes isn’t the only culprit. Chlamydia trachomatis and Neisseria gonorrhoeae (that’s chlamydia and gonorrhea, for short) can also infect the eye via oral-genital contact or fluid transfer. These infections are rare, but when they occur, they can be aggressive. Gonorrhea in particular can erode the corneal surface in days if untreated, leading to vision loss. That’s not fearmongering, that’s a well-documented clinical fact.
This is why any new eye symptoms after oral, kissing, or intimate skin contact should raise a red flag. Not panic. Not shame. Just awareness. Especially if it’s accompanied by other signs like swollen lymph nodes, a gritty or foreign body sensation, blurred vision, or light sensitivity.
Doctors Miss This All the Time, Here’s What to Ask For
Even when someone shows up with textbook signs of an ocular STD, it’s easy to get brushed off. A nurse might call it allergies. A doctor might prescribe standard antibiotic drops. But unless someone orders the right tests, swabs for HSV, chlamydia, or gonorrhea, you’ll never know what’s really causing it.
This is where you need to advocate for yourself. If you’ve had recent intimate contact and your eye symptoms are persistent, painful, or weirdly severe, say so. You don’t need to disclose everything, just enough to shift the provider’s thinking.
You can say:
“I’ve had some recent close contact that might’ve involved saliva or fluids, and I’m worried this could be something infectious.”
Or:
“Can we rule out herpes or chlamydia? I read that they can affect the eye, and I’d rather be safe.”
That one question can change everything. It can lead to targeted testing, faster treatment, and fewer long-term complications. It can also help re-educate providers who haven’t updated their diagnostic radar since med school.
And if you’re too anxious to say it in person, consider an at-home STD test that screens for multiple common infections. While they won’t test your eye directly, they can help identify if there’s an underlying exposure that might be related.
Peace of mind is one test away.
Order your rapid test today, results in minutes.

People are also reading: Which STDs Are Most Affected by Medication Interference?
Testing for Eye STDs: What It Involves (And What It Doesn’t)
If you’re imagining a giant Q-tip jammed into your eyeball, don’t worry, it’s not that. Testing for ocular STDs can involve several approaches, and in many cases, the first clue actually comes from a standard STD panel. If a patient tests positive for chlamydia, gonorrhea, or herpes through oral or genital screening, doctors will often connect the dots if there are concurrent eye symptoms.
In more advanced settings, providers may do an ocular swab, a gentle swipe of the inside of the lower eyelid, to test for viral DNA or bacterial cultures. This is more common in ERs or ophthalmology clinics than in standard urgent care. For herpes, a fluorescein eye stain test might be used to detect corneal ulcers, a telltale sign of herpes keratitis. These tests are quick and relatively painless, but they depend on the provider knowing what to look for.
And that’s the rub. A lot of people never get tested for eye infections. They get treated blindly, antibiotics “just in case,” steroid drops that can actually worsen herpes, or nothing at all. Which means many ocular STD cases go unconfirmed and unreported. That’s a problem not just for your eyes, but for broader public health tracking too.
If you’re experiencing persistent eye issues, especially if you’ve recently had a hookup, made out with someone who had a “cold sore,” or received oral sex, don’t assume it’s seasonal allergies. Ask for a test. Better yet, start with an at-home kit and bring the results with you. You’ll be taken more seriously, and you’ll have a baseline to work from.
Check Your STD Status in Minutes
Test at Home with Remedium6-in-1 STD Test Kit

 For Men & Women
For Men & Women Results in Minutes
Results in Minutes No Lab Needed
No Lab Needed Private & Discreet
Private & DiscreetOrder Now $119.00 $294.00
For all 6 tests
What Happens If You Don’t Treat It?
Let’s be blunt: some eye STDs can cause irreversible vision loss. That doesn’t mean panic, it means action. Here’s what the research shows:
Ocular herpes can cause scarring of the cornea, leading to chronic blurred vision. Recurring outbreaks increase risk. A 2021 Lancet review found that untreated cases had a 30% higher chance of long-term visual impairment compared to those who received early antiviral treatment.
Ocular gonorrhea is uncommon but very dangerous. The bacteria can literally eat away at the eye's surface. If left untreated, permanent blindness is possible, sometimes in just a few days. Infections of the eyes with gonorrhea are considered a medical emergency and are treated aggressively with IV antibiotics and close monitoring.
Syphilitic uveitis can make you see floaters, hurt, and be sensitive to light. If not treated, it could lead to damage to the optic nerve, which cannot be fixed. A 2020 EyeNet clinical report said that finding problems early is the best way to keep your vision.
Even chlamydia, typically seen as “less severe,” can wreak havoc. Repeated exposure or untreated ocular chlamydia can lead to chronic conjunctivitis, scarring, and eyelid deformities in rare cases.
The takeaway isn’t “be afraid.” It’s “don’t brush this off.” If your eye symptoms are getting worse, or if they’re not responding to standard treatment, it’s time to look deeper. And in many cases, that means looking at your sexual health.
So... What Do You Do If This Is You?
First, breathe. Most ocular STDs are treatable. Antiviral medications like acyclovir can manage herpes outbreaks and reduce recurrence. Antibiotics like doxycycline or azithromycin can wipe out chlamydia or gonorrhea within days. Even syphilis responds well to early penicillin treatment when caught in time.
Second, get tested, fully. Not just for your eye. Not just for “one thing.” Get a comprehensive screen, including oral, genital, and rectal sites if applicable. Many people carry STDs in one location with no symptoms elsewhere. That means you could treat the eye but miss the source.
Third, if you’re sexually active, talk to your partners. This doesn’t mean shame. This means care. The same way you’d tell someone you had pink eye or strep throat, you can say, “Hey, I had something going on with my eye that turned out to be linked to HSV/chlamydia/etc. You might want to get checked too.”
And finally, don’t let this experience sour your relationship with your body, your sexuality, or your desires. You didn’t “do something wrong.” You didn’t get “punished” for sex. You encountered a virus or bacteria, the same way you’d catch a cold or stomach bug.
Testing is care, not shame, start today.
After the Infection: What Eye Care Looks Like
Healing from an ocular STD is both physical and emotional. Your eye may take days to weeks to fully recover, depending on the infection. Herpes, in particular, may become a chronic condition, manageable, but occasionally flaring up under stress or illness. You might use daily antivirals to prevent recurrences, especially if you’ve had multiple outbreaks in a year.
In more severe cases, like corneal scarring or repeated inflammation, you may be referred to an ophthalmologist for long-term management. That might include steroid drops, lubricants, or even surgical intervention, though that’s rare. The goal is always to preserve vision and prevent future damage.
But what often gets overlooked is the emotional recovery. People feel dirty, embarrassed, ashamed. Some avoid dating or sex altogether after an ocular STD diagnosis, worried someone will judge them or fear them. That isolation is unnecessary, and it’s cruel. Because what you’ve experienced is not a moral failing. It’s a medical condition.
Let’s say that again: This is not your fault. You are not dirty. You are not alone.

People are also reading: Can Men Get Yeast Infections from Their Partners? What You Need to Know
Prevention Doesn’t Mean Fear, It Means Freedom
So how do you prevent STDs in the eye without living in paranoia?
Start with the basics: hand hygiene after sex. It sounds silly, but it's one of the most effective strategies. If you’ve had oral contact or handled fluids, wash your hands before touching your eyes or face. Keep towels and washcloths separate, especially after a hookup or when someone has a cold sore.
If you’re in a new sexual relationship, or seeing multiple partners, regular testing becomes your anchor. An at-home combo STD test can screen for common infections discreetly and quickly, helping you stay ahead of symptoms that don’t show up in the usual places.
And maybe most importantly, communicate. Not everyone will know they’re shedding a virus. Not everyone will have visible symptoms. But by talking openly about testing, exposure, and comfort levels, you can create a safer sexual environment, for your eyes, your genitals, and everything in between.
Take control of your sexual health today.
When It’s Just a Virus, Not a Verdict
Here’s the truth: viruses don’t care who you are. They don’t care if you’re careful or careless, monogamous or open, gay or straight. They move between people through contact, sometimes invisible, sometimes unforgettable. And when they show up somewhere unexpected, like your eye, they can make you question everything.
But the truth is also this: you can have an ocular STD and still have a healthy sex life, a clear mind, and a deep sense of bodily trust. You are not broken. You are not gross. You are informed, empowered, and, hopefully, one step closer to peace of mind.
Don’t wait and wonder, get the clarity you deserve. This at-home combo test kit checks for the most common STDs discreetly and quickly.
FAQs
1. Wait, can you seriously get an STD in your eye?
Yeah, it’s a thing, and it’s more common than most people realize. Infections like herpes, chlamydia, gonorrhea, and even syphilis can find their way into the eye through fluids, fingers, or oral contact. Your eye is a mucous membrane, just like genitals and mouths. Viruses don’t care about geography.
2. How would I even know it’s an STD and not just pink eye?
Great question, and not an easy one. The early symptoms can look identical: redness, discharge, irritation. But if it’s an STD, it’s often more intense. We’re talking light sensitivity, a deep ache, maybe blurry vision or even recurring flare-ups. If it feels like pink eye on steroids, it’s worth getting checked.
3. I haven’t had sex in months, how could I have this?
Because “sex” isn’t just penis-in-vagina or even genitals-only. If you kissed someone with a cold sore or received oral from someone shedding HSV or chlamydia, you could’ve picked it up. These things don’t come with a warning label. One steamy hookup, one shared towel, one forgetful eye rub, and boom.
4. Can I get herpes in my eye from kissing someone?
Yep. If they have oral herpes, even without a visible sore, and you kiss them or share saliva (hello, oral sex or even sharing drinks), that virus can transfer. Rub your eye after that? That’s all it takes. It sounds wild, but it’s medically documented and not even rare.
5. What does eye herpes even feel like?
Imagine your eye feels gritty, almost like there’s sand in it. Then it starts watering, turns red, maybe gets crusty in the morning. You might be sensitive to light, and the vision in that eye gets a little fuzzy. Some people feel a stabbing sensation or a weird “pulse” behind the eye. If it comes and goes? Big herpes red flag.
6. Will a normal STD test tell me if it’s in my eye?
Not always, but it’s a good place to start. If your test shows chlamydia or herpes, and you also have eye symptoms, doctors are more likely to take it seriously and test your eye directly. Otherwise, they may just hand you eye drops and send you home. So start with a full-panel test, it gives you leverage.
7. Can I go blind from this?
In extreme, untreated cases, yes. But that’s not your future if you act early. Herpes can scar the cornea over time. Gonorrhea can do damage fast if it gets aggressive. The good news? Most people who get diagnosed and treated promptly recover fully. Don’t let fear freeze you, use it to move.
8. Okay, so how do they test for it?
If you’re lucky, they’ll swab the inside of your lower eyelid for viral DNA or bacterial cultures. If you're not lucky, they’ll misdiagnose you and you’ll be stuck playing medical pinball. Pro tip: get an at-home test first to confirm exposure, then push for an eye-specific exam with those results in hand.
9. What if I already used antibiotic drops and nothing changed?
That’s a classic sign it’s viral, not bacterial. Most eye STDs, like herpes, laugh in the face of antibiotics. If your symptoms aren't budging after 3–5 days on drops, go back. Say the word “herpes” out loud. Say “recent contact.” Say “I want to rule out an STD.” That flips the script.
10. Can I still kiss or hook up after this?
Yes, but wait until the symptoms are totally gone and you’ve been cleared, or completed treatment if it’s bacterial. Herpes especially can still shed virus even when your eye feels fine, so talk to your provider about antiviral meds if needed. And remember: this doesn’t make you untouchable. It makes you informed.
You Deserve Answers, Not Assumptions
It’s scary when something feels wrong with your body, especially in a place like your eye, where you’re not expecting anything sexual to show up. But your symptoms don’t define you. Your past encounters don’t determine your worth. What matters is what you do next.
STD-related eye infections are real. They’re underdiagnosed. And they’re treatable. Whether you're dealing with cloudy vision, crusty eyelids, or just that nagging gut feeling that something's off, trust yourself. Ask the hard questions. Get tested. And know that you're not alone in this.
Don’t wait and wonder, get the clarity you deserve. This at-home combo test kit checks for the most common STDs discreetly and quickly.
Sources
1. Herpes Keratitis - American Academy of Ophthalmology
2. Global Burden of Ocular Herpes - Journal of Ophthalmology
3. Syphilitic Uveitis - EyeNet Clinical Update